2011 by the American Orthopaedic Foot & Ankle Society DOI: 10.3113/FAI.2011.0414
Stabilization of Chevron Bunionectomy with a Capsuloperiosteal Flap
Berk Guclu, MD; Alper Kaya, MD; Burak Akan, MD; Murat Koken, MD; Ali Kemal Us, MD
Ankara, Turkey
ABSTRACT
Background: Distal chevron osteotomy (DCO) for mild to moderate hallux valgus deformity is inherently more stable than the other forms of distal metatarsal osteotomy, but complications such as loss of correction, infection, joint stiffness, delayed union, malunion and nonunion can occur. In this study, we evaluated the use of a capsuloperiosteal flap for stabilization of DCO in the treatment of hallux valgus. Materials and Methods: A retrospective study was conducted on 59 patients (88 feet) that underwent distal Chevron osteotomy stabilized only with a capsuloperiosteal flap for mild and moderate hallux valgus deformity with a mean followup of 11.3 years. Clinical evaluation was calculated using the hallux score of the American Orthopaedic Foot and Ankle Society (AOFAS). Results: The score improved from a preoperative mean of 52 to a mean of 91.5 points at last followup. Average hallux valgus angle changed from 30.3 degrees preoperatively to 14.2 degrees postoperatively at the last followup. Intermetatarsal angle 1–2 changed from 13.6 degrees preoperatively to 10.2 degrees postoperatively. The correction proved to be consistent with only an average of 3.4-degree correction loss and 4.9-degree loss in the range of motion. Eighty-six feet (97.7%) were pain free. Discomfort with shoewear was absent in 84 feet (95.5%) postoperatively and 24 of 25 (96%) patients were satisfied cosmetically. Conclusion: Capsuloperiosteal flap stabilization of distal chevron osteotomy for mild-moderate hallux valgus yielded excellent clinical results at long-term followup. Level of Evidence: IV, Retrospective Case Series
Key Words: Chevron; Hallux Valgus; Modification; Osteotomy
No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Corresponding Author: Berk Guclu, Assistant Professor
Ufuk University, Orthopaedics and Traumatology Mevlana Bulv (Konya yolu) no 86-88 Balgat, Ankara
Turkey
E-mail: gucluberk@yahoo.com
For information on pricings and availability of reprints, call 410-494-4994, x232.
INTRODUCTION
The most widely used procedure for mild and moderate cases of hallux valgus is the Chevron modification of the Mitchell osteotomy.1–2 Chevron procedure is frequently accompanied by either internal fixation of the osteotomized fragments or application of short leg cast postoperatively.9 The senior author has used the method of capsuloperiosteal flap for stabilization and no other internal fixation material or method and no cast has been used postoperatively.14 Symp-tomatic hallux valgus associated with a first intermetatarsal angle of less than 15 degrees is typically corrected with a modified chevron osteotomy when nonoperative treatment fails. The aim of our study was to evaluate clinical and radio-graphic results of a substantial number of patients with a longer followup.
MATERIALS AND METHODS
Between 1994 and 2000 a total of 96 chevron osteotomies were performed in 65 patients. A total of 59 patients (88 feet) with a minimum followup of 10 years were available for clinical and radiographic analysis. Six patients had moved and were lost to followup. The mean followup was 11.3 (range, 10.2 to 16.1) years. There were 51 women (80 feet) and eight men (eight feet). The mean age at the time of surgery was 37.8 (range, 19.2 to 51.5) years.
Pain was the chief complaint, and the indications for surgery were failed conservative treatment, first to second inter-metatarsal angle less than 15 degrees, hallux valgus angle less than 40 degrees, and the absence of degenerative changes of the first metatarsophalangeal joint.
On physical examination, feet were checked for presence of callosities and second toe deformities. Range of motion of the first metatarsophalangeal joint and presence of pain with movement were recorded. Standard radiographic standing AP and lateral X-rays were taken. The radiographs were repeated on the first postoperative day, 6th postoperative week, 6th postoperative month, first year, then annually until the 5th postoperative year and then every 5th year.
Postoperative followup criteria were measured using the American Orthopaedic Foot and Ankle Society hallux scale.8,13
Intermetatarsal 1 – 2 angle, hallux valgus angle, and rela-tive lengths of the first and second metatarsals were measured.5 Medial, central, or lateral position of the tibial sesamoid and subluxation of the first metatarsophalangeal joint were determined.
Surgical technique
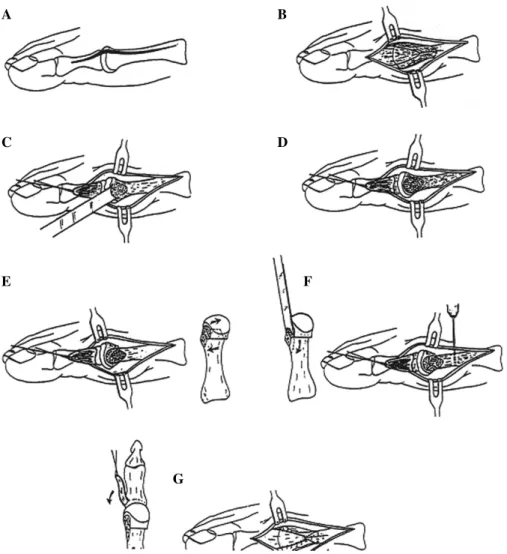
The surgical technique has been described in a previous report.4 The procedure was held under selective spinal
anes-thesia to prevent the pain related to the pneumatic tourniquet applied to ipsilateral thigh. A dorsomedial longitudinal skin incision was followed by a Y-shaped capsulotomy. A capsu-loperiosteal flap was elevated by sharp dissection, exposing the first metatarsophalangeal joint. The bunion was excised starting from the parasagittal groove aiming proximally and medially. A V-shaped metatarsal distal osteotomy with a 60-degree angle and its apex at the center of the metatarsal head was made. The distal fragment was lateralized approximately
one-third the thickness of the metatarsal head and the medial cortical spike was excised. A bicortical canal-drill hole with a 2.5-mm drill was made starting dorsally proceeding plan-tarward just proximal to the V-osteotomy. While holding the hallux in the desired position, strong absorbable sutures (No. 2 vicryl) were passed through this canal to attach the apex of the V-shaped capsuloperiosteal flap to the bone. Manu-ally, the stability of the osteotomy was checked by directly observing passive range of motion. No internal fixation was required. An AP and lateral radiograph or fluoroscan of the joint in the operating room was obtained. Then the layers were closed using absorbable sutures. Night splint and a bulky bandage were applied for the first night. The dressing was changed the next day and the night splint and elastic bandage were applied for the next 4 to 6 weeks. The patients were encouraged to walk as soon as they could tolerate on their heel with a hallux valgus shoe. The splint was kept for 6 weeks until a solid union was obtained. For the bilateral cases, the second procedure was performed a mean of 9.8 (range, 6 – 12) weeks after the first operation (Figure 1).
A B
C D
E F
G
Fig. 1: Illustration of the modified distal chevron procedure and capsuloperiosteal flap stabilization (image originally appeared in The Journal of Foot and
A B
C D
Fig. 2: X-ray examples for hallux valgus. A and B, A 34-year-old female at the time of operation, right hallux valgus with preoperative AOFAS score: 44
pts to postoperative 95 pts at the last followup, preoperative (A) HVA:31◦ IMA1−2:11◦; 11-year postoperative (B) followup with HVA: 17◦, IMA1−2:11◦.
C and D, A 29-year-old male, right hallux valgus with preoperative AOFAS score:42 pts. To postoperative AOFAS score:90 pts. Preoperative (C) HVA:30◦
IMA1−2:12◦to postoperative (D) 13-year followup HVA: 13◦IMA1−2:10◦.
RESULTS
The primary complaint of all patients was pain. All patients also had discomfort in shoes. Twenty-four (27.3%) patients complained of symptomatic plantar keratosis beneath the second metatarsal head. Twenty-five (28.4%) patients were dissatisfied with the appearance of their first toe.
Physical examination revealed an average range of motion (combined dorsi- and plantarflexion) of the first MTP joint of 74.7 (range, 30 to 130) degrees preoperatively. At the last followup, range of motion of the first metatarsophalangeal joint was found to have an average 69.9 (range, 25 to 125) degrees. On average, 4.8 degrees of motion was lost after surgery (Figure 2).
Average correction of the intermetatarsal angle 1 – 2 was 3.4 degrees [preoperative mean value 13.6 (range, 8 to 17) degrees to postoperative mean value of 10.2 (range, 7 to 14) degrees]. The mean first MTP angle improved from 30.3 (range, 24 to 44) degrees to 14.2 (range,−4 to 18) degrees with a mean of 16.1-degree correction (Table 1).
On the immediate postoperative radiographs, it was evident that 46 of the 49 laterally located sesamoids were repositioned to normal anatomic location. Radiographic assessment revealed 41 of 88 had subluxation of the first MTP joint preoperatively which 40 had (97.9%) regained normal anatomic congruency postoperatively. Average hospi-talization time was 2 (range, 1 to 7) days. At the 6th week, all
cases had radiographic evidence of union of the osteotomies. All patients returned to work before the 6th postoperative week except 11 (18.6%) who required an extra 2 weeks of rest.
At the last followup examination, patients were asked to answer a series of questions concerning relief of their complaints. Eighty-six (97.7%) of the 88 feet were pain free. The other two patients who had bilateral operations complained of improved but occasional pain in one of their feet. Discomfort with shoewear was absent in 84 (95.5%) feet, improved in four, and was still present in two (2.3%). In general our patients had started to wear conventional wide shoes at the 6th postoperative week and fashionable shoes without any insert or modification at a mean of 12 weeks after surgery (range, 11 to 15 weeks).
Twenty-four out of 25 patients who were uncomfortable about the sight of their foot were satisfied cosmetically after the procedure. All of the patients who had metatarsalgia were pain free within the first 6 months followup. Of the 42 callosities, 40 resolved while two persisted. Four (4.5%) of the patients developed excessive early postoperative swelling.
We did not encounter any recurrence of deformity, malu-nion, delayed umalu-nion, nonunion or comminution of the frag-ments. Dysesthesia or hypoesthesia was present at the inci-sion site of two (2.3%). One of the cases had a stiff MTP
Ta b le 1 : Clinical and R adiographic D ata o f 8 8 F eet with Followup A fter 5 – 11, 3 Y ears Pr e-operative Level o f significance ∗ First followup mean 5 y ears Level o f significance ∗ Second followup mean 11, 3 y ears AOF AS † hallux score 52 (20 to 70) P < 0.001 89.7 (52 to 100) ns 91.5 (52 to 100) AOF AS score -pain 10.45 (0 to 20) P < 0.001 30.3 (0 to 40) ns 30.7 (0 to 40) AOF AS score -function 26.4 (19 to 40) P < 0.001 38.1 (29 to 45) ns 38.7 (29 to 45) AOF AS score -alignment 4 .6 (0 to 15) P < 0.001 12.4 (0 to 15) ns 12.8 (0 to 15) MTP ‡ range of motion( ◦ ) (dorsiflexion + plantarflexion) 74.7 ◦ (30 ◦ to 130 ◦ ) n s 71.6 ◦ (30 ◦ to 130) ns 69.9 ◦ (25 ◦ to 125 ◦ ) MTP angle 30.3 ◦ (24 ◦ to 44 ◦ ) 13.4 ◦ (− 5 ◦ to 19 ◦ ) 14.2 ◦ (− 9 ◦ to 18 ◦ ) IM ‡ angle 13.6 ◦ (8 ◦ to 17 ◦ )9 .6 ◦ (6 ◦ to 14 ◦ ) 10.2 ◦ (7 to 14) Relative length o f m etatarsals 1 – 2 0 mm − 1.7 m m − 1.6 m m ( − 4m m to + 5 mm) a ( − 6m m to + 3 mm) a ( − 6m m to + 3.3 mm) a ∗Significance levels refer to d if ferences between the two followup inve stigations preoperative as se ss m ent, 5 and 11, 3 y ears after su rg ery. B onferroni adjus ted W ilcoxon si gn rank tes t, n s: non-s ignificant. † A merican Orthopaedic Foot and A nkle S ociety. ‡ M TP; m etatars ophalangeal, IM; intermetatars al. aNegative v alue indicates firs t metatars al is shorter than the second.
joint which did not bother the patient. On the radiographs taken at last followup, two cases had increased density of the metatarsal head without any sign of osteoarthritis. One case developed cystic changes of the metatarsal head without degenerative changes. No apparent avascular necrosis of the metatarsal head was observed. There were four (4.5%) cases of superficial infection during the first postoperative month which resolved with antibiotics.
DISCUSSION
Among the many techniques for the treatment of hallux valgus, the chevron procedure has gained a wide acceptance for its ease, reliability and effectiveness. First described by Corless and then by Johnson3,7 modifications have been suggested to improve minor disadvantages of this procedure. The osteotomy line has been carried proximally for better stability, more bony contact, less joint stiffness, and for being able to correct more severe deformities. Internal fixation with two Kirschner wires or screws has been recommended. Some authors recommend postoperative casting to avoid complications related to internal fixation like pin tract infections, loss of stabilization, soft tissue irritation, migration of wires, pain around wires, and stress shielding effect on bone.4,15 Some authors prefer to use neither, but may experience greater rate of correction loss. Casting has been shown to decrease the rate of lost correction; however, in addition to the discomfort, casting has been shown to increase the metatarsophalangeal stiffness.9 In contrast to the stiffness rates between 4.8% and 42% reported in the literature6,11 the authors observed only one case with range of motion loss greater than 30 degrees. With the use of night splints only, easier rehabilitation after complete union occurred. In a series by Klosok et al.9average return to work time was 7 weeks. Forty-eight patients (81.4%) were able to start working before the 6th postoperative week in this series. As one of the most common complications of surgically treated hallux valgus, loss of correction and recurrence of the deformity are reported around 10% in the literature.9,11 We
have observed an average of 3.4-degree correction loss and no recurrence in followup examinations. Other complications occasionally seen such as malunion, delayed union, nonunion or comminution of the fragments were also prevented to a greater extend by better stabilization and compression. By suturing the distal capsular flap to bone, stable fixation of the osteotomized fragments was achieved. We believe compression provided by the capsular attachment to the metatarsal helped achieve solid union.
Adductor or lateral capsular release was not performed because the desired correction was achieved with proximal
advancement of the medial capsular flap. As Resch et al.12
have proposed, adductor release adds an irrelevant amount to correction. Also, carrying out more soft tissue release increases the risk of avascular necrosis.10By advancing the
capsular flap medially and attaching it to the medial shaft, we believe more correction, better stabilization, promotion of union by compression, and better maintenance of correction can be achieved. We believe avoiding internal fixation and cast application decreased complications and increases patient tolerance.
REFERENCES
1. Austin, DW; Leventen, EO: A new osteotomy for hallux valgus: a horizontally directed “V” displacement osteotomy of the metatarsal head for hallux valgus and primus varus. Clin Orthop. 157:25 – 30, 1981. 2. Bargman, J; Corless, J; Gross, AE; Lange, F: A review of surgical
procedures for hallux valgus. Foot and Ankle. 1:39 – 43, 1980. 3. Corless, JR: A modification of the Mitchell Procedure. J Bone Joint
Surg. 58-B:138, 1976.
4. Halpern, FP; Trepal, MJ; Hodge, W: Contamination and infection rate of percutaneous Kirschner wires in foot surgery. J Am Podiatr Med Assoc. 80(8):433 – 437, 1990.
5. Hardy, RH; Clapham, JCR: Observations on hallux valgus; based on a controlled series. J Bone Joint Surg Br. 33-B(3):376 – 91, 1951. 6. Johnson, JE; Clanton, TO; Baxter, DE; Gottlieb, MS: Comparison of
Chevron osteotomy and modified McBride bunionectomy for correction of mild to moderate hallux valgus deformity. Foot Ankle. 12(2):61 – 8, 1991.
7. Johnson, KA; Cofield, RH; Morrey, BF: Chevron osteotomy for hallux valgus. Clin Orthop Relat Res. (142):44 – 7, 1979.
8. Kitaoka, HB; Alexander, IJ; Adelaar, RS; et al.: Clinical rating systems for the ankle-hindfoot, midfoot, hallux, and lesser toes. Foot Ankle Int. 15(7):349 – 53, 1994.
9. Klosok, JK; Pring, DJ; Jessop, JH; Maffuli, N: Chevron or Wilson metatarsal osteotomy for hallux valgus. J. Bone Joint Surg. 75-B: 825 – 829,1993.
10. Pochatko, DJ; Schlehr, FJ; Murphey, MD; Hamilton, JJ: Distal chevron osteotomy with lateral release for treatment of hallux valgus deformity. Foot Ankle Int. 15(9):457 – 61, 1994.
11. Rossi, WR; Ferreira, JC: Chevron osteotomy for hallux valgus. Foot Ankle. 13(7):378 – 381, 1992.
12. Resch, S; Stenstr¨om, A; Reynisson, K; Jonsson, K: Chevron osteotomy for hallux valgus not improved by additional adductor tenotomy. A prospective, randomized study of 84 patients. Acta Orthop Scand. 65(5):541 – 4, 1994. http://dx.doi.org/10.3109/17453679409000 910
13. Smith, RW; Reynolds, JC; Steward, MJ: Hallux valgus assessment: Report of research comittee of the American Orthopaedic Foot and Ankle Society. Foot and Ankle, 5.92 – 103, 1984.
14. Us, K; Yilmaz, C; Ozdemir, M; O˘g ¨un, T: Stabilization of the Chevron procedure for hallux valgus deformity with a capsuloperiostal flap. J Foot Ankle Surg. 38(1):2 – 7, 1999. http://dx.doi.org/10.1016/S1067-2516(99)80081-7
15. Winemaker, MJ; Amendola, A: Comparison of bioabsorbable pins and Kirschner wires in the fixation of chevron osteotomies for hallux valgus. Foot Ankle Int. 17(10):623 – 8, 1996.