https://doi.org/10.1007/s41999-018-0129-0 RESEARCH PAPER
Knowledge and practice of nursing home caregivers about urinary
incontinence
Semiha Yenişehir1 · İlkim Çıtak Karakaya1 · Mehmet Gürhan Karakaya1
Received: 17 August 2018 / Accepted: 7 November 2018 / Published online: 13 November 2018 © European Geriatric Medicine Society 2018
Abstract
Purpose The aim of this study was to investigate nursing home caregivers’ knowledge and practice of urinary incontinence
in Muğla-Turkey.
Methods Knowledge and practice of urinary incontinence of 34 nursing home caregivers were assessed by a form
origi-nated from knowledge and practice instrument and urinary incontinence knowledge scale. Incontinence quiz was also used to assess knowledge about UI.
Results According to the analysis of the items from the knowledge and practice instrument, 20.6% of caregivers never
control the amount of urinary incontinence in residents with dementia, document the amount of urinary incontinence and set up a toilet plan for residents with no or slight mental incapacity. According to the analysis of the items from the urinary incontinence knowledge scale, majority of caregivers considered urinary incontinence as a normal result of aging. The mean incontinence quiz score of all participants was 5.5 ± 2.0, indicating poor knowledge about UI.
Conclusion Findings indicate the need of developing strategies for improving knowledge and effective practice of urinary
incontinence of nursing home caregivers.
Keywords Caregiver · Geriatrics · Knowledge · Practice · Urinary incontinence
Introduction
Urinary incontinence (UI) is an important and common problem in adults, especially in older women [1, 2]. The prevalence of UI in nursing home residents is reported as 45–70% in the literature [2], and as 30–47.6% in residents of Turkish nursing homes [3–6]. It is a multifactorial condition which leads to many health problems and impairs quality of life. UI might represent an early marker of frailty, since it is associated with a twofold increased risk of impairment in both basic and instrumental activities of daily living [7]. On the other hand, UI can be cured or ameliorated at a large scale when appropriate methods such as lifestyle regulation and behavioral therapy are used [8–10]. However, lack of knowledge about UI and considering it as a result of normal
aging prevent older persons, their families and caregivers from seeking medical help [8, 9, 11–14].
The caregivers have a primary role in the treatment of UI. Since assessment and treatment of UI in nursing home residents are more complex than in younger people due to high prevalence of comorbid conditions in the geriatric pop-ulation such as systemic diseases and cognitive problems, loss of control of bodily functions and loss of independence, caregivers should evaluate incontinent nursing home resi-dents carefully, to find out the most appropriate management methods [10].
The most important barrier to effective intervention plan-ning is the lack of knowledge of caregivers about assessment and treatment of UI. In a study of Resnick et al., lack of knowledge about UI and negative attitude about effective-ness of incontinence treatment among nursing staff, together with adhering to toileting schedules or ignoring requests for toileting, were mentioned as reasons for inadequate conti-nence care [10, 15]. Therefore, knowledge and practice of UI of nursing staff should be assessed, and subject-related training should be provided [13, 14].
* İlkim Çıtak Karakaya
ilkim74@yahoo.com; ikarakaya@mu.edu.tr
1 Department of Physiotherapy and Rehabilitation, Faculty
of Health Sciences, Muğla Sıtkı Koçman University, 48000 Muğla, Turkey
The presence of individuals with UI in nursing homes leads to an increase in health care costs, number of caregiv-ers and workload, and even morbidity and exhaustion in car-egivers [8, 16]. In a study of Kubik et al., it was reported that improving the level of knowledge about UI could increase health care seeking, diagnosis and treatment opportunities [12]. For this reason, the level of knowledge about UI has been studied in different populations [3, 11, 13, 14, 17–19]. The number of studies in the literature which investigated nursing home caregivers’ knowledge and practice of UI is low [10, 14, 18], and to our knowledge, there is no study focusing on the knowledge and practice of UI in nursing home caregivers in Turkey. Therefore, this study aimed to evaluate the caregivers’ level of knowledge and practices of UI in nursing homes.
Methods
This questionnaire-based cross-sectional study was con-ducted on the caregivers of three nursing homes in Muğla-Turkey, between November 2016 and February 2017, in accordance with the Helsinki Declaration of Ethics Principles.
Administrative and ethical approval for the study were obtained from Muğla Family and Social Policies Provincial Directorate and Scientific Research Ethical Board of Muğla Sıtkı Koçman University, respectively.
Age (year), gender (female/male), educational level (liter-ate/primary/middle/high school/university), marital status (married/single/widow(er)/divorced), profession (nurse/ physiotherapist/care staff, etc.) and professional experience (year) of the participants, as well as duration of working at nursing homes (year) and experiences of caregiving to incontinent individuals and continuous training on urinary incontinence (yes/no) were recorded.
Knowledge of UI was also assessed by Turkish Incon-tinence Quiz (IQ) which was developed by Branch et al. [19, 20]. The measure was translated into Turkish by Kara et al. (2017), and the Turkish version was shown to be reli-able and valid in gynecology patients [19]. IQ consists of 14 items and the participants were asked to answer each item as “Agree/Disagree/Don’t know”. “Agree” for the 1st, 4th, 6th, 8th, 10th and 11th items, and “Disagree” for the 2nd, 3rd, 5th, 7th, 9th, 12th, 13th and 14th items were the correct answers. Items marked as “Don’t know” were taken as incorrect. Each correct answer is 1 point, and the total score ranges between 0 and 14, where higher scores indicate higher level of knowledge about UI [19].
The validity of the Turkish IQ has not been established in caregiver population yet and the measure does not include practice items. In addition, there is not any reliable, valid and standardized Turkish scale which measures both knowledge
and practice of caregivers about UI. To assess the knowledge more comprehensively by the items which are not covered in the IQ, and also to assess caregivers’ practice about UI, an additional form originated from urinary incontinence knowledge scale (UIKS) and knowledge and practice instru-ment (KPI) was used in this study [13, 14]. The UIKS and KPI were translated into Turkish by two researchers inde-pendently, and then synthesized by all researchers to obtain common forms for each scale. UIKS measures knowledge about risk factors, symptoms, impacts, prevention, treatment and management of UI. It consists of 30 items and the par-ticipants were asked to answer each item as “Correct/False/ Don’t know”. Scores ≤ 18 indicates poor knowledge, 18–24 moderate knowledge and ≥ 24 good knowledge [13]. The value of content validity index was 0.75; internal consist-ency reliability was 0.72 for the community nurses and 0.69 for the older people as reported in a study on knowledge of urinary incontinence among Chinese community nurses and community-dwelling older people [13]. The KPI-knowledge scale consists of 18 items regarding facts and statements about UI. Response categories are “Yes/No/Don’t know”. KPI-practice scale consists of 28 items regarding caregiv-ers’ actions towards urinary incontinent residents. Responses are measured on a four-point Likert scale (always, often, sometimes, never) [14].
In this study, the correct and false answers to each items were analyzed, the items with most correct and false answers as well as the most lacking practices were reported in terms of number and percentage values.
Statistical analysis
IBM SPSS Statistics for MacOSX, version 22.0 (IBM Corp., 2013, Armonk, NY, USA) was used for statistical analysis. Quantitative variables were described as mean (X) ± stand-ard deviation (SD), and qualitative variables as number (n) and percentage (%).
Results
Among a total of 68 nursing home caregivers, 34 individu-als (30 care staff, 3 nurses, 1 physiotherapist) signed the informed consent form and were included to the study. Twenty-two caregivers (64.7%) were female and 12 (35.3%) were male. Their mean age was 36.5 ± 6.9 years. Most of them (41.2%) were high school graduates, 29.4% were mid-dle school graduates and 17.6% were primary school gradu-ates. Caregivers with a university degree had a low rate of 11.7%.
The professional experience of caregivers was 8.7 ± 5.7 years and they were working at nursing homes for 8.1 ± 5.2 years. All of them have reported that they had
experience in taking care of incontinent patients and also had continuous training about UI.
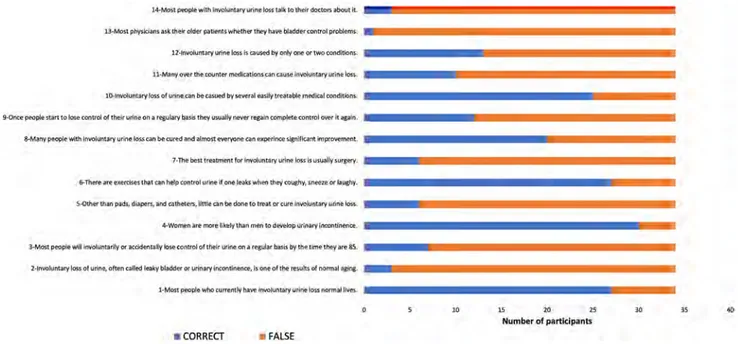
The mean IQ score of all participants was 5.5 ± 2.0, indi-cating a low level of knowledge about UI. IQ items with the highest rate of incorrect answers were the 2nd, 13th and 14th items. The numbers of correct and incorrect answers for each item are presented in Fig. 1. High rate of incorrect answers to the 2nd (involuntary loss of urine, often called leaky bladder or urinary incontinence, is one of the results of normal aging) and 3rd (most people will involuntarily or accidentally lose control of their urine on a regular basis by the time they are 85) items indicates that caregivers consider UI as a natural result of aging. High rate of incorrect answers to the 13th (most physicians ask their older patients whether they have bladder control problems) and 14th (most people with involuntary urine loss talk to their doctors about it) items point out the wrong opinion of caregivers about doc-tor–patient communication on UI.
The IQ item with the highest correct answer rate (n = 30, 88.2%) was the 4th item, indicating that women were more likely than men to develop UI. Furthermore, most of the participants knew that there were exercises that can help control urine if one leaks when he/she coughs, sneezes or laughs (item 6) (n = 27, 79.4%) and involuntary loss of urine could be caused by several easily treatable medical condi-tions (item 10) (n = 25, 73.5%).
In parallel with the 2nd item of IQ, analysis of the 4th item of UIKS also showed that most of the participants (n = 28, 82.4%) considered UI as a normal part of aging. The answers given to the 30th and 12th items of UIKS pre-sented that all of the participants were in agreement that
pads and diapers could be used to manage UI, and UI would restrict the social activities. Almost all of the participants (n = 33, 97.1%) answered the 2nd (recurrent urinary tract infection can cause UI), 8th (UI can occur with frequent urgent sense, a sudden, strong desire to void and inability to hold urine), 11th (UI can restrict the activities of daily living and sexual activities) and 13th (UI can lead to psychological distress, such as anxiety, depression, and low self-esteem) items correctly. UIKS items which were answered as “Don’t know” were the 16th (avoiding constipation can promote urinary continence) and 25th (surgical treatment can solve the problem of UI completely) items. Items related with the effectiveness of pelvic floor exercises in reducing the risk of (20th item) and helping treatment for UI (21st item) were answered correctly by more than half of the participants.
According to the analysis of questions based on KPI-knowledge scale, only 5.9% participants knew that stress incontinence was not caused by psychological problems, and nearly half of the participants (44.1%) did not know that toilet training could improve incontinence in older people requiring care. All of them knew that a bladder infection could cause urinary incontinence. Besides this (4th item), 2nd and 6th items which were related to the normal fre-quency of emptying the bladder and the situations that UI can occur more often were the items with the highest correct rate (n = 33, 97.1%).
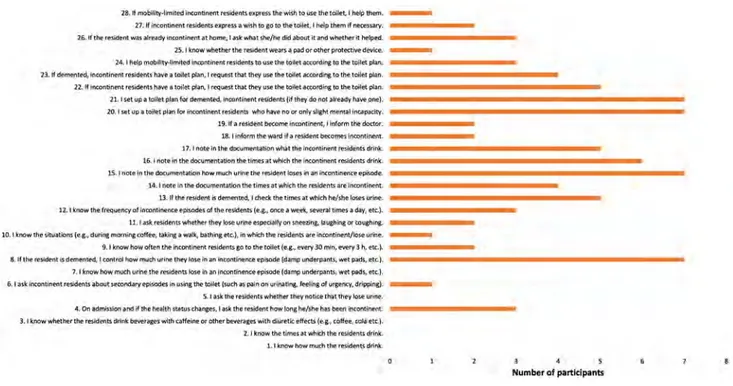
According to the questions based on the KPI-practice scale, 20.6% of caregivers never control the amount of urine which residents with dementia lose in an incontinence epi-sode (damp underpants, wet pads, etc.) (8th item), set up a toilet plan for incontinent residents who have no or only
Fig. 1 Number of participants with correct and false answers to the IQ items
l4•tdo~I pl(10pl,t wilh lnYOIWnUry Wine ~11.atk to I heft dotlrm, 1botlt ii..
10--trwduntlHV Joss of Ul11'• can be cawed bv se~al easily treatable ml!dlmt aiadltbns..
3--M-a""' peDPII!! 'wtth lnwolunla(11 u,lnl!! los.s c.an be cur@d and almost eyeryo~ can !!llperince ilgnlffcant lmprDWfflffll. 7-The bmt lreiltmiml for lnvokmtarv urfnR loss is usually surierv,
CORRECT • FAL5E
10 15 20 2S
slight mental incapacity (20th and 21st items), and docu-ment how much urine the resident loses in an incontinence episode (15th item) (Fig. 2).
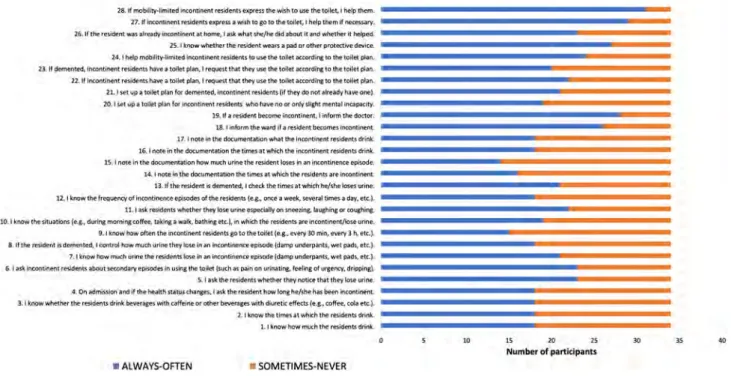
Most of the caregivers reported that they often or always help incontinent residents with (91.2%) or without mobility limitations (85.3%) when they express a wish to go to the toilet (27th and 28th items), and inform the doctor (82.3%) and the ward (76.5%) if a resident becomes incontinent (18th and 19th items). The percentage of caregivers who often or always know whether the resident wears a pad or other protective device was 79.4% (Fig. 3).
The KPI-practice scale items with the lowest “often or always” ratios were the 8th (if the resident is demented, I control how much urine they lose in an incontinence epi-sode) and 9th (I know how often the incontinent residents go to the toilet) items, despite the fact that they should always be practiced (Fig. 3).
Discussion
The findings of this study point out lack of knowledge and practice of UI of nursing home caregivers. Mean score of the caregivers from IQ was 5.5 over 14. This score was similar to the mean IQ score of different ethnic groups (5.8) [12], and slightly higher than the mean score of Korean–American women (4.9) [11]. When it was considered that all of the car-egivers received continuous training about UI before, it can
be affirmed that their mean IQ score is quite low, indicating poor knowledge about UI.
Analysis of the related items from UIKS and KPI-knowl-edge scales also pointed out caregivers’ lack of knowlKPI-knowl-edge about aging and UI relationship. Subject-related literature also supports this finding, indicating that both caregivers and older people consider UI as a normal part of aging due to lack of their knowledge [10, 13, 21]. Considering this issue as a normal condition may prevent caregivers from making accurate assessments and providing an effective management.
Analysis of the responses given to the items about treat-ment of UI showed that many caregivers were unaware of the exercises for UI treatment. Their opinion was that, other than pads, diapers, and catheters, little could be done to treat UI, and the best treatment for UI was usually surgery. The cor-rect response rate of other items related to the treatment and management of UI was also not too high. This indicates that a better education about management of UI including appro-priate exercises and behavioral approaches such as scheduled toileting; avoiding from smoking, alcohol, coffee, obesity and constipation; not restricting fluid intake in daytime, etc., should be provided to the nursing home caregivers.
Analysis of the UI practices of caregivers pointed out that the most common practice was helping incontinent residents with or without mobility limitations, when they expressed a wish to go to the toilet. The most obvious lack of practice was about documenting the amount of urine the resident loses in an incontinence episode. In a previous study about
Fig. 2 Number of participants who responded as “never” to the KPI-practice scale items
281 II mobllity•llmi1~ flltontinlPflt lt'Sictt!11b RJI.PIRSS tht: wish to iG4t the-!ollt-t. I ~ them.
-27. lf inc.ontlnent reiidmts eJprHS • wish to eo to the toilet, I help thl!m if N!Ct'SArV, 26.. tfthe resident w.u. alt'I'•dv lnc.onllnentat homl!:, I asl'. 'Mlriilt she/hi! did abOlll it and wMt~ it h@lped. lS.111:nowwt,,thertht-restdentwtanap,dorotherprot«t.M!'dtvke. -24. I "-elP moblllt'(-llmlted lnmnt.inent resldenU to US!! thl! to•,1accofdln110 the tc!1l'l pl&,L 73. t1 deMt!!'dt4 lncon1lnen1 resi6MU h.Wt I tOiltl plan, I tE'(l\jflSt thlt thtY Ust the tOflf!t -'"Otdin& to !he 1olle.1 pl,an . . n, tt mcGntir,ent re1idtn\S h-&ve I t9ile:t pl~n, I r~uest th.at t ~ uu •~ toilet •c,cof'O!ng to U,t tokd ..,&In. U. I ~t up a toiltt pl•n tot Demcnttd1 inC'Ol'!IIMnt rHidf!:nb (If lhrt do not alr'udy hlvt one}.
20, I ~t up• to1it:t plan b il"ICOf'ltlnmt rH«fl!nU '#ho have no Of only "-l&M mefflil !na~city.
19. If, te.skltAt b«omt 1ncont1n,nt, f !nl0tm the docior. 18. I ;nform the-ward if a r6idtrit Otoeo~ lncontlrieftt.
J 7, t ncte Jn lh1: documentation what lhe lnwntJmmt re:sldurts drink.
16. I oott. in lhl! dcxume.ntatlon the 1untta1 which 1h@ lncontml!nt residents drink. ]5, J n01.e ln th!! docUm!!'llatlon hOw much urine: th!! ,es;ident lml!l in .an fnc.on.tlnffltl' episode.
14, I note In the documem.aOOfl 1he times at ~ h 1he mldents are lncofl(!f\N\t.
U. If the ft-$ldent is df!fl"lented. I ched the tit\'leS at which l'le/s.ht loses uMe:.
11.1 know lh<t frtq~ o, ittlXlnllntnc.t e-pnodti cf lhe re"1tnb. (11.,a.., once a ~ stve:Nlt times a d.111 , ~ ) .
11. I do. rtSld«n.s Wh9'he-f they lose urine-11pe:c:iat!y on ~Dfla. liU&,hlng or c;ouchu,._. JQ, 1 know the srtu11tforu, (te.11,,i durfnc m0tNn1 cofftt, ~k.Jna: • Wo111t., bathing etc.), fn which tht re:side\ts are: inmrrti1W.11t/lose um~
-9, I know how olten W 1ncon1,ne:n1 residents g:o to the toilet fe,1 .. ,:very 30 min1 t!W.,Y 3 h, l!tc.~ .Iii, If I he ~ e n t 15 dl!fflenlNI,, I control t,ow mud\ urll'lt' lhl!'f lose l'"n an Nonlinenu episode (damp undl!!fp.anu. wet p.uis~etc.1. ?, I k'ftf!Whowmvdl u,trie t~ ,~enu.
~e:
"
;a,n lnconrinenc:e~lsode fdarnp urtd,!.rp,1:nu., \N'e1 padi~etc.). 6. I 3sk:4nconllnet1t residenu •boui~nd.1rv epb.odes ln 1uins the- tolle1 ~ch u palnc-,, u1i~~1rc. fPel g of IJlfli!nc¥, dr,Clllif!&)..5.1 t:sk rhe ,~entt'Nhtthtt theyn0tlet 1~1 thf>f lost. Utmt, 4. 011 I d ~ •Md if me he~lth St.ltuJ chal'lttts, I.~ t.l'!e rHidttlt tiow IOfll!I MAM hn bee,\ i't-COl"l(iMn 3, I know ·wheO~.r UJt!" m;ktl!J\b. llrinla: bl!'l'e.ra8('s wilh atfl!iJl'I! or otliu b2'ierala ~th dl~Uc effects {~1,, tciffn., u;iia l!tC.l,
2, I 111:now the tiffll!s at which the ,esidents: drink. .LI lmow how muc:h the resid!!nts drink.
' 5
UI practices of nurses and nurse assistants, the rate of docu-mentation was low in both groups [14]. Lack of practice about documentation of the urine loss may lead to follow-up deficits. If a caregiver overlooks the condition when a resi-dent starts to lose increased amount of urine, this may cause a delay in appropriate treatment by preventing to find out the reason. Therefore, importance of documentation should be included and emphasized in continuous education programs.
Furthermore, although it is necessary to set up a sched-uled toileting plan for residents with no or slight mental incapacity/dementia, low percentage of caregivers who always/often create a toilet plan shows that practice of car-egivers for UI is insufficient.
In this study, 82.3% of the participants reported that they always or often inform the doctor if a resident becomes incontinent and 85.3% help incontinent residents if they express a wish to go to the toilet. These percentages are lower than the percentages (93.9% and 95.8%, respectively) found in a study which was conducted on Korean health-care providers working at long-term health-care hospitals, to assess their knowledge and practice behaviors of UI [18]. While the sample of that study consisted of physicians, nurses and physiotherapists, the sample of the current study was composed of certified caregivers, except three nurses and one physiotherapist. The difference of the findings may be due to different educational formation characteristics of the samples including the time spent for this formation, together with the small sample size in the current study, which might induce large variation of rate for each good or poor response.
The findings of this study should be interpreted by tak-ing some limitations into account. For example, the only reliable and valid Turkish scale used in this study is the IQ, which measures patients’ level of knowledge about UI. The validity of this scale for caregivers has not been established yet. Since there is not any reliable, valid and standardized Turkish scale, other questions related to knowledge and prac-tice of UI of caregivers were assessed by a form originated from knowledge and practice instrument and urinary incon-tinence knowledge scale. Another limitation is that this study was conducted on a small group in Muğla nursing homes; therefore, we do not know if the findings apply to nursing home caregivers in different geographical regions. Most of the participants were certified caregivers and the number of health professionals such as physicians, physiotherapists and nurses was low. Therefore, no statistical comparison could be made between different professional groups.
The findings of this study are important since it informs about the current knowledge level and practice of UI of nursing home healthcare providers in Turkey. Although all of the participants reported that they had relevant con-tinuous training, the findings indicate lack of knowledge and practice deficits about UI. According to the Life-long Learning General Directorate of Turkish Ministry of National Education, prerequisites for being a certified caregiver (in another name, self-care support providers) of patients or elderly people are having at least a primary school degree, being > 18 years old and having basic phys-ical, psychological and motor competencies required for
Fig. 3 Number of participants who “always/often” or “sometimes/never” practiced KPI-practice scale items
28.. 1r mob.llty•lllffllted lncon~n,ent r~ld~s: e>:pre-ss Ute-"'41.h le> U$e the toilet., I help dl,MI_ 17. If tnCanlTIINU re-sldt!-nt~ ~pr~~ .JI Wlll'li 101!!010 the toilet, I help 11\e-n-ilr ~$J.al"Y.
16.lrl.hl!' re~idc!nt was i.lf'l!ad¥ looonliner.t al homl!1 I ;ask what ~he/he did ;;ibout it and whe1i.r i'I heJpe:d.. - - - --
-25. I knew ~ ~ ltw: ~ D@l"ll wears a p;ad Dr oth!'r protective d~ir::e.
~4.1~mol:lil1t~lmiu:d!nco,i.1lnem,~i:1tnutou"-1the~llt:1~il'l&tarNtoMe1oto,n, - - - -- -l3, ll dernt:r1tfd1 lncontiMM residonu h~• ai t0,1t:t pbn, I tt:Qvut 1ha11hcv use lht: tollct accordirw to me toilet plin. - - -
-22. If lrKontlne"t resrdents h,1'1,1!' a toll et pl111,, I req~ tl\at (he<,' u~ the tolll!t ila:on:llng to the toUl!'t pl;;in 2L I seet up a toilet plan for d!!IT'll!'f'lt:!!d, lnCOJl.tlner,t ,ulde:nlihf they do not already haittone).
20, l..ef upa tarlt1 pl.tin fClf l«onlintnl res.tfcrm whoha\/eno01 ontysiqihl mc:nr.ilfMapac1ty. l.9, ,, • residr:M b«oma rnc:onllnent.-1 inlom, IM dOclor.
lS. 1 lnformthew.atd !fa ~sldentbecomH1noontlnen~ - - - --
-17.1 note rntht doc.umentat.ori~I the lnmndne.ntre-sldenudrfnlc.. - - - -- -16.11101.e in lhe docu'1ll!ntation thlil! tlmH at Whkh tht: iqcootinfflt residl!nts. ~ k.
15, I note ln the docufflll!r}tiltion how much U'1n1! the ~ t loses. In iln ~1inencl! episode.
1". I n-o,:e:l,i.thedoet1mNtaUOnthetlmesat \Ntlkhthensldentiateinmntlnent. - - -
-13. tl the ~ m i:li·ctetnen1ect, I check the liMt',$ 111 wi'!ichht/t.he ~ 1.lflne.
12, 1 knrciw lh~ fnqutncy of il")COn~ni:@ tDisodcs of thl! rHi;lm~ [t!l.J., Ofl(;ill a '#'ttk, several u ~ ~ day, ttc,).
11.1.a~k. resldet1ts•1Mu!thf!rtheyloieurirleiHPl!dallvonsneezin~ lil1JihnJOl"COUJh~ - - - --
-10. I ~now the1ltt111tlons je,11., dwlng morning coffee,. ui\i:lng 11,,,1alk, ba1h"1.1etc.l, tn wt!ICh lhl rtsldents 1retncontlnentfios,li!'u1lne. - - - -- -9. I !(now' how 0,ten the mcontlMnt ftilderll'!I g61olbt l~lt (e.11,, e</11!',y 30 fl'l+n., ~ l h, tlc.),
8, If thl! ~ t n: dl!fflenkd,, I tlOfltl DI I\Dw much urfne the¥ lo~ In •n lnccnllMAC't' e:p&.ode (damp underp.ants, wtl pads, e:tt.J.
1. I k.now hcwA'AICh u,1ne the res.idl!'nt!ID\e In •n ITTGanlinw,,aieplsodejcbmpundBpanu, wli!'tpad~, etc.). - - - --
-'-I ~sic lnc.o(l1,,1n«f"I• rinddtnu abot.11 ,ecol'ldJN episode, In usln1 ~ ,01 ... [111th H pain on IJrlnatir-L fetlin& of urtencv, dripQir,g). - - - --
-S.. l ask t.ht residf111.1swhtthtr thtVnotie.t 1h111he-y lost utiN. - - - --
-4. On admission ;and if the he.al th stalu sma,.e5, I a~ 1M resldenl hew long he/she h-as been lnc.anbnent.
:3, I li:nowwhether the-resldentsdflM beYet;tgl.:!5 with caff~ne or olhl!f beverat11!5-withdluretlc effecl!i je.g.. coffee. c:da etc.). - - - --
-"2. I kno'w chic UMt\l\ 'wh~h 1tie: midt.n~ drm1':. - - - --
-1.1t110WhoW'JT11Jch1h!'raidt11t£dl"l('lij_ - - - --
-10 15 ,o
,.
30Number of participants
the course program. The eligible individuals should com-plete a 305-h course program, in which they are trained in regard to giving care to the elderly people or patients with incontinence (for only 12 h). The learning outcomes of this module of the curriculum are providing urinal/bedpan to the individual in need of care by taking care of privacy, and giving care to the individuals who have urinary/fecal incontinence. The applicants who successfully complete this course program and pass the related exams receive a course completion certificate, transcript and Europass Certificate Attachment [22]. The short duration of the cur-riculum for UI and the fact that people have so many dif-ferent backgrounds before getting certified caregivers may be the explanations of poor knowledge and practice of UI. The answers may need a deeper analysis but the too small number of participants from different professions prevents this. Also, the source and content of continuous training for the participants were not questioned in the study. This lack of the study prevents making any comments related to the current curriculum about UI for the continuous train-ing programs.
It seems that current state of basic and continuous training for the caregivers needs to be reinforced for an effective management of UI in nursing homes. Therefore, future studies should focus on improving theoretical and practical content of these training programs. In addition, it is advisable to develop reliable and valid measures in Turkish language, to assess if these specific programs are efficient in improving UI awareness, knowledge and prac-tice of nursing home staff from different professions.
Acknowledgements The authors thank Ömer Günay (physical
trainer—Abide Hasan Nuri Öncüer Nursing Home) and İsmail Uysal (physiotherapist—Fethiye Nursing Home) for their valuable help in collecting data for the study.
Author contribution All authors were responsible for critical revisions
of the manuscript and for important intellectual content. All authors approved the final contents of the manuscript.
Funding This study was funded by Muğla Sıtkı Koçman University
Research Projects Coordination Office (Project Grant number 17/092 and the title “Knowledge and Practice of Nursing Home Caregivers about Urinary Incontinence”).
Compliance with ethical standards
Conflict of interest The authors have no conflict of interest to declare.
Ethical approval This study was performed in accordance with the
ethi-cal standards as laid down in the 1964 Helsinki Declaration of Ethics Principles and its later amendments or comparable ethical standards. Administrative and ethical approvals for the study were obtained from Muğla Family and Social Policies Provincial Directorate and Scientific Research Ethical Board of Muğla Sıtkı Koçman University, respec-tively.
Informed consent Informed consent was obtained from all individual
participants included in the study.
References
1. Abrams P, Cardozo L, Fall M et al (2003) The standardisation of terminology in lower urinary tract function. Report from the standardization of the subcommittee of the International Conti-nence Society. Urology 61:37–49
2. Ueda T, Tamaki M, Kageyama S, Yoshimura N, Yoshıda O (2000) Urinary incontinence among community-dwelling people aged 40 years or older in Japan: prevalence, risk factors, knowledge and self-perception. Int J Urol 7(3):95–103
3. Arıkan E, Özcan E, Bardak A, Ketenci A (2002) Urinary incon-tinence in women living in a rest home. Turk J Geriatr 5(1):7–10 4. Olgun N, Eti Aslan F, Yücel N, Kan Öntürk Z, Laçin Z (2013)
Assessment of health status of the elderly. ACU Sağlık Bil Derg 4(2):72–78
5. Cankurtaran F, Soyuer F, Akın S (2015) Urinary incontinence problem in elderly people living in rest home and its relationship with mobility. Gümüşhane Univ J Health Sci 4(4):594–603 6. Çuhadar D, Sertbaş G, Tutkun H (2006) Relationship between
level of cognitive functions and activities of daily life at elderly people who live in rest home. Anadolu Psikiyatri Derg 7(4):232–239
7. Veronese N, Soysal P, Stubbs B, Marengoni A, Demurtas J, Maggi S et al (2018) Association between urinary incontinence and frailty: a systematic review and meta-analysis. Eur Geriatr Med 9:1–8
8. Jerez-Roig J, Santos MM, Souza DLB, Amaral FLJS, Lima KC (2016) Prevalence of urinary incontinence and associated factors in nursing home residents. Neurourol Urodyn 35(1):102–107 9. Rijal C, Hakim S (2014) Urinary incontinence in women
liv-ing in nursliv-ing homes: prevalence and risk factors. INAJOG 2(4):193–198
10. Skotnes LH, Hellzen O, Kuhry E (2013) Perceptions and barriers that influence the ability to provide appropriate incontinence care in nursing home residents: statements from nursing staff. Open J Nurs 3:437–444
11. Kang Y (2009) Knowledge and attitudes about urinary inconti-nence among community-dwelling Korean American women. J Wound Ostomy Cont Nurs 36(2):194–199
12. Kubik K, Blackwell L, Heit M (2004) Does socioeconomic status explain racial differences in urinary incontinence knowledge? Am J Obstet Gynecol 191(1):188–193
13. Yuan H, Williams BA (2010) Knowledge of urinary incontinence among Chinese community nurses and community-dwelling older people. Health Soc Care Community 18(1):82–90
14. Saxer S, de Bie RA, Dassen T, Halfens RJ (2008) Nurses’ knowl-edge and practice about urinary incontinence in nursing home care. Nurse Educ Today 28:926–934
15. Resnick B, Keilman LJ, Calabrese B, Parmelee P, Lawhorne L, Pailet J et al (2006) Nursing staff beliefs and expectations about continence care in nursing homes. J Wound Ostomy Cont Nurs 6:610–618
16. Offermans MP, Du Moulin MF, Hamers JP, Dassen T, Halfens RJ (2009) Prevalence of urinary ıncontinence and associated risk factors in nursing home residents: a systematic review. Neurourol Urodyn 28(4):288–294
17. De Gagne J, So A, Wu B, Palmer MH, McConnell ES (2015) The effect of a urinary incontinence self management program for older women in South Korea: a pilot study. IJNSS 2(1):39–46
18. Jang Y, Kwon BE, Kim HS, Lee YJ, Lee S, Kim SJ et al (2015) Knowledge and practice behaviors regarding urinary incontinence among Korean healthcare providers in long-term care hospitals. Int Neurourol J 19:259–264
19. Kara KC, Çıtak Karakaya İ, Tunalı N, Karakaya MG (2018) Reli-ability and validity of the Turkish version of incontinence quiz. J Obstet Gynaecol Res 44(1):144–150
20. Branch LG, Walker LA, Wetle TT, DuBeasu CE, Resnick NM (1994) Urinary incontinence knowledge among community dwelling people 65 years of age and older. J Am Geriatr Soc 42:1257–1262
21. Ehlman K, Wilson A, Dugger R, Eggleston B, Coudret N, Mathis S (2012) Nursing home staff members’ attitudes and knowledge
about urinary incontinence: the impact of technology and training. Urol Nurs 32(4):205–213
22. Turkish Ministry of National Education, Lifelong Learning General Directorate [T.C. Milli Eğitim Bakanlığı, Hayat Boyu Öğrenme Genel Müdürlüğü]. Self-Care Support Staff Training Course Program for Patient and Elderly Services Area [Hasta ve Yaşlı Hizmetleri Alanı Öz Bakıma Destek Elemanı Eğitimi Kurs
Programı]. Ankara: 2018. http://hbogm .meb.gov.tr/modul erpro
graml ar/?q=29&alan=Hasta %20ve%20Ya%C5%9Fl%C4%B1%20 Hiz metle ri. Accessed 20 Sept 2018