SCIENTIFIC ARTICLE
Treatment of Kienböck Disease by Lunate Core
Decompression
Saeed Reza Mehrpour, MD, Reza Shahriar Kamrani, MD, Mohamad Reza Aghamirsalim, MD, Reza Sorbi, MD, Alper Kaya, MD
Purpose Kienböck disease is characterized by avascular necrosis of the lunate bone, which is usually progressive without treatment. This study examined lunate core decompression for its treatment potential.
Methods We surgically treated 20 patients with stage 1 to 3b Kienböck disease with lunate
core decompression. We evaluated pain, range of motion, functional disability, and radio-graphic indices in these patients at baseline and 5 years after surgery.
Results The mean age of the patients was 29 years; 16 were men. Ten patients had Lichtman
stage 1 disease, 6 had stage 2 disease, 3 had stage 3a, and 1 had stage 3b disease. Range of motion scores showed meaningful improvement. Two patients did not improve with this technique and were revised with radial shortening procedures.
Conclusions Lunate core decompression is a simple surgical procedure that is effective in the treatment of Kienböck disease. (J Hand Surg 2011;36A:1675–1677. Copyright © 2011 by the American Society for Surgery of the Hand. All rights reserved.)
Type of study/level of evidence Therapeutic IV.
Key words Kienböck disease, decompression, functional disability, pain
K
IENBÖCK ORIGINALLY DESCRIBED lunatomalaciaand its characteristic radiographic findings in 1910.1He surmised that some form of trauma leads to a “disturbance of the nutrition” of the lunate, causing sclerosis, fracture, and collapse. The natural history of Kienböck disease is unknown, although the disease is assumed to progress through stages, as first described by Stahl and modified by Lichtman and
Deg-nan.2 Specifically, the natural history of the disease
suggests that the lunate will ultimately fracture and collapse. As a result, the carpus itself collapses, with the
scaphoid assuming a hyperflexed position. Eventually, the wrist becomes arthritic as a result of the altered
biomechanics.2
Many factors may predispose to Kienböck disease, but it is likely caused by a combination of repetitive
loading, vascular risk, and mechanical predisposition.3,4
As a result, treatments to date have been designed to decrease compressive loading of the lunate to prevent lunate collapse and allow lunate revascularization.
In 1928, Hulten observed an association between negative ulnar variance and the development of Kien-böck disease. Many studies have supported this obser-vation and have recommended shortening of the
ra-dius5,6 or lengthening of the ulna.7 Success has been
observed even in the absence of a negative ulnar
vari-ance.8Favorable results have been reported after medial
or lateral closing osteotomy of the radius.9 These
dis-crepancies further question the value of joint-leveling procedures.
Hori et al10showed that transplantation of an
arte-riovenous pedicle into normal and avascular bone resulted in the formation of new bone. Since then,
FromtheDepartmentofOrthopedicandTraumaSurgery,ShariatiHospital,TehranUniversityofMed-ical Sciences; and the Department of Orthopaedics and Traumatology, Ufuk University, Balgat, An-kara, Turkey.
Received for publication September 23, 2010; accepted in revised form June 22, 2011. No benefits in any form have been received or will be received related directly or indirectly to the subject of this article.
Corresponding author: Mohamad Reza Aghamirsalim, MD, Department of Orthopedic Surgery,
Tehran University of Medical Sciences, Shariati Hospital, Kargar Shomali Street, Tehran, Iran 192303; e-mail:aghamirsalim@gmail.com.
0363-5023/11/36A10-0017$36.00/0 doi:10.1016/j.jhsa.2011.06.024
© ASSH䉬Published by Elsevier, Inc. All rights reserved.䉬1675
Downloaded for Anonymous User (n/a) at Ufuk Universitesi from ClinicalKey.com by Elsevier on August 01, 2018. For personal use only. No other uses without permission. Copyright ©2018. Elsevier Inc. All rights reserved.
different types of vascularized bone graft have been suggested to treat Kienböck disease.11,12Because some
studies13–15have reported many complications related
to joint-leveling procedures, including nonunion, infec-tion, and ulnar impingement, and the need for plate removal in most patients undergoing radial shortening, the authors of this study performed lunate core decom-pression. The purpose of this study was to report the medium-term results of lunate core decompression for Kienböck disease.
PATIENTS AND METHODS
This study examined 20 patients (16 men and 4 women, average age 29 y, range, 21– 42 y) with Kienböck disease treated by lunate core decompression performed at a single institution between 2004 and 2010. We included patients with stage 1 to 3b Kienböck disease who were willing to give informed consent. Exclusion criteria consisted of patients with previous surgery of the wrist, stage 4 disease, the presence of osteoarthritis in the wrist, and a history of major wrist trauma. Before the intervention, we explained the various treatment methods to the patients. All patients were evaluated by subjective questionnaires before surgery, which in-cluded a visual analog scale (VAS) and the Disabilities of the Arm, Shoulder, and Hand score. Each patient signed an informed consent form before the procedure. A total of 15 patients showed radiographic evidence of Kienböck disease without osteoarthritis at the time of the decompression procedure. In the other 5 patients who had Lichtman stage I Kienböck disease, we made the diagnosis using magnetic resonance imaging. We identified 10 patients as stage 1, 6 as stage 2, 3 as stage 3a, and 1 as stage 3b, Measurement of the carpal height ratio and radioscaphoid angle were part of the preoper-ative evaluation. The ulnar variance was determined by measuring the distance between lines drawn perpendic-ular to the long axis of the radius and tangential to the lunate facet of the radial articular surface and the distal extent of the ulnar head. We obtained magnetic reso-nance imaging for all patients preoperatively to clearly define the extent of necrosis and rule out other condi-tions. We examined all patients for wrist range of mo-tion and lunate tenderness. We repeated all measure-ments 5 years postoperatively and compared them with the preoperative values using paired Student t-test. Surgical technique
We approached the wrist with a transverse dorsal 2-cm incision directly over the lunate. The extensor retinac-ulum was raised as a radial-based flap and the capsule in the fourth dorsal compartment was raised as a
prox-imally based flap. We identified the lunate with a guide-wire under fluoroscopic control. We used a dental burr (2.5 mm) to decompress the lunate thoroughly from a dorsal entry under fluoroscopic control. We did not remove the cancellous bone.
After decompression, we repaired the capsule, reti-naculum, and skin in layers and placed a splint. After 1 week, we applied a light cast for 6 weeks to protect the decompressed bone. Then we initiated range of motion exercises. In cases where the patient’s symptoms did not greatly improve after 6 months, we suggested an-other procedure such as radial shortening. We evaluated patients with the same questionnaires 5 years after the procedure, re-evaluated radiographic indices, and as-sessed wrist motions.
RESULTS Subjective findings
Postoperative frequency of pain decreased from a mean preoperative rating (visual analog scale) of 88 to 14 (P ⬍ .001). Preoperative episodes of pain severe enough to awake the patient from sleep were observed in 18 of 20 patients and in 1 patient postoperatively (P⬍ .001). Splints were used in 17 of the 20 patients preoperatively compared with 3 patients postopera-tively. Nonsteroidal anti-inflammatory medications, narcotics, or both were used routinely in 18 of the 20 patients preoperatively compared with 4 patients post-operatively.
Disabilities of the Arm, Shoulder, and Hand scores decreased from a mean preoperative score of 84 to a postoperative score of 14 (P ⬍ .001), indicating that most patients had functional preoperative disabilities and that most showed postoperative improvements. The most noteworthy improvements were in the ability to open jars and car doors, and to use a screwdriver.
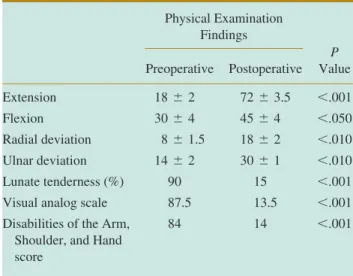
Postoperatively, wrist flexion, extension, radial devi-ation, and ulnar deviation improved significantly (Table
1). Preoperatively, 18 of the 20 patients had expressed
lunate tenderness to palpation, compared with 3 patients
postoperatively (P⬍ .001).
Postoperatively, most patients showed no change in Lichtman stage. The preoperative carpal height ratio
was 0.56 ⫾ 0.10 compared with 0.55 ⫾ 0.09
postop-eratively, which indicated no collapse in carpals during the 5-year follow-up.
We saw no complication related to the core decom-pression. Two patients with stage 3a and 3b disease, respectively, had radial shortening procedures because the pain did not change notably 6 months after lunate decompression.
1676 LUNATE CORE DECOMPRESSION
JHS䉬VolA, October
Downloaded for Anonymous User (n/a) at Ufuk Universitesi from ClinicalKey.com by Elsevier on August 01, 2018. For personal use only. No other uses without permission. Copyright ©2018. Elsevier Inc. All rights reserved.
DISCUSSION
Vascular insufficiency and microtraumatic factors16 likely have a role in the development and progression of Kienböck disease. Although joint-leveling procedures and revascularization techniques have become the stan-dard treatment during the past decade, these procedures have not been able to reverse Kienböck disease, and as many as 25% of patients have reported
complica-tions14,15,17 including infection, nonunion, and ulnar
impingement. Although hardware removal is not con-sidered a complication, in 1 study, greater than 70% of patients required a second surgery to remove hardware
to relieve pain or extensor tendonitis.18
We thought that lunate decompression could de-crease the intraosseous pressure as occurs with femoral head avascular necrosis, which has good results with
core decompression in early stages.19
In 2001, Illaramendi20 described distal radius and
ulna core decompression for Kienböck disease, with good results. The radius and ulna decompression pro-cedures may diminish the pain via secondary hyper-emia. The lunate decompression technique directly decreases intraosseous pressure, which may lead to increased comfort, motion, and revascularization.
This study proposed lunate decompression for the treatment of Kienböck disease with similar benefits as joint-leveling procedures (reduction in pain, improve-ment in functional activity, and improveimprove-ment of mo-tion) but with fewer complications. The disease did not progress, except in 2 patients whose pain did not im-prove after lunate decompression, and who subse-quently required radial shortening. Both of these patients were stage 3, so we suggest this method only in stage 1 and 2 of Kienböck disease. The results of this
study are similar to those of several studies on radial
shortening.12–15The main advantage of this procedure
is that it is simpler, with less risk of complications than the joint-leveling procedures. This preliminary study did not include a control group. A randomized trial on the effectiveness of this procedure is therefore neces-sary.
REFERENCES
1. Peltier LF. The classic. Concerning traumatic malacia of the lunate and its consequences: degeneration and compression fractures. Privatdozent Dr. Robert Kienböck. Clin Orthop 1980;149:4 – 8. 2. Lichtman DM, Degnan GG. Staging and its use in the determination
of treatment modalities for Kienböck’s disease. Hand Clin 1993;9: 409.
3. Amadio PC, Hanssen AD, Berquist TH. The genesis of Kienböck’s disease: evaluation of a case by magnetic resonance imaging. J Hand Surg 1987;12A:1044 –1049.
4. Almquist EE. Kienböck’s disease. Clin Orthop Relat Res 1986;202: 68 –78.
5. Tatebe M, Horii E, Majima M, Koh S, Nakamura R, Hirata H. Radial osteotomy for Kienböck’s disease with displaced fracture of the lunate. J Hand Surg 2007;32A:1343–1347.
6. Altay T, Kaya A, Karapinar L, Ozturk H, Kayali C. Is radial shortening useful for Lichtman stage 3B Kienböck’s disease? Int Orthop 2008;32:747–752.
7. Quenzer DE, Linscheid RL. Ulnar lengthening procedures. Hand Clin 1993;9:467– 474.
8. DeSmet L. Ulnar variance: facts and fiction review article. Acta Orthop Belg 1994;60:1–9.
9. Kam B, Topper SM, McLoughlin S, Liu Q. Wedge osteotomies of the radius for Kienböck’s disease: a biomechanical analysis. J Hand Surg 2002:27A:37– 42.
10. Hori Y, Tamai S, Okuda H, Sakamoto H, Takita T, Masuhara K. Blood vessel transplantation to bone. J Hand Surg 1979;4:23–33. 11. Moran SL, Cooney WP, Berger RA, Bishop AT, Shin AY. The use
of the 4⫹ 5 extensor compartmental vascularized bone graft for the treatment of Kienböck’s disease. J Hand Surg 2005;30A:50 –58. 12. Arora R, Lutz M, Deml C, Krappinger D, Zimmermann R, Gabl M.
Long-term subjective and radiological outcome after reconstruction of Kienböck’s disease stage 3 treated by a free vascularized iliac bone graft. J Hand Surg 2008;33A:175–181.
13. Wintman BI, Imbriglia JE, Buterbaugh GA, Hagberg WC. Operative treatment with radial shortening in Kienböck’s disease. Orthopedics 2001;24:365–371.
14. Watanabe T, Takahara M, Tsuchida H, Yamahara S, Kikuchi N, Ogino T. Long-term follow-up of radial shortening osteotomy for Kienböck disease. J Bone Joint Surg 2008;90A:1705–1711. 15. Almquist EE, Burns JF Jr. Radial shortening for the treatment of
Kienböck’s disease—a 5- to 10-year follow-up. J Hand Surg 1982; 7A:348 –352.
16. Botte MJ, Pacelli LL, Gelberman RH. Vascularity and osteonecrosis of the wrist. Orthop Clin North Am 2004;35:405– 421.
17. Khorbi A, Chebil M, Kanoune ML, Haddad N, Ben Maitigue M, Hachem A. Use of radial shortening for Kienböck disease. Tunis Med 2005;83:467– 472.
18. Wintman BI, Imbriglia JE. Operative treatment with radial shorten-ing in Kienböck’s disease. Thorofare 2001;24:365–367.
19. Castro FP Jr, Barrack RL. Core decompression and conservative treatment for avascular necrosis of the femoral head: a meta-analysis. Am J Orthop 2000;29:187–194.
20. Illarramendi AA. The surgical treatment of Kienböck disease by radius and ulna metaphyseal core decompression, J Hand Surg 2001;26A:252–259.
TABLE 1. Results of Lunate Core Decompression
Physical Examination Findings P Value Preoperative Postoperative Extension 18⫾ 2 72⫾ 3.5 ⬍.001 Flexion 30⫾ 4 45⫾ 4 ⬍.050 Radial deviation 8⫾ 1.5 18⫾ 2 ⬍.010 Ulnar deviation 14⫾ 2 30⫾ 1 ⬍.010 Lunate tenderness (%) 90 15 ⬍.001 Visual analog scale 87.5 13.5 ⬍.001 Disabilities of the Arm,
Shoulder, and Hand score
84 14 ⬍.001
LUNATE CORE DECOMPRESSION 1677
JHS䉬VolA, October
Downloaded for Anonymous User (n/a) at Ufuk Universitesi from ClinicalKey.com by Elsevier on August 01, 2018. For personal use only. No other uses without permission. Copyright ©2018. Elsevier Inc. All rights reserved.