Vol.:(0123456789)
1 3
Acta Neurologica Belgica (2020) 120:935–937 https://doi.org/10.1007/s13760-019-01130-6
NEURO-IMAGES
Selective intra-arterial recombinant tissue-plasminogen activator
in a case of acute posterior inferior cerebellar artery occlusion
Gokhan Ozdemir1
Received: 21 January 2019 / Accepted: 19 March 2019 / Published online: 1 April 2019 © Belgian Neurological Society 2019
Introduction
Stroke is the third leading cause of death and the most com-mon cause of serious long-term disability in the world. Posterior circulation ischemic stroke (PCIS) accounts for approximately 20% of the total number of ischemic strokes and is associated with high rates of morbidity and mortality [1]. Endovascular procedures in large-artery occlusions have been demonstrated to provide clinical benefit in selected patients with acute ischemic stroke. The posterior inferior cerebellar artery (PICA) is the largest branch of the vertebral artery and is one of the largest arteries in the brain. Despite the fact that PICA infarcts are rare, rapid clinical deteriora-tion and sudden death may develop due to their presence [2]. Intravenous recombinant tissue-plasminogen activator (IV rt-PA) has been administered in cases of acute PICA occlusion. There is no case report about selective intra-arterial rt-PA treatment in cases of acute PICA occlusion in the literature. In this case report, we show that selective intra-arterial rt-PA administration for acute PICA occlusion is safe and effective.
Case description
A 61-year-old male was admitted to our clinic due to nausea and vomiting that had started 2 h previously. Dysarthria and truncal ataxia were detected during a neurological examina-tion of the patient. Acute ischemic stroke was seen in the left lateral cerebellum on the diffusion-weighted MRI (DWI). Eight milligrams of intravenous (IV) tissue plasminogen activator (tPA) was administered in the emergency room 3 h after the symptoms had started. The patient’s clinical
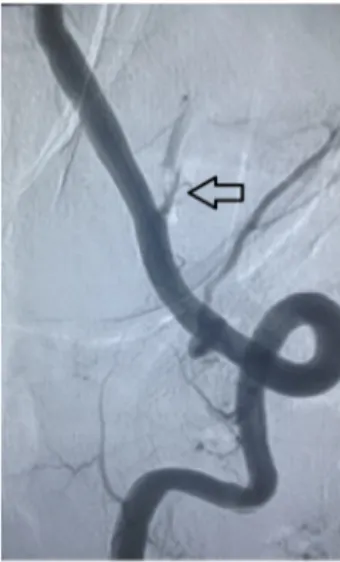
findings and magnetic resonance images suggested that there might be an occlusion of large blood vessels, such as verte-bral or basilar arteries. But the digital subtraction angiog-raphy DSA revealed only the left PICA occlusion (Fig. 1). Nine milligrams of intra-arterial rt-PA was administered into the PICA with a microcatheter three and a half hours after the symptoms had started. A successful recanalization into the PICA was accomplished after the administration of the rt-PA (Fig. 2). The time from groin puncture to reca-nalization was 17 min. Subsequent to the intervention, the patient was transferred to the intensive care unit. After the endovascular treatment, the patient underwent a follow-up CT scan within 24 h of thrombolysis. There was no bleed-ing in the brain. Antiplatelet and antihypertensive treatment was administered to the patient after the follow-up CT scan. Laboratory examination showed vitamin B12 deficiency. No cardiac arrhythmia was demonstrated in ECG examina-tion. The transthoracic echocardiography and carotid artery Doppler were normal. A paroxysmal rhythm disorder was not detected by the Holter monitor. The patient was in good condition after the intervention, and he was transferred to the neurology clinic. He consulted with the nutritionist for oral alimentation regulation. There were no complications, and the patient was discharged on the third day post-intervention.
Discussion
The PICA is the largest branch of the vertebral artery; it sup-plies blood to the inferior portion of the vermis, the lower medulla, and the posteroinferior cerebellar hemispheres. PICA occlusion is a rare clinical entity in ischemic stroke syndromes. The clinical symptoms of PICA occlusion include vertigo, nausea, vomiting, ipsilateral facial numb-ness, dysmetria, Horner’s syndrome, dysphagia, ataxia, dys-phonia, and contralateral hemisensory loss below the face [3]. Rapid deterioration in neurological status leading to a coma and often death may develop in patients with PICA
* Gokhan Ozdemir
noro.ozdemir@gmail.com; dekanlik@selcuk.edu.tr 1 Department of Neurology, Selcuk University Medical
936 Acta Neurologica Belgica (2020) 120:935–937
1 3
occlusion [2]. Treatment options for acute posterior circula-tion occlusions are an IV-rt-PA, intra-arterial thrombolysis, and endovascular thrombectomy [4]. Recent studies have shown that intravenous t-PA treatment improves clinical out-comes at 3 months and reduces disability [5, 6]. However, the recanalization rate of occlusions in the vertebrobasilar system is higher in patients that were administered arterial thrombolysis than those who were treated with intra-venous therapy [7, 8]. In addition, Wolfe et al. showed that the recanalization rate is higher when using combined IA
and IV therapy. In spite of that, the risk of symptomatic intracerebral hemorrhage and mortality were not signifi-cantly higher in thrombolysis therapy modalities [9]. Moreo-ver, there was no significant difference in the rate of serious adverse events between these therapy modalities [10]. We also administered combined therapy to our patient. There was no complication during follow-up.
The effectiveness of selective intra-arterial thromboly-sis therapy for large artery occlusions in the vertebrobasilar system (the vertebral, basilar, and posterior cerebral artery) has been demonstrated. In this case report, we showed that combined IV and IA tPA treatment can be performed safely and effectively to treat PICA occlusions. But the process should be done very carefully.
Acknowledgements I would like to thank the nurses, technicians and assistants who worked in Neurology Department of Selcuk University.
Funding This research received no specific Grant from any funding agency in the public, commercial, or not for profit sectors.
Compliance with ethical standards
Conflict of interest The authors declare no competing financial inter-est.
References
1. Long J, Qin H, Zhang H (2017) Evaluation of recanalisation treatment on posterior circulation ischemic stroke by Solitaire device—a multicenter retrospective study. Neurol Neurochir Pol 51(3):208–213. https ://doi.org/10.1016/j.pjnns .2017.02.004
(Epub 2017 Mar 24)
2. Macleod MR, Davis SM, Mitchell PJ, Gerraty RP, Fitt G, Hankey GJ, Stewart-Wynne EG, Rosen D, McNeil JJ, Bladin CF, Cham-bers BR, Herkes GK, Young D, Donnan GA (2005) Results of a multicentre, randomised controlled trial of intra-arterial urokinase in the treatment of acute posterior circulation ischaemic stroke. Cerebrovasc Dis 20(1):12–17. (Epub 2005 May 30)
3. Barinaga Rementeria F, Amaya LE, Cantú C (1997) Causes and mechanisms of cerebellar infarction in young patients. Stroke 28(12):2400–2404
4. Amre Nouh J, Remke, Ruland S (2014) Ischemic posterior circula-tion stroke: a review of anatomy, clinical presentacircula-tions, diagnosis, and current. Manag Front Neurol 5:30. https ://doi.org/10.3389/ fneur .2014.00030 . (Published online 2014 Apr 7)
5. Mathews MS, Sharma J, Snyder KV, Natarajan SK, Siddiqui AH, Hopkins LN, Levy EI (2009) Safety, effectiveness, and practi-cality of endovascular therapy within the first 3 hours of acute ischemic stroke onset. Neurosurgery 65(5):860–865 https ://doi. org/10.1227/01.NEU.00003 58953 .19069 .E5 (discussion 865) 6. Nakashima T, Minematsu K (2009) Prospects of thrombolytic
therapy for acute ischemic stroke. Brain Nerve 61(9):1003–1012 7. Rha JH, Saver JL (2007) The impact of recanalization on ischemic stroke outcome: a meta-analysis. Stroke 38(3):967–973 (Epub
2007 Feb 1)
8. Lindsberg PJ, Mattle HP (2006) Therapy of basilar artery occlu-sion a systematic analysis comparing intra-arterial and intravenous thrombolysis. Stroke 37(3):922–928
Fig. 1 Digital subtraction angiography (DSA) revealed the left PICA occlusion (arrow)
Figs. 2 Recanalization in the PICA (star: microcatheter, black arrow:
937 Acta Neurologica Belgica (2020) 120:935–937
1 3
9. Wolfe T, Suarez JI, Tarr RW, Welter E, Landis D, Sunshine JL,Zaidat OO (2008) Comparison of combined venous and arterial thrombolysis with primary arterial therapy using recombinant tissue plasminogen activator in acute ischemic stroke. J Stroke Cerebrovasc Dis 17(3):121–128
10. Ciccone A, Valvassori L, Ponzio M, Ballabio E, Gasparotti R, Sessa M, Scomazzoni F, Tiraboschi P, Sterzi R, SYNTHESIS Investigators (2010) Intra-arterial or intravenous thrombolysis for
acute ischemic stroke? The SYNTHESIS pilot trial. J Neurointerv Surg 2(1):74–79
Publisher’s Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.