Evaluation of the Efficiency of the Nursing Care
Plan Applied Using NANDA, NOC, and NIC
Linkages to Elderly Women with Incontinence
Living in a Nursing Home: A Randomized
Controlled Study
Dercan Gencbas, RN, PhD, Assistant Professor , Hatice Bebis, RN, PhD, Associate Professor, and Hatice Cicek, RN, PhD, Associate Professor
Atilim University, Faculty of Health Sciences, Department of Nursing, Ankara, Turkey, Gulhane School of Nursing, Health Science University, Ankara, Turkey, and Nursing High School, Girne American University, Girne, Cyprus
PURPOSE: Evaluate the efficiency of the nursing care plan, applied with the use of
NANDA-I, NOC, and NIC (NNN) linkages, for elderly women with incontinence who live in nursing homes.
METHODS: A randomized controlled experimental design was applied. NNN
link-ages were prepared and applied for 12 weeks in an experimental group. NOC scales were evaluated again for two groups.
RESULTS: A 0.5 NOC point change targeted in all elderly in the experimental group
were provided between pretest–posttest scores. The experimental group had higher life quality and lower incontinence severity/symptoms than the control group.
CONCLUSION: It is important that NNN linkages effective for solving the problems
are used in different groups and with larger samples to create further evidence linking NNN. Search terms: elderly, incontinence, NANDA/NOC/NIC, NNN linkages, nursing Author contact:
dgencbas@gmail.com, with a copy to the Editor: journal@nanda.org
Efforts to improve the quality of nursing care and support professional practices are ongoing (Kautz & Van Horn, 2008). The American Nursing Association (ANA) has ap-proved the use of Standard Nursing Languages (SNLs) for nurses in their field of work to increase evidence-based nurs-ing care. Use of SNLs improves efficient decision-maknurs-ing and critical thinking in the nursing process. It was reported that NANDA-I, Nursing Outcomes Classification (NOC), and Nursing Intervention Classification (NIC) are the most com-monly used SNLs (ANA, 2015; Tastan et al., 2014). During the nursing process, the existing problem of an individual is identified with NANDA-I, while the seriousness of the problem and targets to be achieved after care are identified with the NOC. The NIC includes nursing interventions that will guide nurses. Creating and using NANDA-I, NOC, and NIC linkages (NNN) appropriate for an individual’s illness/health condition enables providing of a holistic nursing care (John-son et al., 2012). NNN linkages are used not only in hospitals but also in nurseries, schools, home care centers, and reha-bilitation centers, as well as by different health professionals (Johnson et al., 2012). Although many studies have used
NANDA-I, NOC, and NIC systems extensively, only few have assessed NNN linkages (Azzolin et al., 2013; Kautz & Van Horn, 2008; Tastan et al., 2014).
When the literature is examined, the prevalence of uri-nary incontinence (UI) in elderly individuals is higher in the nursing home, ranging from 30 to 77% (Abrams et al., 2002; Ayeleke, Hay-Smith, & Omar, 2013). Additionally, no stan-dardized, comprehensive nursing care study using NNN link-ages has been found (Vinsnes et al., 2012). For the compre-hensive nursing care of the elderly with UI, it is important to develop and implement a complex nursing care plan that includes practices such as bladder training, urine output con-trol, pelvic muscle exercises, infection concon-trol, and evalua-tion of the intervenevalua-tion results (Angelica et al., 2013). The nurse can clinically observe, scientifically assess patients and provide national and international comparative care with UI-specific NNN linkages. (Bitencourt, Alves, Santana, & Lopes, 2015; Brito-Brito et al., 2014; Johnson et al., 2012).
The aim of this study was to assess the effectiveness of the nursing care plan implemented using NNN linkages for el-derly women with incontinence and living in nursing homes.
Methods
Study Design and Sample
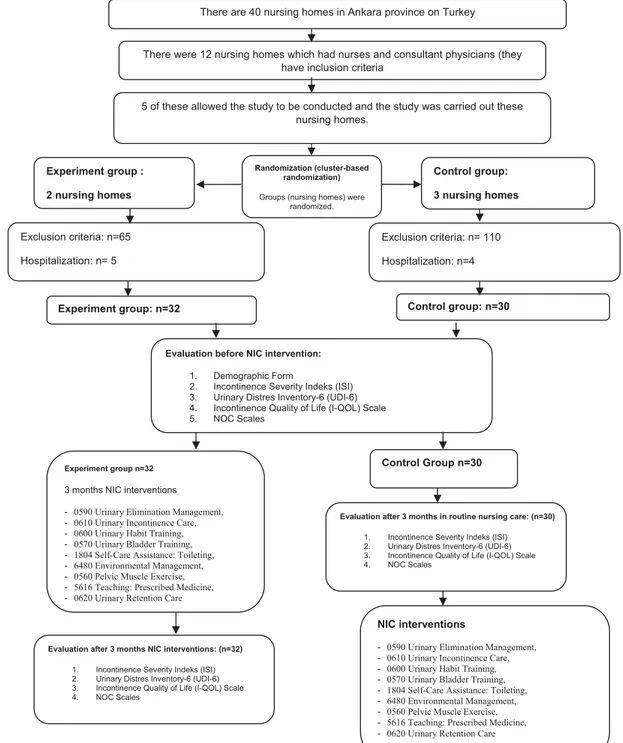
The experimental design with randomized control was used in this study. There are 40 nursing homes in Ankara province in Turkey. There are 12 nursing homes that have nurses and consultant physicians. Five of these allowed the study to be conducted.
Randomization
In this study, individual randomization may lead to a bias because elderly women with UI assigned to the experimen-tal and control groups live in the same nursing home and in-teract with each other. Therefore, cluster-based randomiza-tion has been used in nursing homes (Rosenberger & Lachin, 2002). Two of these five nursing homes were assigned to the experimental group and three to the control group using the withdrawal method.
The sample size of the study was calculated such that there were at least 22 people in each group according to a clinic effect size of 0.5 points on the pre–post NOC scale points, an alpha of 0.05, and a power of 0.80 (Azzolin et al., 2013; Kashanian, Ali, Nazemi, & Bahasadri, 2011; Lee, Park, Nam, & Whyte, 2011).
In the five nursing homes where 249 elderly women lived, dementia or Alzheimer’s communication problems and UI were identified by the institutional nurse and researchers. El-derly women whose minimental test result was 23 and more and those who accepted participation in the study were in-cluded in the study. Sixty-two elderly women with UI were included in the study, 32 in the experimental group and 30 in the control group. The elderly women were subjected to questionnaires after obtaining their verbal consent.
Ethical Procedures
Prior to the study, ethical board permission was received from the Gulhane Military Medical Academy Ethical Board and institutional permission was received from the nursing homes.
Instruments
NNN linkages guideline. In this study, personal nursing
care plans were created with NANDA I, NOC, and NIC link-ages related to UI using the NNN linklink-ages book as a guide (Johnson et al., 2012). The NNN linkages related to UI in this book have been translated into Turkish by five nurses who have a good level of English knowledge and are specialists in their fields. As a result of the evaluation of the expert opinions, Content Validity Index values of the forms were found to be between 0.82 and 0.91.
NANDA-I. In the study, six NANDA-I diagnoses out of
nine UI-related NANDA-I nursing diagnoses, which belonged
“Domain 3: Elimination and Exchange” (NANDA-I has do-mains, classes and diagnoses), were used (Herdman & Kamitsuru, 2014).
NOC. NOC scales are five Likert-type scales. All of the
scales are expressed as least desirable (1) to most desirable (5) (1= never, 5 = always can/1 = severe, 5 = none/1 = with serious risk, 5= no risk). The scales are evaluated based on the total score average. Each scale is evaluated within itself, and it can be used in special, different numbers and types unique to each individual (Moorhead, Johnson, Mass, & Swanson, 2012). In this study, all five NOC scales (“0502 Urinary Continence,” “1101 Tissue Integrity: Skin and Mucous Membranes,” “0310 Self-care Toileting,” and “Medication Response”) recommended in the guidelines specific to the selected NANDA-I were used.
NIC. For the solution of the problems of elderly women
with UI in the study, nine NIC attempts specific to NANDA-I di-agnoses and chosen according to NOCs (“0590 Urinary Elim-ination Management,” “0610 Urinary Incontinence Care,” “0600 Urinary Habit Training,” “0570 Urinary Bladder Train-ing,” “1804 Self-Care Assistance: ToiletTrain-ing,” “6480 Environ-mental Management,” “0560 Pelvic Muscle Exercise,” “5616 Teaching: Prescribed Medicine,” and “0620 Urinary Reten-tion Care”) were applied (Bulechek, Butcher, Dochterman, & Wagner, 2012).
Incontinence severity index. The Incontinence
Sever-ity Index (ISI) was developed by Sandvik, Hunskaar, Seim, Hermstad, Vanvik, and Bratt (1993) by applying it to women with incontinence. Hazar et al. (2008) carried out Turkish va-lidity and reliability. In this study, Cronbach’s alpha was .84. It has two questions concerning the frequency and amount of urine. The score is obtained by multiplying the score in the first question with that in the second question. A score of 1–2 represents slight UI, 3–6 moderate UI, 8–9 severe UI, and 12 very strong UI.
Urinary distress inventory-6. The Urinary Distress
Inventory-6 (UDI-6) scale was developed by Shumaker, Wyman, Uebersax, McClish, and Fantl (1994) with 19 ques-tions. Subsequently, Uebersax, Wyman, Shumaker, and Mc-Clish (1995) reduced the number of questions to six and studied the validity and reliability. Cam, Sakallı, Ay, Cam, and Karateke (2007) carried out the Turkish validity of this short form. In this study, Cronbach’s alpha was .78. The UDI-6 scale evaluates the disorder associated with urinary symptoms and its degree. The degree of the disorder was marked on the Likert-type scale as follows: 0= none, 1 = slight, 2 = moderate, and 3= serious. A maximum score of 18 and a minimum score of 0 were obtained from the scale.
Incontinence quality of life scale. The Incontinence
Quality of Life (I-QQL) scale was developed by Wagner, Patrick, Bavendam, Martin, and Buesching (1996) to assess
the impact of incontinence on the quality of life. However, the scale was revised by Patrick et al. in 1999. In this study, Cronbach’s alpha was .96. In the I-QQL scale, all items were evaluated using the six-category Likert-type scale (1= very, 6= none), and they were converted into scale value rang-ing from 0 to 132 for the calculated total score. A high score indicates good quality of life.
Intervention Procedure
Before the intervention, the health staff at the nursing homes were given a conference on “incontinence nursing care education.” During the period of 1 week, the researchers and nursing home health staff observed all the elderly with UI and recorded their observations in bladder diaries.
According to the results obtained from the 1-week bladder records and data collection forms, individual-specific Nurs-ing Care Plans were prepared usNurs-ing NNN linkages for the elderly with UI in the experimental group (Johnson et al., 2012). In accordance with the incontinence type and re-quirement for each elderly individual, one or more than one NANDA-I diagnoses were chosen. Thereafter, each NANDA-I diagnosis was measured using the appropriate NOC and value (1–5), indicating that the current status of the elderly with UI was obtained. To solve the incontinence-related prob-lem of the elderly, prevent complications, and treat the cur-rent status of UI, the expected/required NOC target in the el-derly with UI was determined. To achieve the specified NOC goals, NIC attempts were selected and implemented by the nurse for 12 weeks. No attempt was made with the control group, which continued with routine practices in this pro-cess. After 12 weeks, the NOC and other scales were applied to the experimental and control groups again to measure whether the target NOC scores were achieved (Figure 1).
Data Analysis
The SPSS 15.0 package program was used in the study. De-scriptive statistical analyses were performed for sociodemo-graphic and incontinence-related features. In terms of these features, chi-squared test was used for consecutive data and Mann–Whitney U-test was used for continuous data to de-termine whether there was a significant difference between the experimental and control groups. Student t-tests were used for those with normal distribution and Mann–Whitney U-test was used for those without normal distribution in the independent groups to determine whether there was a sig-nificant difference between the experimental and control groups in terms of the ISI, UDI-6, and I-QOL scale point av-erages. The Wilcoxon test was used for nonresponders in groups with normal distribution to compare the pretest and posttest results.
Findings
We found that 43.8% of the experimental group and 53.3% of the control group were in the 75–85-year age
group. Additionally, 56.3% of the experimental group and 36.7% of the control group were found to be overweight. In both groups, only five persons gave birth to infants over 4,000 g, and 71.9% of the experimental group and 83.3% of the control group had normal births. Moreover, 93.8% of the experimental group and 80% of the control group had at least one chronic illness. The elderly using anticholinergic drugs covered 21.9% of the experimental group and 6.7% of the control group.
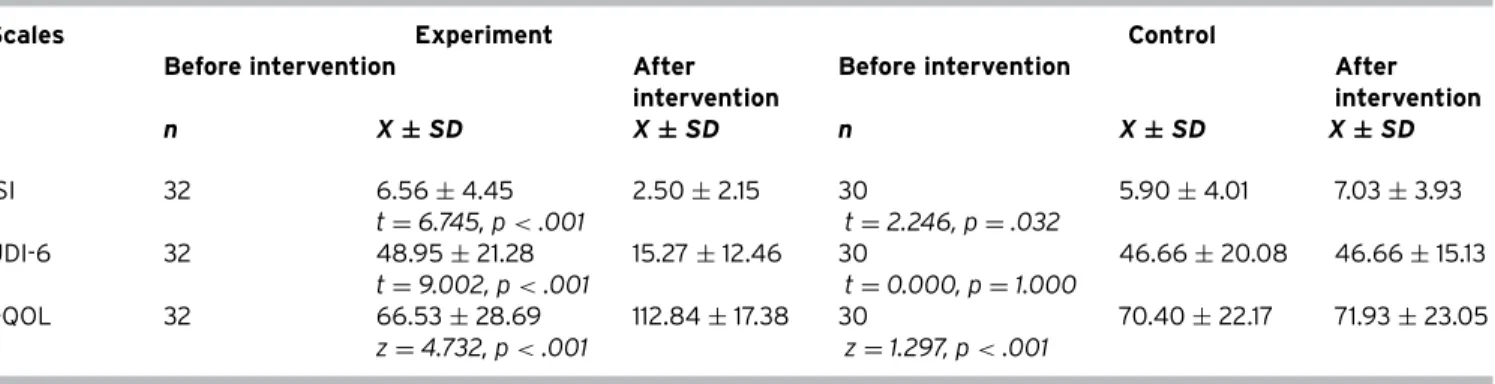
The experimental and control group received minimum 1 point and maximum 12 points for the ISI scores. However, the highest UDI-6 score in the experimental group was 88.89, while that in the control group was found to be 100. The I-QOL scale score for the experimental group and the control group was 66.53± 28.69 and 70.40 ± 22.17, respectively (Table 1). No statistically significant difference was found in favor of the control group in comparison with the experimen-tal group in terms of the sociodemographic characteristics except for educational factors that might be associated with incontinence, ISI, UDI-6, and I-QOL scale averages (p> .05).
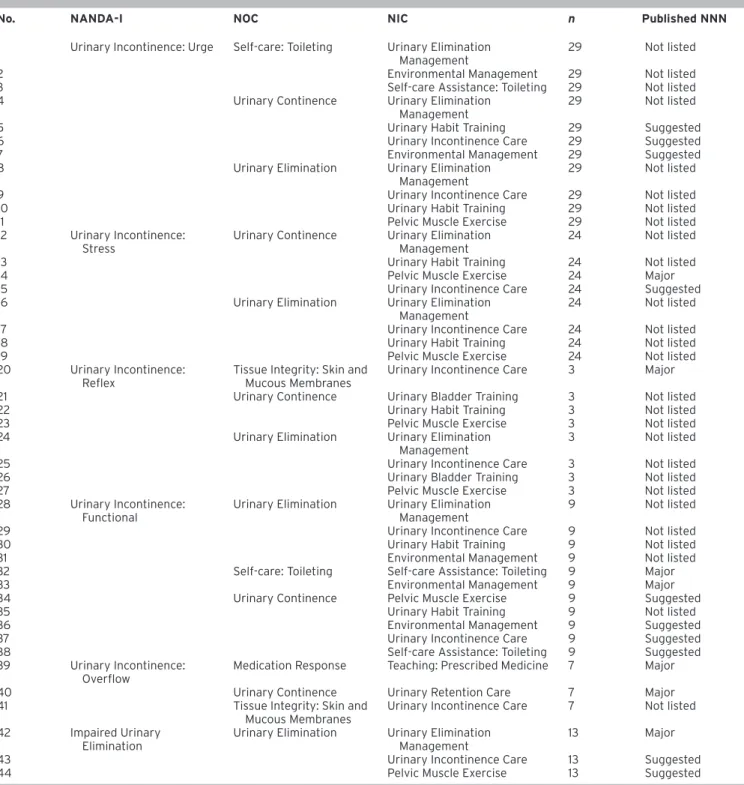
Selected NANDA-I Diagnoses, NOC Outcomes, and NIC Interventions
In this study, “00019 Urge Incontinence” was selected the most, and “00018 Reflex Incontinence” was selected the least. NANDA-I diagnosis was selected. In the experimental group, an average of 2.63± 1.15 NANDA-I diagnoses was se-lected; in the control group, 2.93± 1.01 NANDA-I diagnoses were selected (p> .05).
In this study, while “0502 Urinary Continence” and “0503 Urinary Elimination” NOCs were used for all the elderly with UI in both the experimental and control groups, the least used NOC was “2301 Medication Response.” The experimen-tal group was evaluated with a mean of 3.37± 0.83 NOC scales, and the control group was evaluated with 3.76± 1.07 NOC scales (p> .05).
The most applied NICs were “0590 Urinary Elimina-tion Management,” “0610 Urinary Incontinence Care,” and “0560 Pelvic Muscle Exercise,” and they were implemented in all of the elderly. “5616 Teaching: Prescribed Medication,” “0620 Urinary Retention,” and “0570 Urinary Bladder Train-ing” NICs were the least applied NICs, implemented in seven elderly individuals. In the experimental group, the average number of applied NICs per person was 6.43± 1.16.
Effect of NIC Interventions on NOC Outcomes
Table 2 indicates the variations in the NOC scores of each NIC activities applied to the experimental group af-ter the inaf-tervention. Afaf-ter all NIC activities had been imple-mented, the expected change in the NOC scores was found to be above 0.5 points. In this study, nine different NIC activities for the NANDA-I diagnoses were performed in el-derly women with UI (there were 192 total NIC activities in
Figure 1. Study Design
There were 12 nursing homes which had nurses and consultant physicians (they have inclusion criteria
Control group: 3 nursing homes Exclusion criteria: n= 110 Hospitalization: n=4 Experiment group : 2 nursing homes
Evaluation before NIC intervention:
1. Demographic Form 2. Incontinence Severity Indeks (ISI) 3. Urinary Distres Inventory-6 (UDI-6) 4. Incontinence Quality of Life (I-QOL) Scale 5. NOC Scales
Exclusion criteria: n=65 Hospitalization: n= 5
Randomization (cluster-based randomization)
Groups (nursing homes) were randomized.
Experiment group n=32
3 months NIC interventions - 0590 Urinary Elimination Management, - 0610 Urinary Incontinence Care, - 0600 Urinary Habit Training, - 0570 Urinary Bladder Training, - 1804 Self-Care Assistance: Toileting, - 6480 Environmental Management, - 0560 Pelvic Muscle Exercise, - 5616 Teaching: Prescribed Medicine, - 0620 Urinary Retention Care
Evaluation after 3 months NIC interventions: (n=32)
1. Incontinence Severity Indeks (ISI) 2. Urinary Distres Inventory-6 (UDI-6) 3. Incontinence Quality of Life (I-QOL) Scale 4. NOC Scales
Evaluation after 3 months in routine nursing care: (n=30)
1. Incontinence Severity Indeks (ISI) 2. Urinary Distres Inventory-6 (UDI-6) 3. Incontinence Quality of Life (I-QOL) Scale 4. NOC Scales
NIC interventions
- 0590 Urinary Elimination Management, - 0610 Urinary Incontinence Care, - 0600 Urinary Habit Training, - 0570 Urinary Bladder Training, - 1804 Self-Care Assistance: Toileting, - 6480 Environmental Management, - 0560 Pelvic Muscle Exercise, - 5616 Teaching: Prescribed Medicine, - 0620 Urinary Retention Care
Control group: n=30 Experiment group: n=32
Control Group n=30
5 of these allowed the study to be conducted and the study was carried out these nursing homes.
There are 40 nursing homes in Ankara province on Turkey
the guide, at least 72 and mostly 131 NIC activities were used in this study).
Following NIC interventions, when changes in the NOC scores of the experimental group were compared with the previous results prior to the intervention, the highest change was found to be in the “Urinary Continence” NOC (1.48 points); after the “0570 Urinary Bladder Training” NIC
attempt, the least change was observed in the “2301 Medica-tion Response” (0.79 points) NOC after the “5616 Teaching: Prescribed Medicine” NIC intervention. In the control group, the “0503 Urinary Elimination” (–0.13) and “0310 Self-care: Toileting” (–0.06) NOC scores decreased after 3 months, and “2301 Medication Response” NOC scores did not change (p< .05) (Table 3).
Table 1. ISI, UDI-6, and I-QOL Scores of Experimental and Control Groups
Experiment Control
Mean± SD Mean± SD t p*
I-QOL 66.53± 28.69 70.40± 22.17 0.591 .55
Median Min–max Median Min–max z p*
ISI 4 1–12 5 1–12 −0.558 .57
UDI-6 44.44 11.11–88.89 41.66 16.67–100.00 −0.688 .49
t: t test for independent samples. z: Mann–Whitney U-test.
*p< .05 was considered significant.
NNN Linkages Used in Elderly Women with UI
In this study, 44 total NNN connections were used in the nursing care plans of the elderly with UI in the experimen-tal group (Table 4). In the guide, there are 106 NNN connec-tions for the six NANDA-I diagnoses used in the study. In this research, 7 major NNN linkages and 10 suggested NNN link-ages were used. In addition, 27 new NNN links, which were not in the guidelines, were created and used in this study for the elderly women with UI. These new NNN connections used in the study accounted for 61% of the intervention. However, in this study, no classification was made as a re-quired/recommended attempt for newly created NNN con-nections.
Relationship between the NOC and the ISI, UDI-6, and I-QOL
The impact of the nursing care provided for the elderly with UI was evaluated using the ISI, UDI-6, and I-QOL scale scores besides the NOC scale scores. There were statistical differences between pretest and posttest scores in the con-trol group, but these differences are not significant for prac-tice (Table 5). Furthermore, a positive statistical significance was found between the UDI-6, I-QOL, “0502 Urinary Inconti-nence,” “0503 Urinary Elimination,” “1101 Tissue Integrity: Skin and Mucous Membranes,” and “0310 Self-Care” NOC scales (p< .05), except for the “2301 Drug Response” NOC scale average scores (p> .05) before and after intervention in the experimental group.
Discussion
In this study, the nursing care plan using NNN linkages was applied to elderly women with UI living in nursing homes, and its effectiveness was assessed. No statistically signifi-cant difference was found between the two groups in terms of the sociodemographic characteristics, factors that might be related to incontinence, and ISI, UDI-6, and I-QOL scale point scores.
NANDA-I
In this study, regarding UI, six of the nine NANDA-I nursing diagnoses (2.63± 1.15 in the experimental group, 2.93± 1.01 in the control group) recommended using the NNN linkage guide. In the guide, each NANDA-I diagnosis was defined, and its etiology was supported with literature (Herdman & Kamitsuru, 2014). In this study, similar to the lit-erature, elderly women showed more urge incontinence and stress-type incontinence and less reflex type incontinence nursing diagnosis (Thüroff et al., 2011; Palese & Carniel, 2011). Nurses with different levels of education and experience who provide care for elderly women with UI evaluate the elderly with UI in terms of incontinence. NANDA-I is a guide in the selection of the nursing diagnosis.
NOC
Nurses assess the situation of patients/individuals with NOC, detect the severity and degree of the problem, and plan their initiatives accordingly. With the NOC scales, the nurse can evaluate the change not only in the amount of urine, incontinence frequency, and duration but also in self-care skills and compliance with medicine (Moorhead et al., 2012). Lin (2013) emphasizes that urinary excretion (urine excretion rate, urine color, odor, fluid intake, dysuria, pres-ence of nocturia) should be assessed for the elderly with incontinence to identify the severity of the problem. In this study, the “0503 Urinary Elimination” NOC scale was used, and all elderly with UI were evaluated in terms of urine rou-tine, urine color, odor, retention, and nocturia status. Thus, the nurse could make the right decision because he or she could evaluate the urinary excretion routine, infection sta-tus, and urinary incontinence level.
Studies have indicated that it is necessary to evaluate in-dividuals in terms of recognizing the need for urination and going to the toilet without any help, changing clothes, and fluid intake status (Al-Samarrai, Uman, Al-Samarrai, & Alessi, 2007; Lewicky-Gaupp et al., 2008; Klay & Marfyak, 2005). In this study, all of these characteristics of women with UI were evaluated with the “0502 Urinary Continence” NOC, and it is
Table 2. Changes in NOC Scores According to Participant NIC Interventions in the Experimental Group
NIC NOC n X ± SD Min Max Difference*
0570 Urinary Bladder Training
Urinary Continence Pretest 7 2.93± 3.72 2.47 3.52 1.48 Posttest 7 4.41± 0.24 3.88 4.64
Urinary Elimination Pretest 7 3.04± 0.41 2.27 3.52 1.45 Posttest 7 4.49± 0.22 4.19 4.71
0590 Urinary Elimination Management
Self-care: Toileting Pretest 32 3.01± 1.09 0.00 4.12 1.07 Posttest 32 4.08± 1.41 0.00 5.00
Urinary Continence Pretest 32 3.24± 0.44 2.47 4.11 1.2 Posttest 32 4.44± 0.37 3.25 4.88
Urinary Elimination Pretest 32 3.23± 0.46 2.10 4.21 1.36 Posttest 32 4.59± 0.22 4.19 5.00
0600 Urinary Habit Training
Urinary Continence Pretest 31 3.24± 0.45 2.47 4.11 1.21 Posttest 31 4.45± 0.37 3.25 4.88
Urinary Elimination Pretest 31 3.22± 0.46 2.10 4.21 1.36 Posttest 31 4.58± 0.22 4.19 5.00
1804 Self-care Assistance: Toileting
Self-care: Toileting Pretest 29 3.32± 0.49 2.18 4.12 1.18 Posttest 29 4.50± 0.49 3.08 5.00
Urinary Continence Pretest 29 3.20± 0.44 2.47 4.11 1.23 Posttest 29 4.43± 0.37 3.25 4.82
6480 Environmental Management
Self-care: Toileting Pretest 29 3.32± 0.49 2.18 4.12 1.18 Posttest 29 4.50± 0.49 3.08 5.00
Urinary Continence Pretest 29 3.20± 0.44 2.47 4.11 1.23 Posttest 29 4.43± 0.37 3.25 4.82
Urinary Elimination Pretest 29 3.17± 0.44 2.10 4.21 1.4 Posttest 29 4.57± 0.22 4.19 5.00
0560 Pelvic Muscle Exercise
Urinary Continence Pretest 32 3.24± 0.44 2.47 4.11 1.2 Posttest 32 4.44± 0.37 3.25 4.88
Urinary Elimination Pretest 32 3.23± 0.46 2.10 4.21 1.36 Posttest 32 4.59± 0.22 4.19 5.00
0610 Urinary Incontinence Care
Urinary Continence Pretest 32 3.24± 0.44 2.47 4.11 1.2 Posttest 32 4.44± 0.37 3.25 4.88
Urinary Elimination Pretest 32 3.23± 0.46 2.10 4.21 1.36 Posttest 32 4.59± 0.22 4.19 5.00
Tissue Integrity: Skin and Mucous Membranes
Pretest 32 4.10± 0.75 2.69 4.88 0.83 Posttest 32 4.93± 0.06 4.84 5.00
5616 Teaching: Prescribed Medicine
Medication Response Pretest 7 4.19± 0.81 2.85 5.00 0.70 Posttest 7 4.89± 0.90 4.50 5.00
0620 Urinary Retention Care
Urinary Continence Pretest 7 3.12± 0.26 2.72 3.41 1.36 Posttest 7 4.48± 0.21 4.15 4.82
*0.5 increments presupposition.
believed that nurses will evaluate the patients in a compre-hensive way with this NOC as specified in the literature.
Lewicky-Gaupp et al. (2008) also emphasize the need to assess the relationship between incontinence and the self-care status in older adults with UI. In this sense, the el-derly women with UI who participated in the study were evaluated in terms of their ability to react to urination feel-ing, removing their clothes before urination, and maintain-ing their hygiene after urination usmaintain-ing the “0310 Self-care: Toileting” NOC.
Similar to that in the study carried out by Beeckman, Verhaeghe, Defloor, Schoonhoven, and Vanderwee (2011) for the elderly with incontinence, urinary skin assessment was performed using the “1101 Tissue Integrity: Skin & Mucous Membranes” NOC as the elderly with UI frequently used medical pads in this study as well. In the literature, it is emphasized that pharmacological treatments and their effects should be evaluated (Burgio et al., 1998). In this
study, the pharmacological treatments of seven elderly individuals and effects of incontinence were evaluated using the “Medication Response” NOC.
NIC
In the meta-analysis study of nursing practice in individ-uals with UI, it was found that pelvic muscle exercises with other therapies were effective in the treatment of inconti-nence in a long term (bladder training, biofeedback, vaginal cone, intravaginal electrical stimulation, and psychotherapy) (Moroni, Magnani, Haddad, de Aquino Castro, & Brito, 2016). In this study, researchers conducted at least four and at most nine NIC (mean 6.43± 1.16) interventions for each elderly individual to solve the incontinence problem in them. For example, the “0590 Urinary Elimination Management” NIC helped the elderly to go to the toilet and those with signs of
Table 3. Changes in the Average NOC Points of the Experiment and Control Group before and after the Intervention
NOC Experiment before
NIC intervention
Control after NIC intervention Change between experiment–control group z* p* 0503 Urinary Elimination 1.36 −0.13 1.49 6.51 .001 0310 Self-care: Toileting 1.18 −0.06 1.24 5.32 .001 0502 Urinary Continence 1.20 0.05 1.15 6.03 .001 1101 Tissue Integrity: Skin and Mucous Membranes 0.83 0.09 0.74 3.92 .001 2301 Medication Response 0.70 0.0 0.70 2.88 .004 *Mann–Whitney U-test.
*p< .05 was considered significant.
infections were monitored for fluid intake; additionally, uri-nary retention was triggered with water sound. Therefore, it would be easy to adjust the episodes. In parallel with the literature, with this NIC, multiple nursing care techniques are provided to adjust the incontinence status of the elderly (Tanaka et al., 2009). With the “5616 Teaching: Prescribed Medication” NIC, the knowledge level of the elderly was in-creased and impacts of the medicine and interaction of the drugs with each other were taught. In the literature, it was emphasized that it is important to increase the knowledge level of drug management for the elderly (Kane & Xu, 2013). NIC interventions can be employed separately or together in accordance with the needs of the elderly and circum-stances. Additionally, NIC will enable the nurse to apply the initiatives specified in the literature in a more standard and systematic way and based on evidence.
Change in the NOC Score Averages after NIC Intervention
The effectiveness of the NICs applied in the study was measured by the NOCs. Change was mostly found in the “0502 Urinary Continence” and “0503 Urinary Elimination” NOC scores (1.48 and 1.45 points, respectively) after the “0570 Urinary Bladder Training” NIC intervention. In the literature, toilet program/bladder education has been re-ported as an effective method to improve the urinary con-tinence level and excretion order of the individual and is ap-plied by the nurses (Albers-Heitner et al., 2011; Yoon, Song, & Ro, 2003).
In the study, the effectiveness of the “0590 Urinary Elim-ination Management” NIC intervention was evaluated with the “0310 Self-care: Toileting,” “0502 Urinary Continence,” and “0503 Urinary Elimination” NOCs, and positive changes were observed in NOC scores (1.07, 1.2, and 1.3 points, respec-tively). Similar to these findings in the literature, improve-ments in the self-care status and urination routine have
been observed after urine removal procedure of the elderly with incontinence (Bitencourt et al., 2015; Borrie, Bawden, Speechley, & Kloseck, 2002; Klutke et al., 2009).
In this study, like the “0590 Urinary Elimination Manage-ment” NIC, “0600 Urinary Habit Training,” “0610 Urinary Incontinence Care,” “1804 Self-care Assistance: Toileting,” “0560 Pelvic Muscle Exercise,” “0620 Urinary Retention Care,” and “5616 Teaching: Prescribed Medicine” NIC inter-ventions were evaluated using various NOCs. As a result of the interventions, all the NOCs showed an expected change greater than 0.05 points. This situation demonstrates that nurses can positively change UI outcomes by providing a standard and regular toilet program, pelvic muscle exercise, and urinal retention care for elderly women and increasing their urinary medication knowledge and enabling their self-care process.
NNN Linkages
Nurses can perform objective and comprehensive care at every stage of the nursing process with recommended NNN linkages and evaluate the resulting outcomes ob-jectively with the NOCs. Therefore, they can monitor the development in the elderly with UI for whom they provide care and can make a self-evaluation about whether her choices are right and whether the interventions are suffi-cient. Twenty-seven of 44 NNN linkages used in this study have been recently developed, and positive care results were collected. These NNN linkages may lead and provide evi-dence regarding the nurses. The nurses can also create new NNN linkages.
ISI, UDI-6, and I-QOL
In this study, a statistically significant and positive differ-ence was found in terms of the ISI, UDI-6, and I-QOL scale scores of the elderly in the experimental group before and
Table 4. Comparison of NNN Linkages According to the NANDA-I Nursing Diagnoses with Published NNN Linkages
No. NANDA-I NOC NIC n Published NNN
1 Urinary Incontinence: Urge Self-care: Toileting Urinary Elimination Management
29 Not listed
2 Environmental Management 29 Not listed
3 Self-care Assistance: Toileting 29 Not listed
4 Urinary Continence Urinary Elimination
Management
29 Not listed
5 Urinary Habit Training 29 Suggested
6 Urinary Incontinence Care 29 Suggested
7 Environmental Management 29 Suggested
8 Urinary Elimination Urinary Elimination
Management
29 Not listed
9 Urinary Incontinence Care 29 Not listed
10 Urinary Habit Training 29 Not listed
11 Pelvic Muscle Exercise 29 Not listed
12 Urinary Incontinence: Stress
Urinary Continence Urinary Elimination Management
24 Not listed
13 Urinary Habit Training 24 Not listed
14 Pelvic Muscle Exercise 24 Major
15 Urinary Incontinence Care 24 Suggested
16 Urinary Elimination Urinary Elimination
Management
24 Not listed
17 Urinary Incontinence Care 24 Not listed
18 Urinary Habit Training 24 Not listed
19 Pelvic Muscle Exercise 24 Not listed
20 Urinary Incontinence: Reflex
Tissue Integrity: Skin and Mucous Membranes
Urinary Incontinence Care 3 Major
21 Urinary Continence Urinary Bladder Training 3 Not listed
22 Urinary Habit Training 3 Not listed
23 Pelvic Muscle Exercise 3 Not listed
24 Urinary Elimination Urinary Elimination
Management
3 Not listed
25 Urinary Incontinence Care 3 Not listed
26 Urinary Bladder Training 3 Not listed
27 Pelvic Muscle Exercise 3 Not listed
28 Urinary Incontinence: Functional
Urinary Elimination Urinary Elimination Management
9 Not listed
29 Urinary Incontinence Care 9 Not listed
30 Urinary Habit Training 9 Not listed
31 Environmental Management 9 Not listed
32 Self-care: Toileting Self-care Assistance: Toileting 9 Major
33 Environmental Management 9 Major
34 Urinary Continence Pelvic Muscle Exercise 9 Suggested
35 Urinary Habit Training 9 Not listed
36 Environmental Management 9 Suggested
37 Urinary Incontinence Care 9 Suggested
38 Self-care Assistance: Toileting 9 Suggested
39 Urinary Incontinence: Overflow
Medication Response Teaching: Prescribed Medicine 7 Major
40 Urinary Continence Urinary Retention Care 7 Major
41 Tissue Integrity: Skin and
Mucous Membranes
Urinary Incontinence Care 7 Not listed 42 Impaired Urinary
Elimination
Urinary Elimination Urinary Elimination Management
13 Major
43 Urinary Incontinence Care 13 Suggested
44 Pelvic Muscle Exercise 13 Suggested
after the intervention. In the literature, an increase is ob-served in the I-QQL scores after the nursing interventions and in the welfare level of the elderly particularly related to incontinence (Kashanian et al., 2011; Zimmern, Litman,
Mueller, Norton, & Goode, 2010). Therefore, the NIC interven-tions employed for the elderly women with UI lessen the in-continence degrees and symptoms and increase their quality of life in terms of incontinence.
Table 5. Distribution of the Changes in the Mean Score of ISI, UDI-6, and I-QOL Scales before and after Intervention in the Experiment and Control Groups
Scales Experiment Control
Before intervention After
intervention
Before intervention After
intervention n X ± SD X ± SD n X ± SD X ± SD ISI 32 6.56± 4.45 2.50± 2.15 30 5.90± 4.01 7.03± 3.93 t= 6.745, p < .001 t= 2.246, p = .032 UDI-6 32 48.95± 21.28 15.27± 12.46 30 46.66± 20.08 46.66± 15.13 t= 9.002, p < .001 t= 0.000, p = 1.000 I-QOL 32 66.53± 28.69 112.84± 17.38 30 70.40± 22.17 71.93± 23.05 z= 4.732, p < .001 z= 1.297, p < .001
t: t test for dependent samples. z, Wilcoxon test.
p< .05 was considered significant.
Limitation of the Study
The lack of healthcare personnel in the nursing home may have created disruptions in the continuity of the initia-tive. Some elderly people have not accepted UI and are not seeking treatment. This situation has become a barrier for their adaptation to the nursing intervention. The fact that the nursing process was carried out manually rather than in the electronic environment caused time and labor loss for the health personnel in the nursing home. There are no sta-tistical differences for NANDA and NOCs before study inter-ventions between the experimental and control groups. But, in the study process, incompatibility of some elderlies may have affected the results of the study.
Conclusions
According to these results, employing the nursing care plan using NNN linkages, a positive change was observed in the incontinence-related NOC scores, I-QOL, ISI, and UDI-6 scales of the elderly women with UI, a decrease has been identified in the incontinence degree and symptoms, and their quality of life has increased. Additionally, in the guide used for this research, 27 NNN linkages were created. It is im-portant that these NNN linkages are used in different groups and with larger samples to create further evidence linking NNN.
Funding. We thank the editor and reviewers for their helpful
and constructive comments, which have helped develop this paper.
Authors’ contribution. All authors have agreed on the
fi-nal version and meet at least one of the following criteria, substantial contributions to conception and design, acquisi-tion of data, or analysis and interpretaacquisi-tion of data; drafting
the article or revising it critically for important intellectual content.
Conflict of interest. No conflict of interest was declared by
the authors in relation to the study itself. References
Abrams, P., Cardozo, L., Fall, M., Griffiths, D., Roiser, P., Ulmsten, U., … Wein, A. (2002). The standardisation of terminology of lower urinary tract func-tion: Report from the Standardisation Sub-Committe of the International Continence Society. Neurourology and Urodynamics, 21(2), 167–178. Albers-Heitner, C., Lagro-Janssen, A., Joore, M., Berghmans, L., Nieman, F.,
Venema, P., … Winkens, R. R. (2011). Effectiveness of involving a nurse spe-cialist for patients with urinary incontinence in primary care: Results of a pragmatic multicentre randomised controlled trial. International Journal
of Clinical Practice, 65(6), 705–712.
Al-Samarrai, N. R., Uman, G. C., Al-Samarrai, T., & Alessi, C. A. (2007). Introduc-ing a new incontinence management system for nursIntroduc-ing home residents.
Journal of the American Medical Directors Association, 8(4), 253–261.
American Nursing Association. (2015). Nursing intervention classification,
nursing: Scope and standards of practice (3rd ed.). Maryland: Silver Spring.
Angelica, T. H., Lee-Pin, W., Ajit, K., Wen-Shan, J., Li-Fang, H., Ching-Chiu, K., & Chien-Yeh, H. (2013). Nursing process decision support system for urology ward. International Journal of Medical Informatics, 82(7), 604–612. Ayeleke, R. O., Hay-Smith, E. J. C., & Omar, M. I. (2013). Pelvic floor muscle
training added to another active treatment versus the same active treat-ment alone for urinary incontinence in women. Cochrane Collaboration, 11, 1–105.
Azzolin, K., Mussi, C. M., Ruschel, K. B., de Souza, E. N., Lucena, A. D., & Rabelo-Silva, E. R. (2013). Effectiveness of nursing interventions in heart failure patients in home care using NANDA-I, NIC, and NOC. Applied Nursing
Re-search, 26(4), 239–244.
Beeckman, D., Verhaeghe, S., Defloor, T., Schoonhoven, L., & Vanderwee, K. (2011). A 3-in-1 perineal care wash cloth impregnated with dimethicone 3% versus water and pH neutral soap to prevent and treat incontinence-associated dermatitis: A randomized, controlled clinical trial. Journal of
Wound Ostomy & Continence Nursing, 38(6), 627–634.
Bitencourt, G. R., Alves, L. F., Santana, R. F., & Lopes, M. O. (2015). Agreement between experts regarding assessment of postoperative urinary elimina-tion nursing outcomes in elderly patients. Internaelimina-tional Journal of Nursing
Knowledge, 27(3), 143–148.
Borrie, M. J., Bawden, M., Speechley, M., & Kloseck, M. (2002). Interventions led by nurse continence advisers in the management of urinary inconti-nence: A randomized controlled trial. Canadian Medical Association
Jour-nal, 166(10), 1267–1273.
Brito-Brito, P. R., Oter-Quintana, C., Martín-García, Á., Alcolea-Cosín, M., Martín-Iglesias, S., & Fernández-Gutiérrez, D. Á. (2014). Case study:
Community nursing care plan for an elderly patient with urinary inconti-nence and social interaction problems after prostatectomy. International
Journal of Nursing Knowledge, 25(1), 62–65.
Bulechek, G., Butcher, H., Dochterman, J., & Wagner, C. (2012). Nursing
inter-ventions classification (NIC) (6th ed.). St. Louis, MO: Mosby.
Burgio, K. L., Locher, J. L., Goode, P. S., Hardin, J. M., McDowell, B. J., Dom-browski, M., & Candip, D. (1998). Behavioral vs drug treatment for urge urinary incontinence in older women: A randomized controlled trial.
Jour-nal of the American Medical Association, 280(23), 1995–2000.
Cam, C., Sakallı, M., Ay, P., Cam, M., & Karateke, A. (2007). Validation of the Short Forms of the Incontinence Impact Questionnaire (IIQ-7) and the Uro-genital Distress Inventory (UDI-6) in a Turkish Population. Neurourology
and Urodynamics, 26(1), 129–133.
Hazar, H. U., & ¸Sirin, A., A. (2008). Validity and reliablity study of the inconti-nence index. Adnan Menderes University Journal of Medical Faculty, 9(3), 5.
Herdman, T. H., & Kamitsuru, S. (2014). NANDA International nursing
diag-noses: Definitions and classification (2015–2017). Oxford: Wiley-Blackwell.
Johnson, M., Moorhead, S., Bulechek, G., Butcher, H., Maas, M., & Swanson, E. (2012). NOC and NIC linkages to NANDA-I and clinical conditions.
Sup-porting clinical reasoning and quality care (3rd ed.). Maryland, USA, MO:
Mosby.
Kane, R. L., & Xu, D. (2013). Addressing the quality-of-life implications of uri-nary incontinence among nursing home residents. Aging Health, 9(6), 603–605.
Kashanian, M., Ali, S. S., Nazemi, M., & Bahasadri, S. (2011). Evaluation of the effect of pelvic floor muscle training (PFMT or Kegel exercise) and assisted pelvic floor muscle training (APFMT) by a resistance device (Kegel master device) on the urinary incontinence in women “comparison between them: A randomized trial”. European Journal of Obstetrics & Gynecology and
Reproductive Biology, 159(1), 218–223.
Kautz, D. D., & Van Horn, E. R. (2008). An exemplar of the use of NNN language in developing evidence-based-practice guidelines. International Journal of
Nursing Knowledge, 19(1), 14–19.
Klay, M., & Marfyak, K. (2005). Use of a continence nurse specialist in an ex-tended care facility. Urologic Nursing, 25(2), 101–102.
Klutke, C. G., Burgio, K. L., Wyman, J. F., Guan, Z., Sun, F., & Berriman, S. (2009). Combined effects of behavioral intervention and tolterodine in patients dissatisfied with overactive bladder medication. Journal of Urology, 181(6), 2599–2607.
Lee, E., Park, H., Nam, M., & Whyte, J. (2011). Identification and comparison of interventions performed by Korean school nurses and U.S. school nurses using the Nursing Interventions Classification (NIC). Journal of School
Nursing, 27(2), 93–101.
Lewicky-Gaupp, C., Wei, J. T., DeLancey, J. O., Fenner, D. E., McGuire, E. J., & Morgan, D. M. (2008). The association of Incontinence Symptom Index scores with urethral function and support. American Journal of Obstetrics
and Gynecology, 199(6), 1–13.
Lin, S. Y. (2013). A pilot study: Fluid intake and bacteriuria in nursing home residents in southern Taiwan. Nursing Research, 62(1), 66–72.
Moorhead, S., Johnson, M., Mass, M., & Swanson, E. (2012). Nursing outcomes
classification (NOC). (5th ed.). St. Louis, MO: Mosby.
Moroni, R. M., Magnani, P. S., Haddad, J. M., de Aquino Castro, R., & Brito, L. G. O. (2016). Conservative treatment of stress urinary incontinence: A sys-tematic review with meta-analysis of randomized controlled trials.
Gyne-cology and Obstetrics, 38(2), 97–111.
Palese, A., & Carniel, G. (2011). The effects of a multi-intervention incontinence care program on clinical, economic, and environmental outcomes. Journal
of Wound Ostomy & Continence Nursing, 38(2), 177–183.
Patrick, D., Martin, M., Bushnell, D., Yalcin, I., Wagner, T., & Buesching, D. (1999). Quality of life of women with urinary incontinence: Further development of the incontinence quality of life instrument (I-QOL). Urology, 53(1), 71–76. Rosenberger, W. F., & Lachin, J. M. (2002). Randomization in clinical trials:
Theory and practice. Hoboken, NJ, USA: John Wiley & Sons, Inc.
Sandvik, H., Hunskaar, S., Seim, A., Hermstad, R., Vanvik, A., & Bratt, H. (1993). Validation of a severity index in female urinary incontinence and its im-plementation in an epidemiological survey. Journal of Epidemiology and
Community Health, 47(6), 497–499.
Shumaker, S. A., Wyman, J. F., Uebersax, J., McClish, D., & Fantl, J. A. (1994). Health-related quality of life measures for women with urinary inconti-nence: The incontinence impact questionnaire and the urogenital distress inventory. Quality of Life Research, 3(5), 291–306.
Tanaka, Y., Nagata, K., Tanaka, T., Kuwano, K., Endo, H., Otani, T., … Koyama, H. (2009). Can an individualized and comprehensive care strategy im-prove urinary incontinence (UI) among nursing home residents? Archives
of Gerontology and Geriatrics, 49(2), 278–283.
Tastan, S., Linch, G. C., Keenan, G. M., Stifter, J., McKinney, D., Fahey, L., … Wilkie, D. J. (2014). Evidence for the existing American Nurses Association-recognized standardized nursing terminologies: A systematic review.
In-ternational Journal of Nursing Studies, 51(8), 1160–1170.
Thüroff, J. W., Abrams, P., Andersson, K. E., Artibani, W., Chapple, C. R., Drake, M. J., … Tubaro, A. (2011). EAU guidelines on urinary incontinence. Actas
Urológicas Españolas, 35, 373–388.
Uebersax, J. S., Wyman, J. F., Shumaker, S. A., & McClish, D. K. (1995). Short forms to assess life quality and symptom distress for urinary incontinence in women: The Incontinence Impact Questionnaire and the Urogenital Dis-tress Inventory. Neurourology and Urodynamics, 14(2), 131–139. Vinsnes, A. G., Helbostad, J. L., Nyronning, S., Harkless, G. E., Granbo, R., &
Seim, A. (2012). Effect of physical training on urinary incontinence: A ran-domized parallel group trial in nursing homes. Journal of Clinical
Interven-tions in Aging, 7, 45–50.
Wagner, T., Patrick, D. L., Bavendam, T., Martin, M., & Buesching, D. (1996). Quality of life of persons with urinary incontinence: Development of a new measure. Urology, 47(1), 67–71.
Yoon, H. S., Song, H. H., & Ro, Y. J. (2003). A comparison of effectiveness of bladder training and pelvic muscle exercise on female urinary incon-tinence. International Journal of Nursing Studies, 40(1), 45–50. Zimmern, P., Litman, H. J., Mueller, E., Norton, P., & Goode, P. (2010). Effect
of fluid management on fluid intake and urge incontinence in a trial for overactive bladder in women. BJU International, 105(12), 1680–1685.