Vol. 21, No. 1, pp. 74/78
DOI: 10.1097/gme.0b013e318293761f
* 2013 by The North American Menopause Society
Collagen cross-links as a marker for subclinical atherosclerosis
in postmenopausal women
Gamze Sinem Caglar, MD,
1Inci Kahyaoglu, MD,
1Elif Didem Ozdemir, MD,
1Rabia Seker, MD,
2and Selda Demirtas, MD
2Abstract
Objective: This study aimed to examine the utility of pyridinoline (Pyd) and deoxypyridinoline (Dpd) cross-links in the detection of subclinical atherosclerosis in postmenopausal women with or without osteoporosis.
Methods: We measured Pyd, Dpd, carotid intima-media thickness (CIMT), fasting total cholesterol, triglycerides, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, and blood pressure in 59 healthy post-menopausal women: 30 had normal bone mineral density (group I) and the remaining 29 had osteoporosis or osteopenia (group II) according to World Health Organization criteria.
Results: There were no statistically significant differences in age, duration of menopause, age at menopause, lipid profile, body mass index, Pyd level, Dpd level, and Pyd-to-Dpd ratio between the groups (P9 0.05). No significant difference in CIMT was found when groups I and II were compared (P = 0.538). No statistically significant differences in Pyd level, Dpd level, and Pyd-to-Dpd ratio were found when women with CIMT higher than 5 mm and women with CIMT of 5 mm or less were compared in groups I and II (P9 0.05). However, significantly declined Dpd level and increased Pyd-to-Dpd ratio were found in women with CIMT higher than 5 mm when compared with women with CIMT of 5 mm or less. CIMT was found to be negatively correlated with Dpd level (r = j0.346, P = 0.007) and to be positively correlated with the Pyd-to-Dpd ratio (r = 0.702, PG 0.001).
Conclusions: The increase in the Pyd-to-Dpd ratio, irrespective of the participants’ bone mineral density, may have predictive value in the determination of subclinical atherosclerosis in postmenopausal women.
Key Words: Pyridinium cross-links Y Atherosclerosis Y Pyridinoline Y Deoxypyridinoline Y Carotid intima-media thickness.
C
ollagen is the main structural protein of human con-nective tissue. The tensile strength of collagen fibrils is maintained by intramolecular and intermolecular modifications. Stabilization of collagen is achieved through the formation of bifunctional intermediate cross-links by hy-droxylation of lysine residues through the action of lysyl oxidase, which are converted into more stable trifunctional cross-links by lysyl hydroxylase. Pyridinoline (Pyd) and deoxy-pyridinoline (Dpd) are two nonreducible collagen cross-links that are released to the circulation when collagen is degradedinto molecular fragments. Pyd is present predominantly in connective and cartilage tissues, whereas Dpd is mainly found in mineralized tissues such as bone and dentine.1,2The pyridinium cross-links Pyd and Dpd are well-characterized markers for bone resorption.1
In postmenopausal women, Pyd and Dpd are used to eval-uate osteoporosis and short-term treatment response. Research on the use of these markers as diagnostic tools for genetic disorders of collagen metabolism and bone diseases other than osteoporosis continues. Recently, maturation and degradation of collagen have been evaluated in atherosclerotic vascular tissue.3Pyd and Dpd cross-links of normal and atherosclerotic vascular tissues have shown differences in collagen matura-tion.3In carotid endarterectomy specimens, greater collagen deposition and increased Pyd-to-Dpd ratio were found in plaque versus normal vascular tissue.3 To our knowledge, measure-ment of Pyd and Dpd cross-links in normal and atherosclerotic vascular tissues has been performed by Hector et al.3Therefore, we hypothesized that pyridinium cross-links might be valuable for the evaluation and diagnosis of subclinical atherosclerosis. However, the clinical use of Pyd and Dpd cross-links in atherosclerosis has not been investigated. There is little in-formation to no inin-formation about the utility of Pyd, Dpd, or Pyd-to-Dpd ratio as a predictive measure of atherosclerosis.
Received November 26, 2012; revised and accepted March 18, 2013. From the Departments of1Obstetrics and Gynecology and2Biochemistry, Faculty of Medicine, University of Ufuk, Ankara, Turkey.
G.S.C. and E.D.O. collected, analyzed, and interpreted the data. I.K. con-tributed to data acquisition. G.S.C., I.K., and E.D.O. prepared the manu-script. S.D. and R.S. performed biochemical analyses on the serum and urine samples. All authors drafted and critically revised the manuscript for important intellectual content and approved the final version of the manuscript.
Funding/support: None.
Financial disclosure/conflicts of interest: None reported.
Address correspondence to: Gamze Sinem Caglar, MD, Department of Ob-stetrics and Gynecology, Faculty of Medicine, University of Ufuk, Mevlana BulvarN Balgat, Ankara 06520, Turkey. E-mail: gamzesinem@hotmail.com
A variety of screening tests are available to detect and treat subclinical atherosclerosis. Some of these screening tests, such as measurement of coronary artery calcification by CT scanning and measurement of carotid intima-media thickness (CIMT) and plaque by ultrasonography, have been available longer than others and are capable of providing direct evi-dence for the presence and extent of atherosclerosis. Both of these imaging methods provide prognostic information of proven value regarding the future risk of myocardial infarction and stroke.4 A meta-analysis of about 11 population-based studies (N = 54,336 women) demonstrated that increased CIMT shows diagnostic precision in predicting myocardial infarction (area under the curve = 0.61).5However, whether increased CIMT is able to support correct clinical decision-making and leads to specified antiatherosclerotic therapy is yet to be elu-cidated. Moreover, because of well-known histopathological mechanisms in the intima-media complex and calculated car-diovascular risks associated with increased CIMT, the ques-tion of CIMT interference via medical treatment arose in the last decade. The effect of different low-density lipoprotein cholesterol (LDL-C)Ylowering therapies on CIMT regression has been proven in different studies.6<9In women with CIMT less than 1 mm, no plaque (moderately high risk), lifestyle modifications, and an LDL-C target lower than 130 mg/dL (G3.37 mmol/L), as well as belonging to the 50th to 75th percentiles, targeting less than 100 mg/dL (G2.59 mmol/L) is optional. In women with CIMT of 1 mm or more, less than 50% stenosis (high risk), lifestyle modifications, and an LDL-C target lower than 100 mg/dL (G2.59 mmol/L), as well as belonging to higher than the 75th percentile, targeting less than 70 mg/dL (G1.82 mmol/L) is optional.10
As a result, this study planned to examine the utility of Pyd and Dpd cross-links for the detection of subclinical atheroscle-rosis in postmenopausal women with or without osteopoatheroscle-rosis.
METHODS
The participants of the study were healthy postmeno-pausal women who were followed at a gynecology clinic of a university hospital (N = 59). The exclusion criteria for all women were as follows: hypogonadism, hyperparathyroid-ism, thyroid dysfunction, chronic liver disease, chronic renal disease, malabsorption, malnutrition, diabetes mellitus, alco-hol consumption, Cushing syndrome, and any other diseases that can cause secondary osteoporosis. All participants were nonsmokers. Women treated for osteoporosis or those receiv-ing hormone therapy were also excluded from the study as well as women who had ever used antiepileptic, corticosteroid, and anticoagulant drugs.
Blood samples were obtained in the morning after an over-night fast for at least 12 hours. Fasting blood was drawn for glucose and lipid profile (total cholesterol, triglycerides [TG], high-density lipoprotein cholesterol [HDL-C], and LDL-C). Plasma glucose was determined with the glucose hexokinase method (Cobas Integra 400 Plus; Roche Diagnostics, Mann-heim, Germany). Total cholesterol, HDL-C, LDL-C, and TG
were measured by enzymatic calorimetric assays (Roche Di-agnostics). The intra-assay and interassay coefficients of varia-tion were less than 1.9% and less than 4%, respectively, for all assays performed. Blood pressure was measured by the same trained nurse on the same visit. After a 5-minute rest, blood pressure was measured on the right arm of the seated participant using a sphygmomanometer with an appropriate-sized cuff. Hypertension was defined as a blood pressure of 140/90 mm Hg or higher or the use of antihypertensive medi-cations. Lipid profile values were considered abnormal if total serum cholesterol was greater than 200 mg/dL, serum TG was greater than 250 mg/dL, LDL-C was higher than 100 mg/dL, and HDL-C was lower than 40 mg/dL.
Morning urine samples were collected for pyridinium cross-links after an overnight fast to avoid the influences of circadian rhythm. Pyd and Dpd were measured by high-performance liquid chromatography (HPLC) using a commercially available assay (Chromosystems Instruments and Chemicals, Munich, Germany). Pyd-to-Dpd ratios were calculated.
Bone mineral density (BMD; g/cm3) was measured at the lumbar spine (L1-L4), femoral neck, greater trochanter, and Ward’s triangle using dual-energy x-ray absorptiometry (GE Healthcare DPX Duo). Femoral neck BMD was measured at the narrowest point of the femoral neck and perpendicular to the femoral midline. Spine BMD was measured in the anteroposterior view and was the mean of four lumbar verte-brae (L1-L4). All bone scans were administered by the same radiology technician to eliminate discrepancies. Normal BMD, osteopenia, and osteoporosis were defined according to World Health Organization criteria.11Among the participants, 30 women were considered to have normal BMD (group I), and the re-maining 29 women had osteoporosis or osteopenia (group II) according to World Health Organization criteria.
Common CIMT was conducted using a high-resolution ultrasound machine. The posterior carotid wall at 1 cm of the common carotid artery was imaged in B-mode, and CIMT was estimated by a visual assessment of the distance between the lumen-intima interface and the intima-adventitia interface in longitudinal frames acquired during arterial diastole.12 The mean of CIMT measurements made at the greatest thickness on both sides was used for statistical analyses. Ultrasono-graphic measurements were performed by the same experi-enced radiologist. To define subclinical atherosclerosis, we used a 50th percentile cutoff value (0.5 mm) for white women aged 45 to 54 years.13
Statistical analysis
Data analysis was performed using SPSS for Windows, version 11.5 (SPSS Inc., Chicago, IL). Whether or not the distributions of continuous variables were normal was deter-mined by Shapiro-Wilk test. Continuous variables were pre-sented as mean (SD) or median (min-max), where applicable. Although the mean differences between groups were compared with Student’s t test, Mann-Whitney U test was applied to compare the median values. Categorical data were analyzed by Pearson’sW2test. Degrees of associations between continuous
variables were analyzed by Spearman’s rank correlation test. PG 0.05 was considered statistically significant.
RESULTS
Demographic characteristics and the prevalence of hyper-tension and hyperlipidemia in groups I and II are presented in Table 1. The mean duration of menopause was 5 years (range, 1-23 y). Among the participants of the study, 44% had hyper-tension and 54% had hyperlipidemia. The mean (SD) fasting plasma glucose level was 97.8 (9.1) and 95.8 (8.8) mg/dL in groups I and II, respectively (P = 0.393). The values for lipid profile, Pyd, and Dpd in all women and groups are given in Table 2. The mean (SD) CIMT was 0.65 (0.10) mm, and the mean (SD) intraobserver variability of the ultrasonographer was 0.13 (0.10) mm for the mean CIMT. No significant dif-ference in CIMT was found when groups I and II were com-pared (Table 2). Subclinical atherosclerosis (CIMT9 0.5 mm) was detected in 24 women in group I and in 25 women in group II (P = 0.731).
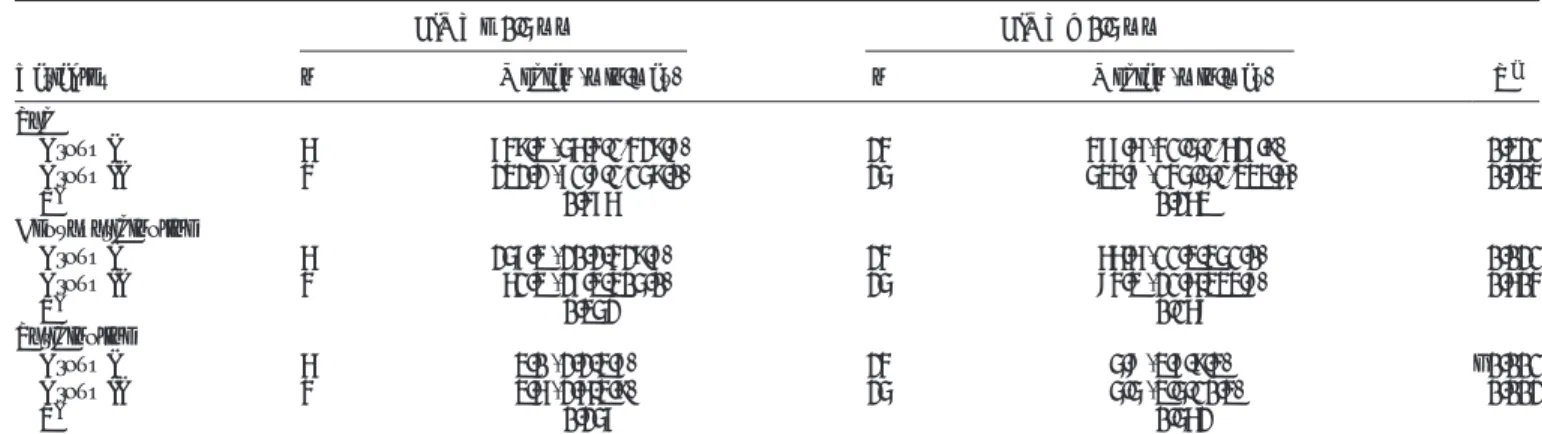
Pyd, Dpd, and calculated ratios were further analyzed for the CIMT of groups I and II (Table 3). When women with in-creased (90.5 mm) CIMT in groups I and II were compared for Pyd, Dpd, and Pyd-to-Dpd ratio, no statistically significant difference was found (P9 0.05). Similar to this result, women with CIMT of 0.5 mm or less in groups I and II also had no differences in Pyd, Dpd, and Pyd-to-Dpd ratio (P 9 0.05). However, significantly declined levels of Dpd and increased Pyd-to-Dpd ratio were found in women with CIMT higher than 0.5 mm when compared with women with CIMT of 0.5 mm or less (Table 3). According to Spearman’s rank correlation analyses, CIMT was found to be negatively correlated with
Dpd values (r = j0.346, P = 0.007) and to be positively cor-related with the Pyd-to-Dpd ratio (r = 0.702, PG 0.001).
DISCUSSION
Atherosclerosis is a chronic inflammatory reaction of the vascular wall to dyslipidemia and endothelial distress in-volving the inflammatory recruitment of leukocytes and the activation of resident vascular cells.14 Chronic inflammation of the arterial vascular wall leads to multifocal plaque devel-opment.15,16After the oxidation of cholesterol particles in the intima of vessels, macrophages, which become foam cells, further stimulate the inflammatory process. Previously, a link between inflammation and attenuated collagen cross-link mat-uration in plaques has been shown.17In addition, Hector et al3 directly measured mature collagen cross-links in plaques and showed that plaque tissue had less Dpd than either the under-lying media or the normal arterial wall.3Consequently, plaque tissue had a higher Pyd-to-Dpd ratio than both the underlying media and the normal tissue.3Similarly, the results of our study demonstrated significantly declined Dpd levels and increased Pyd-to-Dpd ratio in the urine samples of women with subclin-ical atherosclerosis (CIMT 9 0.5 mm) (Fig. 1). In addition, CIMT was found to be negatively correlated with Dpd values and to be positively correlated with the Pyd-to-Dpd ratio.
CIMT is an established marker for early structural athero-sclerotic disease, and CIMT measurements provide a com-prehensive noninvasive assessment of arterial structure and function and an assessment of early cardiovascular disease. Increased CIMT is correlated with atherosclerotic vascular disease, such as coronary artery disease and stroke, and pre-dicts future vascular events after other conventional vascular
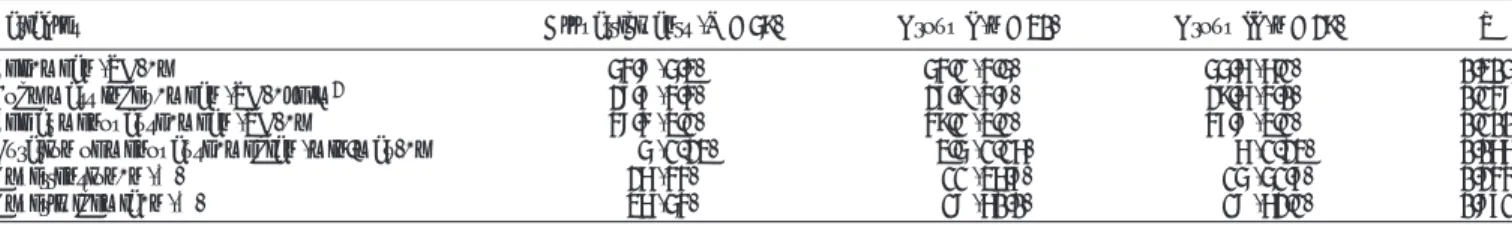
TABLE 1. Demographic and clinical characteristics of all participants, group I, and group II
Variables All participants (N = 59) Group I (n = 30) Group II (n = 29) P
Age, mean (SD), y 54.8 (5.3) 54.1 (4.5) 55.6 (6.1) 0.305
Body mass index, mean (SD), kg/m2 28.7 (4.4) 27.9 (4.8) 29.6 (4.0) 0.148
Age at menopause, mean (SD), y 48.4 (3.1) 49.1 (3.1) 47.8 (3.1) 0.100
Duration of menopause, median (min-max), y 5 (1-23) 3.5 (1-16) 6 (1-23) 0.066
Hypertension, n (%) 26 (44) 11 (36.7) 15 (51.7) 0.244
Hyperlipidemia, n (%) 36 (54) 18 (60.0) 18 (62.1) 0.871
TABLE 2. Results of lipid profile , pyridinium cross-links, and CIMT all women, group I, and group II
Variables All women (N = 59) Group I (n = 30) Group II (n = 29) P
TC, mg/dL 209 (60-375) 217 (159-375) 207 (60-300) 0.544
LDL-C, mg/dL 162 (48-288) 161 (89-288) 164 (48-243) 0.575
HDL-C, mg/dL 52 (36-131) 55 (38-81) 50 (36-131) 0.539
TG, mg/dL 118 (37-259) 119 (37-259) 115 (53-239) 0.744
Pyd,Hmol/mol creatinine 518 (41-1,627) 508 (41-1,627) 519 (71-1,333) 0.773
Dpd,Hmol/mol creatinine 84 (11-429) 81 (11-429) 84 (21-333) 0.750
Pyd-to-Dpd ratio 5.3 (2.1-10.3) 5.5 (2.2-9.3) 5.1 (2.6-10.3) 0.964
CIMT, mm 0.65 (0.50-0.90) 0.66 (0.50-0.85) 0.65 (0.50-0.90) 0.538
Data are presented as median (min-max).
CIMT, carotid intima-media thickness; TC, total cholesterol; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol; TG, triglycerides; Pyd, pyridinoline; Dpd, deoxypyridinoline.
risk factors have been adjusted in the general population.18 Classification of CIMT values varies considerably depending on the CIMT measurement protocol. Therefore, fixed cutoff values or percentile distributions are used to evaluate CIMT values.10 Moreover, similar to other markers for subclinical atherosclerosis, CIMT increases with age. Therefore, sex- and aged-stratified CIMT values are reasonably provided. In this study, 50th percentile was used to define subclinical athero-sclerosis in white women aged 45 to 54 years, as our study population has a mean age of 54 years.13
During the process of atherosclerosis, smooth muscle cells migrating from the medial layer to the intimal layer of the arterial wall proliferate and, by producing collagen, form a fibrous cap overlying the atheroma.19 Fibrosis causes an in-creased formation of hydroxyallysine cross-links, resulting in irreversible accumulation of collagen.20,21In vascular tissue, the major pathway for collagen stabilization is via telopeptide hydroxylysine aldehydes, resulting in the formation primarily of the pyridinium cross-links Pyd and Dpd.22,23 Lysyl hy-droxylase is consistently high in severe forms of fibrosis21; in vascular tissue, the Pyd-to-Dpd ratio is an indicator of lysyl hydroxylase activity.3Therefore, the Pyd-to-Dpd ratio can be a valuable marker for detecting the collagen content of the atherosclerotic lesions of vessel walls. In our study, the Pyd-to-Dpd ratio detected from morning urine samples was higher than 5 among women with increased CIMT. In the study by Hector et al,3women with coronary heart disease (CHD) had significantly higher Pyd-to-Dpd ratios (17.34 [8.38-37.79]) in vascular tissue samples than women without CHD (12.87 [11.22-16.67], P = 0.0218). A significantly higher Pyd-to-Dpd ratio in the vascular tissue of women with CHD needs to be evaluated with urine samples to clarify any detectable change in urine as in our study. Studies using alternative sources of biomarker discovery for the progression of atherosclerotic dis-ease are ongoing. Therefore, even a higher Pyd-to-Dpd ratio in women with CHD necessitates further research of clinical value regarding the pyridinium cross-links for atherosclerotic disease. After that, a valuable cutoff value for the Pyd-to-Dpd ratio can be determined. If future studies confirm our results, then a
Pyd-to-Dpd ratio higher than 5 might be valuable for discrimi-nating cardiovascular high-risk populations.
Approximately 60% of the pyridinium cross-links are ex-creted in urine in peptide-bound form and in free form (40%).24 Both Pyd and Dpd can be measured in urine by HPLC (total cross-link) or immunoassay (free cross-link).24The automated HPLC used in this study is a precise and convenient method for measuring Pyd and Dpd in urine samples.1The analytical and clinical performance of Pyd and Dpd cross-links by HPLC has to be established to determine the Pyd-to-Dpd ratio in post-menopausal women.
The measurement of Dpd and Pyd cross-link concentrations has clinical value in enabling the identification of increased bone resorption in metabolic bone diseases.1In our study, the Pyd-to-Dpd ratio is found to be increased in women with
TABLE 3. Pyd, Dpd, and Pyd-to-Dpd ratio in the groups in relation to CIMT
Variables
CIMT e 0.5 mm CIMT9 0.5 mm
Pa
n Median (min-max) n Median (min-max)
Pyd Group I 6 749.3 (56.4-1,429.8) 24 477.6 (41.5-1,627.9) 0.321 Group II 4 232.2 (71.8-1,159.0) 25 534.7 (145.5-1,333.6) 0.203 Pb 0.476 0.263 Deoxypyridinoline Group I 6 257.3 (20.2-429.7) 24 66.6 (11.3-351.0) 0.021 Group II 4 61.3 (27.3-305.0) 25 84.3 (21.6-333.8) 0.604 Pb 0.352 0.168 Pyridinoline Group I 6 3.0 (2.2-3.7) 24 5.8 (3.7-9.3) G0.001 Group II 4 3.6 (2.6-3.9) 25 5.5 (3.5-10.3) 0.002 Pb 0.257 0.562
Pyd, pyridinoline; Dpd, deoxypyridinoline; CIMT, carotid intima-media thickness. Bold values are statistically significant.
a
Comparisons between CIMT levels within groups. b
Comparisons between groups I and II within CIMT levels.
FIG. 1. Ratio of pyridinoline (Pyd) to deoxypyridinoline (Dpd) according to carotid intima-media thickness (CIMT) levels in group I (PG 0.001) and group II (P = 0.002).
CIMT higher than 0.5 mm, irrespective of BMD results. The increase in the Pyd-to-Dpd ratio, irrespective of the BMD status of the participants, may be an indicator of subclinical atherosclerosis in postmenopausal women.
CONCLUSIONS
The urine samples of postmenopausal women with sub-clinical atherosclerosis (CIMT9 0.5 mm) show significantly declined levels of Dpd and increased Pyd-to-Dpd ratio irrespec-tive of BMD status. In addition, CIMT is found to be negairrespec-tively correlated with Dpd values and to be positively correlated with the Pyd-to-Dpd ratio. The Pyd-to-Dpd ratio from urine can be used as a valuable marker for detecting subclinical atheroscle-rotic lesions.
Acknowledgments: We wish to thank all women for their partici-pation in this study and all personnel at the Department of Obstetrics and Gynecology for their enthusiastic contribution.
REFERENCES
1. Kraenzlin ME, Kraenzlin CA, Meier C, Giunta C, Steinmann B. Auto-mated HPLC assay for urinary collagen cross-links: effect of age, men-opause, and metabolic bone diseases. Clin Chem 2008;54:1546-1553. 2. Mu¨ller A, Jakob K, Hein GE. Evaluation of free and peptide bound
col-lagen crosslink excretion in different skeletal diseases. Ann Rheum Dis 2003;62:65-67.
3. Hector EE, Robins SP, Mercer DK, Brittenden J, Wainwright CL. Quan-titative measurement of mature collagen cross-links in human carotid artery plaques. Atherosclerosis 2010;211:471-474.
4. Naghavi M, Falk E, Hecht HS, et al. SHAPE Task Force. From vulner-able plaque to vulnervulner-able patient, 3: executive summary of the Screening for Heart Attack Prevention and Education (SHAPE) Task Force report. Am J Cardiol 2006;98:2H-15H.
5. Inaba Y, Chen JA, Bergmann SR. Carotid plaque, compared with carotid intima media-thickness, more accurately predicts coronary artery disease events: a meta-analysis. Atherosclerosis 2012;220:128-133.
6. Crouse JR III, Raichlen JS, Riley WA, et al. Effect of rosuvastatin on progression of carotid intima-media thickness in low risk individuals with subclinical atherosclerosis: the METEOR Trial. JAMA 2007;298: 1344-1353.
7. Salonen R, Nyysso¨nen K, Porkkala E, et al. Kuopio Atherosclerosis Prevention Study (KAPS). A population-based primary preventive trial
of the effect of LDL lowering on atherosclerotic progression in carotid and femoral arteries. Circulation 1995;92:1758-1764.
8. Hodis HN, Mack WJ, LaBree L, et al. Reduction in carotid arterial wall thickness using lovastatin and dietary therapy: a randomized controlled trial. Ann Intern Med 1996;124:548-556.
9. de Groot E, Jukema JW, van Boven AJ, et al. Effect of pravastatin on progression and regression of coronary atherosclerosis and vessel wall changes in carotid and femoral arteries: a report from the Regression Growth Evaluation Statin Study. Am J Cardiol 1995;76:40C-46C. 10. Bauer M, Caviezel S, Teynor A, Erbel R, Mahabadi AA,
Schmidt-Trucksa¨ss A. Carotid intima-media thickness as a biomarker of subclinical atherosclerosis. Swiss Med Wkly 2012;142:w13705.
11. Kanis JA, Melton LJ III, Christiansen C, Johnston CC, Khaltaev N. The diagnosis of osteoporosis. J Bone Miner Res 1994;9:1137-1141. 12. Pignoli P, Tremoli E, Poli A, Oreste P, Paoletti R. Intimal plus medial
thickness of the arterial wall: a direct measurement with ultrasound im-aging. Circulation 1986;74:1399-1406.
13. Stein JH, Korcarz CE, Hurst RT, et al. Use of carotid ultrasound to identify subclinical vascular disease and evaluate cardiovascular disease risk: a consensus statement from the American Society of Echocardiography Ca-rotid Intima-Media Thickness Task Force. J Am Soc Echocardiogr 2008; 21:93-111.
14. Libby P. Inflammation in atherosclerosis. Nature 2002;420:868-874. 15. Hansson GK. Inflammation, atherosclerosis, and coronary artery disease.
N Engl J Med 2005;352:1685-1695.
16. Davies MJ. The pathophysiology of acute coronary syndromes. Heart 2000;83:361-366.
17. Ovchinnikova O, Robertson AK, Wagsater D, et al. T-cell activation leads to reduced collagen maturation in atherosclerotic plaques of ApoE(j/j)mice. Am J Pathol 2009;174:693-700.
18. Kong X, Jia X, Wei Y, et al. Association between microalbuminuria and subclinical atherosclerosis evaluated by carotid artery intima-media in elderly patients with normal renal function. BMC Nephrol 2012;13:37. 19. van Lammeren G, Moll F, Borst GJ, de Kleijn DP, de Vries JP,
Pasterkamp G. Atherosclerotic plaque biomarkers: beyond the horizon of the vulnerable plaque. Curr Cardiol Rev 2011;7:22-27.
20. Ricard-Blum S, Bresson-Hadni S, Vuitton DA, Ville G, Grimaud JA. Hydroxypyridinium collagen cross-links in human liver fibrosis: study of alveolar echinococcosis. Hepatology 1992;15:599-602.
21. van der Slot AJ, Zuurmond AM, van den Bogaerdt AJ, et al. Increased for-mation of pyridinoline cross-links due to higher telopeptide lysyl hydroxylase levels is a general fibrotic phenomenon. Matrix Biol 2004;23:251-257. 22. Robins SP, Duncan A. Cross-linking of collagen. Location of pyridinoline
in bovine articular cartilage at two sites of the molecule. Biochem J 1983;215:175-182.
23. Ogawa T, Ono T, Tsuda M, Kawanishi Y. A novel fluor in insoluble collagen: a crosslinking moiety in collagen molecule. Biochem Biophys Res Commun 1982;107:1252-1257.
24. Simsek B, Karacaer O, Karaca I. Urine products of bone breakdown as markers of bone resorption and clinical usefulness of urinary hydroxy-proline: an overview. Chin Med J 2004;117:291-295.