December 2015 Brief Communications 921 posterior scleritis. Subtle evidence of inflammation such as
episcleritis raised autoimmune markers may provide a clue to the diagnosis of this uncommon condition.
Clinical misinterpretation of nodular posterior scleritis as malignant melanoma can lead to misguided therapy and devastating outcomes, including enucleation. When a choroidal mass presents with atypical features of melanoma, any evidence of inflammation may suggest its inflammatory rather than malignant cause. A trial of anti‑inflammatory medication may serve as a therapeutic test and help spare patients from invasive and unnecessary interventions.
Financial support and sponsorship Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. McCluskey PJ, Watson PG, Lightman S, Haybittle J, Restori M, Branley M. Posterior scleritis: Clinical features, systemic associations, and outcome in a large series of patients. Ophthalmology 1999;106:2380‑6.
2. Biswas J, Mittal S, Ganesh SK, Shetty NS, Gopal L. Posterior scleritis:
Clinical profile and imaging characteristics. Indian J Ophthalmol 1998;46:195‑202.
3. Shields JA, Augsburger JJ, Brown GC, Stephens RF. The differential diagnosis of posterior uveal melanoma. Ophthalmology 1980;87:518‑22.
4. Hage R, Jean‑Charles A, Guyomarch J, Rahimian O, Donnio A, Merle H. Nodular posterior scleritis mimicking choroidal metastasis: A report of two cases. Clin Ophthalmol 2011;5:877‑80.
5. Accuracy of diagnosis of choroidal melanomas in the Collaborative Ocular Melanoma Study. COMS report no 1. Arch Ophthalmol 1990;108:1268‑73.
6. Finger PT, Perry HD, Packer S, Erdey RA, Weisman GD, Sibony PA. Posterior scleritis as an intraocular tumour. Br J Ophthalmol 1990;74:121‑2.
7. Osman Saatci A, Saatci I, Kocak N, Durak I. Magnetic resonance imaging characteristics of posterior scleritis mimicking choroidal mass. Eur J Radiol 2001;39:88‑91.
8. Shukla D, Kim R. Giant nodular posterior scleritis simulating choroidal melanoma. Indian J Ophthalmol 2006;54:120‑2. 9. Sridharan S, Juneja R, Hussain A, Biswas J. Giant nodular posterior
scleritis mimicking choroidal tumor. Retin Cases Brief Rep 2007;1:65‑7.
10. Demirci H, Shields CL, Honavar SG, Shields JA, Bardenstein DS. Long‑term follow‑up of giant nodular posterior scleritis simulating choroidal melanoma. Arch Ophthalmol 2000;118:1290‑2.
Department of Eye, Faculty of Medicine, Ufuk University, Ankara, Turkey Correspondence to: Dr. Gülizar Demirok, 1425 Avenue, Hayat Sebla Apartment Number 30/37, Kızılırmak Street, Çankaya, Ankara, Turkey. E‑mail: gsoyugelen@yahoo.com
Manuscript received: 11.06.15; Revision accepted: 30.11.15
Unilateral sequential papillophlebitis
and central retinal artery occlusion in
a young healthy patient
Gülizar Demirok, Mehmet Fatih Kocamaz,
Yasemin Topalak, Ahmet Şengün,
Berati Hasanreisoğlu
A 23‑year‑old girl presented to the clinic with metamorphopsia and photopsia in her left eye. After detailed ophthalmic examination, central retinal vein occlusion with optic disc edema was detected in that eye. Three days after diagnosis, the patient returned to our clinic with visual acuity decrease. Central retinal artery occlusion sparing cilioretinal artery was detected. All the laboratory tests were normal except for heterozygous methylenetetrahydrofolate reductase mutation (A1298C
genotypes) and an indefinite Lyme disease seropositivity. Symptoms and visual disturbance recovered without any further treatment other than acetylsalicylic acid for prophylaxis.
Key words: A1298C mutation, central retinal artery occlusion, central retinal vein occlusion, methylenetetrahydrofolate reductase gene mutation, papillophlebitis
Retinal vascular occlusions, including arterial and venous obstructions, are serious pathologies that can cause blindness. The clinical characteristics and prognosis are influenced by the location of the occlusion. The presence of cilioretinal artery is vitally important for visual prognosis in central retinal artery occlusions (CRAO).[1]
Central retinal vein occlusion (CRVO) in the young is also known as papillophlebitis and is caused by compression of the central retinal vein due to inflammation of the optic nerve head. CRVO is mostly seen as an isolated event in young adults; however, a previous report showed that there might be some underlying systemic associations in up to 50% of affected individuals.[2]
CRAO in young patients may be caused by hyperhomocysteinemia, systemic lupus erythematosus, Access this article online
Quick Response Code: Website:
www.ijo.in
DOI:
10.4103/0301-4738.176029
PMID:
***
Cite this article as: Demirok G, Kocamaz MF, Topalak Y, Sengün A,
Hasanreisoglu B. Unilateral sequential papillophlebitis and central retinal artery occlusion in a young healthy patient. Indian J Ophthalmol 2015;63:921-4. This is an open access article distributed under the terms of the Creative Commons Attribution‑NonCommercial‑ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non‑commercially, as long as the author is credited and the new creations are licensed under the identical terms.
For reprints contact: reprints@medknow.com
922 Indian Journal of Ophthalmology Vol. 63 No. 12 trauma, sickle cell disease, platelet abnormalities, in addition
to embolic disease.[3,4]
Combined papillophlebitis and CRAO in the same eye are a devastating and rare entity, especially in an otherwise healthy young patient. Herein, we are trying to report this unusual entity with an extensive laboratory workup to determine the etiological factor. The present case provides, to our knowledge, the first description of this combined entity with sparing cilioretinal artery and excellent visual prognosis in the affected eye.
Case Report
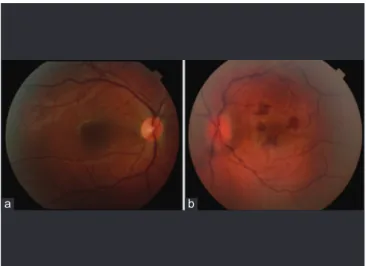
A 23‑year‑old healthy female patient presented with metamorphopsia and photopsia in her left eye. At presentation, the best‑corrected visual acuity (BCVA) was 20/20 in both eyes. Her medical history was unremarkable except her smoking habit (20/day) and coke drinking habit (2l/day). Anterior segment examination and intraocular pressures were within normal limits (17 mmHg) in both eyes. Dilated fundus examination of the left eye showed blurred optic disc margins with hyperemic disc swelling, venous engorgement, and preretinal hemorrhages in the macula. No abnormalities were found in the right eye [Fig. 1a and b]. The optical coherence tomography revealed retinal thickening in the left eye.
Extensive laboratory workup including the complete blood count, serum C‑reactive protein, erythrocyte sedimentation rate (ESR), C‑protein, S‑protein, D‑dimer, lupus test, antinuclear antibody, prothrombin time/partial thromboplastin time, antithrombin III activity, factor V Leiden and prothrombin gene mutation, anticardiolipin antibody, antineutrophil cytoplasmic antibodies, angiotensin converting enzyme, and homocysteine levels were ordered to rule out underlying conditions that might cause papillophlebitis.
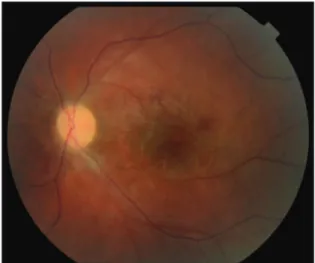
At the 3rd day of follow‑up, she noted a sudden visual loss in
the left eye. BCVA was 20/20 in her right eye and 20/200 in the left eye. Dilated fundus examination revealed CRAO [Fig. 2] and intact cilioretinal artery circulation was determined by fundus fluorescein angiography [Fig. 3]. Since the macular perfusion was good, there is no proof to accompany of an embolism; the emergency treatment of CRAO, including hyperbaric oxygen or anterior chamber lavage, were not done; only acetylsalicylic acid (ASA) drug 100 mg/day treatment was started.
Routine laboratory findings only showed a mild elevation of white blood cells, ESR, and C‑reactive protein. The chest X‑ray and magnetic resonance imaging of brain and orbits were normal. All of the tests which were studied to determine the cause of the papillophlebitis were negative except heterozygous (A1298C) methylenetetrahydrofolate reductase (MTHFR) mutation. Despite the fact that the heterozygous mutation of this gene is very common and harmless, the patient was consulted to a hematologist because of the clinical signs. It was reported that this kind of mutation could not cause this condition alone. She was consulted by a cardiologist and a dermatologist who did not reveal any etiological factor.
At the 5th day of follow‑up, BCVA increased but there were
cells (2+) bilaterally in the anterior chamber and serologic study was conducted for iridocyclitis. Only the Western blot test for Borrelia burgdorferi was positive. Since Turkey was
Figure 2: Fundus photography of the left eye on the 3rd day of the presentation with central retinal artery occlusion. Note retinal edema except foveal region
Figure 3: Fundus fluorescein angiography of the left eye on the 3rd day of the presentation. Note intact cilioretinal artery circulation
Figure 1: (a) Fundus photography of the normal right eye at the
initial presentation (b) fundus photography of the left eye at the initial presentation. Note mildly edematous optic disc, dilated and tortuous retinal veins, and preretinal hemorrhages in the macula
b a
December 2015 Brief Communications 923
Figure 4: The left eye with the pale optic disc and attenuated arteries
on the 20th day of the presentation
an endemic region for this infection, the infectious disease specialist suggested starting antibiotheraphy although there was no history of any tick bite.
At the 20th day of the examination, left optic disc was pale;
the hemorrhages and retinal edema were decreased, and arteries were attenuated [Fig. 4]. On the other hand, BCVA was 20/20 in both eyes. Since the cardiology department suggested the patient to be on ASA, we decided to continue her medication.
Discussion
Papillophlebitis is believed to be a type of CRVO in young people; the exact cause is still not known. It can be isolated or can be seen with retinal artery occlusion, most commonly cilioretinal artery.[5] In the current case, the occluded artery
after papillophlebitis was central retinal artery. The increased venous pressure after CRVO may have impaired the retinal blood flow, so these two vascular entities may be related. The second possible pathomechanism that is caused to suggest the linkage between them is inflammation of optic disc that caused to disruption of retinal blood flow. The inflammation may be related to smoking, nutritional deficiency, and unhealthy lifestyle of the patient. Because of the papillophlebitis has a better natural course compared retinal vein occlusion in older adults and the presence of an intact cilioretinal circulation, our patient gained her visual acuity without any further treatment.
The enzyme MTHFR has an important role in homocysteine metabolism; therefore, decreased enzyme activity leads to buildup of homocysteine and can cause thromboembolic events.[6]
Turaka et al. reported a case of young female with unilateral papillophlebitis who was found to have positive homozygous mutations for MTHFR C677T and A1298C genes. Although there was no information about the blood level of homocysteine in that case report, presumed hyperhomocysteinemia was thought as the main cause for that hypercoagulable state.[7] Conversely,
in our patient, there was a heterozygous mutation of A1298C MTHFR and homocysteine level was normal (=6,9 µmol/L). A previous study showed mutation of A1298C MTHFR was a risk for early coronary disease without hyperhomocysteinemia.
[8] Thus, heterozygous A1298C mutations may also present an
independent risk factor for thrombosis, especially if combined
with unhealthy lifestyle and some risk factors such as smoking, high stress, and toxic exposures.
Lyme is a spirochetal disease responsible for a multitude of ocular and systemic manifestations. While it is an uncommon cause of papillitis, it can be presented with severe acute anterior uveitis, howbeit previous cases reported unilateral papillitis as the sole significant ocular sign of Lyme disease.[9]
Therefore, due to accompanying bilateral anterior chamber reaction, Lyme seropositivity, and being in an endemic area for Lyme, she was treated with intravenous ceftriaxone with the recommendation of infectious diseases department, despite the lack of any bite story.
Performing extensive laboratory workup is very important in such patients to rule out some etiologic factors. Furthermore, it should be known that heterozygous mutation of A1298C MTHFR gene may cause thromboembolic events even if with the presence of normal homocysteine levels.[8] Based on this knowledge, we
decided to recommend systemic anticoagulant therapy, other than ASA to our patient for prophylaxis. The limitation of our paper is that the exact cause of anterior chamber reaction was not clearly determined, and it might have been a simultaneous self‑healing iridocyclitis with false positive Lyme serology.
Although combined CRVO (or papillophlebitis) and CRAO entity tend to develop devastating complications such as rubeosis iridis, macular ischemia, and neovascular glaucoma,[10]
in the present case, even in the 3rd month of vascular occlusion,
neovascularization or macular ischemia was not seen and the visual prognosis was excellent, due to good perfusion of cilioretinal artery in the affected eye. In this regard, this patient is one of the rare cases which vision is preserved despite the combined CRVO and CRAO. The most important challenge for this case is to determine the exact etiology.
Last, heterozygous mutation of A1298C MTHFR with an unhealthy lifestyle or Lyme disease with an atypical presentation may be the reason for this condition in such a young healthy person.
Financial support and sponsorship Nil.
Conflicts of interest
There are no conflicts of interest.
References
1. Hayreh SS, Podhajsky PA, Zimmerman MB. Natural history of visual outcome in central retinal vein occlusion. Ophthalmology 2011;118:119‑33.
2. Fong AC, Schatz H. Central retinal vein occlusion in young adults. Surv Ophthalmol 1993;37:393‑417.
3. Brown GC, Magargal LE, Shields JA, Goldberg RE, Walsh PN. Retinal arterial obstruction in children and young adults. Ophthalmology 1981;88:18‑25.
4. Greven CM, Slusher MM, Weaver RG. Retinal arterial occlusions in young adults. Am J Ophthalmol 1995;120:776‑83.
5. Schatz H, Fong AC, McDonald HR, Johnson RN, Joffe L, Wilkinson CP, et al. Cilioretinal artery occlusion in young adults with central retinal vein occlusion. Ophthalmology 1991;98:594‑601. 6. Hanson NQ, Aras O, Yang F, Tsai MY. C677T and A1298C
polymorphisms of the methylenetetrahydrofolate reductase gene: Incidence and effect of combined genotypes on plasma fasting and
924 Indian Journal of Ophthalmology Vol. 63 No. 12
Minimal gauge vitrectomy for optic
disc pit maculopathy: Our results
Atul Kumar, Varun Gogia, Ritu Nagpal, Sangeeta Roy,
Shikha Gupta
The purpose of the study was to describe the surgical technique and clinical outcomes of pars plana vitrectomy without laser or gas tamponade in cases with optic disc pit maculopathy at our centre. Six eyes of six consecutive patients presenting with unilateral optic disc pit maculopathy were enrolled. Preoperative optical coherence tomography (OCT) was performed to determine the presence and extent of schisis and macular detachment. All eyes underwent 23‑gauge pars plana vitrectomy with induction of posterior vitreous detachment (PVD) and internal limiting membrane (ILM) peeling and eyes were closed under fluid. Patients were followed up for at least 12 months post‑surgery. Median age of patients was 22.5 years. Five of six eyes had neurosensory detachment (NSD) at the presentation; whereas, inner layer schisis was present in all patients. None of the patients had any evidence of vitreomacular or vitreopapillary adhesion or PVD either clinically or on OCT. Inner and outer retinal schisis resolved in all eyes after follow‑up of at least 6 months. Resolution of subretinal fluid in eyes with NSD was seen in 4 of 5 eyes. There was a significant visual acuity improvement from mean preoperative visual acuity of 0.79 logarithm of the minimum angle of resolution (logMAR) units to 0.36 logMAR units at 12 months (P = 0.001). Thus, vitrectomy with ILM peeling and PVD induction alone could achieve good functional outcomes in cases with optic disc pit maculopathy.
Key words: Internal limiting membrane peeling, maculopathy, optic disc pit, schisis
Optic nerve pits are a rare entity and are generally asymptomatic unless complicated by macular involvement in the form of macular schisis, neurosensory detachment (NSD), or pigmentary changes owing to chronicity which is seen in 25–75% of patients.[1,2]
Management of optic pit related maculopathy is controversial and includes observation, laser of pit margin, scleral buckling, and pars plana vitrectomy.[1,3‑7] The use of laser therapy to
produce scarring of the margins is often unsuccessful, and repeated treatments are needed.[1,3,4] Various reports suggest
that vitrectomy combined with laser photocoagulation and gas tamponade may be more effective than laser, particularly in eyes with severe visual loss.
However, Hirakata et al. had hypothesized that gas tamponade may not be necessary considering slow resolution of macular changes after surgery and have reported good anatomical and functional outcomes in their recent series without use of gas tamponade.[8]
We report our experience in this series of six cases with optic nerve head pit maculopathy (ONH‑M) who underwent pars plana vitrectomy with posterior vitreous detachment (PVD) induction without gas tamponade or laser treatment.
Methods
Consecutive patients with unilateral optic disc pit with maculoschisis with/without NSD and diminished visual acuity (<6/18) were included. All patients underwent baseline ophthalmological examination and spectral domain optical coherence tomography (OCT) to confirm the optic disc pit and macular abnormalities in all patients.
All underwent 23‑gauge pars plana vitrectomy with triamcinolone acetonide‑assisted PVD induction and internal limiting membrane (ILM) peeling. Separation of posterior hyaloid over the schitic area was done cautiously to prevent deroofing of the schisis cavity. Surgery was concluded with fluid filled vitreous cavity, and no tamponading agent was used. No laser was performed at the pit margin in any of the cases.
Dr. Rajendra Prasad Centre for Ophthalmic Sciences, All India Institute of Medical Sciences, New Delhi, India
Correspondence to: Dr. Varun Gogia, Dr. Rajendra Prasad Centre for Ophthalmic Sciences, All India Institute of Medical Sciences, New Delhi ‑ 110 029, India. E‑mail: varungogia@gmail.com
Manuscript received: 25.07.14; Revision accepted: 14.11.15 Access this article online
Quick Response Code: Website:
www.ijo.in
DOI:
10.4103/0301-4738.176030
PMID:
***
Cite this article as: Kumar A, Gogia V, Nagpal R, Roy S, Gupta S. Minimal
gauge vitrectomy for optic disc pit maculopathy: Our results. Indian J Ophthalmol 2015;63:924-6.
This is an open access article distributed under the terms of the Creative Commons Attribution‑NonCommercial‑ShareAlike 3.0 License, which allows others to remix, tweak, and build upon the work non‑commercially, as long as the author is credited and the new creations are licensed under the identical terms.
For reprints contact: reprints@medknow.com
post‑methionine load homocysteine in vascular disease. Clin Chem 2001;47:661‑6.
7. Turaka K, Ziemianski MC, Bryan JS. Papillophlebitis in a Young Girl Secondary to Homozygous Mutation of MTHFR C677T and A1298C Genotypes. Retina Today; March 2013.
8. Szczeklik A, Sanak M, Jankowski M, Dropinski J, Czachór R, Musial J, et al. Mutation A1298C of methylenetetrahydrofolate
reductase: Risk for early coronary disease not associated with hyperhomocysteinemia. Am J Med Genet 2001;101:36‑9.
9. McVeigh K, Vakros G. Case report: Papillitis as the sole ocular sign in lyme disease. Clin Ophthalmol 2012;6:1093‑7.
10. Md Noh UK, Fang SY, Md Din N. Central retinal artery occlusion following central retinal vein occlusion – A case report. J Diabetes Metab 2015;6:566.