Allergy. 2019;74:1611–1630. wileyonlinelibrary.com/journal/all © 2019 EAACI and John Wiley and Sons A/S.
|
1611 Published by John Wiley and Sons Ltd. Received: 27 January 2019|
Revised: 15 February 2019|
Accepted: 20 February 2019DOI: 10.1111/all.13786
E A A C I P O S I T I O N P A P E R
Management of ocular allergy
Andrea Leonardi
1| Diana Silva
2| Daniel Perez Formigo
3,4| Banu Bozkurt
5|
Vibha Sharma
6| Pia Allegri
7| Carmen Rondon
8| Virginia Calder
9| Dermot Ryan
10|
Marek L. Kowalski
11| Luis Delgado
2| Serge Doan
12| Jean L. Fauquert
131Ophthalmology Unit, Department of Neuroscience, University of Padua, Padua, Italy 2Basic and Clinical Immunology, Department of Pathology, Faculty of Medicine, Serviço de Imunoalergologia, Centro Hospitalar São João, University of Porto, EPE – Porto, Porto, Portugal 3Department of Ophthalmology, Hospital Universitario de Torrejon, Madrid, Spain 4Faculty of Medicine, University of Francisco de Vitoria (UFV), Pozuelo de Alarcon, Madrid, Spain 5Department of Ophthalmology, Faculty of Medicine, Selcuk University, Konya, Turkey 6Department of Paediatric Allergy and Immunology, Royal Manchester Children's Hospital, Manchester University NHS Foundation Trust, Manchester, UK 7Allergic Conjunctivitis Unit, Ocular Inflammatory Diseases Referral Center, Rapallo Hospital Ophthalmology Department, Genova, Italy 8Allergy Unit, Regional University Hospital of Malaga, IBIMA, UMA, Malaga, Spain 9Department of Ocular Biology & Therapeutics, UCL Institute of Ophthalmology, London, UK 10Allergy and Respiratory Research Group, Medical School, Usher Institute of Population Health Sciences and Informatics, University of Edinburgh, Edinburgh, UK 11Department of Immunology, Rheumatology, and Allergy, Medical University of Lodz, Lodz, Poland 12Service d’Ophtalmologie, Hôpital Bichat and Fondation A. de Rothschild, Paris, France 13CHU Estaing, Unité d’Allergologie de l’Enfant, Clermont‐Ferrand Cedex1, France Correspondence Andrea Leonardi, Ophthalmology Unit, Department of Neuroscience, University of Padua, Padua, Italy. Email: andrea.leonardi@unipd.it Funding information This work was done under the approval of EAACI with a TF budget 2015‐18.
Abstract
The treatment and management of ocular allergy (OA) remain a major concern for different specialties, including allergists, ophthalmologists, primary care physicians, rhinologists, pediatricians, dermatologists, clinical immunologists, and pharmacists. We performed a systematic review of all relevant publications in MEDLINE, Scopus, and Web Science including systematic reviews and meta‐analysis. Publications were considered relevant if they addressed treatments, or management strategies of OA. A further wider systematic literature search was performed if no evidence or good quality evidence was found. There are effective drugs for the treatment of OA; how‐ ever, there is a lack an optimal treatment for the perennial and severe forms. Topical antihistamines, mast cell stabilizers, or double‐action drugs are the first choice of treatment. All of them are effective in reducing signs and symptoms of OA. The safety and optimal dosing regimen of the most effective topical anti‐inflammatory drugs, corticosteroids, are still a major concern. Topical calcineurin inhibitors may be used in steroid‐dependent/resistant cases of severe allergic keratoconjunctivitis. Allergen‐specific immunotherapy may be considered in cases of failure of first‐line treatments or to modify the natural course of OA disease. Based on the current wealth of publications and on the collective experience, recommendations on man‐ agement of OA have been proposed.1 | INTRODUCTION
Ocular allergy (OA) represents a collection of ocular hypersensitivity disorders affecting the eyelid, conjunctiva, and cornea. OA includes seasonal and perennial allergic conjunctivitis (SAC and PAC), vernal and atopic keratoconjunctivitis (VKC and AKC), and contact bleph‐ aroconjunctivitis (CBC).1 These clinical subtypes may be diagnosed and managed by ophthalmologists, allergists, pediatricians, and rhi‐ nologists, with or without experience in managing allergies, consid‐ ering clinical history and signs and symptoms, aided by in vivo and in vitro tests.1‐3 Although several studies suggest a high comorbidity of conjunctivitis and rhinitis, conjunctival symptoms are often per‐ ceived by clinicians as a minor problem and suboptimally treated. A recent survey revealed that daily treatment of OA has little con‐ cordance with current recommendations.4 Topical ocular deconges‐ tants and corticosteroids were used in the majority of cases. This was independent of the specific diagnosis of OA subtype and se‐ verity. Topical antihistamines and mast cell stabilizers, which are the first‐line therapy in most published recommendations, were used less frequently.4 The incorrect management of OA may increase the risk of local and systemic treatment‐related side effects.4 This sys‐ tematic review (SR) intends to provide a comprehensive overview of the currently available treatments for OA and of ocular comor‐ bidities and/or complication, and suggest recommendations for their management using best available evidence in published literature.2 | METHODS
2.1 | General search strategy
The literature search was based on the systematic literature search in MEDLINE, Scopus, and Web Science. First, we performed a SR of all SR and meta‐analyses that addressed OA treatments, according to the search query. For each subtype of OA or treatment, if good quality SR or systematic analysis of randomized controlled trials (RCTs) were found, no further systematic search was performed. If no evidence or poor quality of evidence was found, a further sys‐ tematic search was performed. The included literature was selected with respect to their hierarchy in the “evidence pyramid.”
2.2 | Eligibility criteria
We included SR of observational and interventional studies regard‐ ing treatment of OA (SAC, PAC, VKC, AKC, and CBC). The following treatments were included the following: antihistamines, mast cell stabilizers, dual‐acting agents (topical mast cell stabilizers and an‐ tihistamines), non‐steroidal anti‐inflammatory drugs (prostaglandin and leukotriene inhibitors), steroids, calcineurin inhibitors, allergen‐ specific immunotherapy, and biologics. A SR was defined as a re‐ view of the literature with a predetermined and transparent search strategy, where the search strategy and inclusion and exclusion cri‐ teria were explicitly described and included guidelines or position papers containing information regarding quality of evidence. Our systematic literature search included nonpharmacological interven‐ tions including surgery, psychological, lid hygiene, and lubricants. Specific search strategy, selection of the study, and assessment of the quality of the evidence are reported as Appendix S1 and S1.3 | RESULTS
The flowchart of the selection strategy is shown in Figure 1. K E Y W O R D S management, ocular allergy, allergic conjunctivitis, systematic review, treatment F I G U R E 1 Flowchart of the selection strategy of the systematic reviews potentially relevant for the purpose of the position paper. Of the 432 publications, 28 were selected and included (see Tables 2‐6)3.1 | Overview of the available pharmacological
classes of anti‐allergic drugs
There is a wide range of treatment options for OA, some of which are off‐ label. Currently available topical drugs for OA can be classified into differ‐ ent pharmacological classes based on their mechanism of action (Table 1): antihistamines, mast cell stabilizers, dual‐acting agents (topical mast cell stabilizers and antihistamines), alpha‐adrenergic agonists (vasoconstric‐ tors), non‐steroidal anti‐inflammatory drugs (prostaglandin inhibitors), corticosteroids, and calcineurin inhibitors. Immunomodulatory treat‐ ments for OA include allergen‐specific immunotherapy and biologicals.
3.1.1 | Topical antihistamines, mast cell
stabilizers, and dual‐acting agents
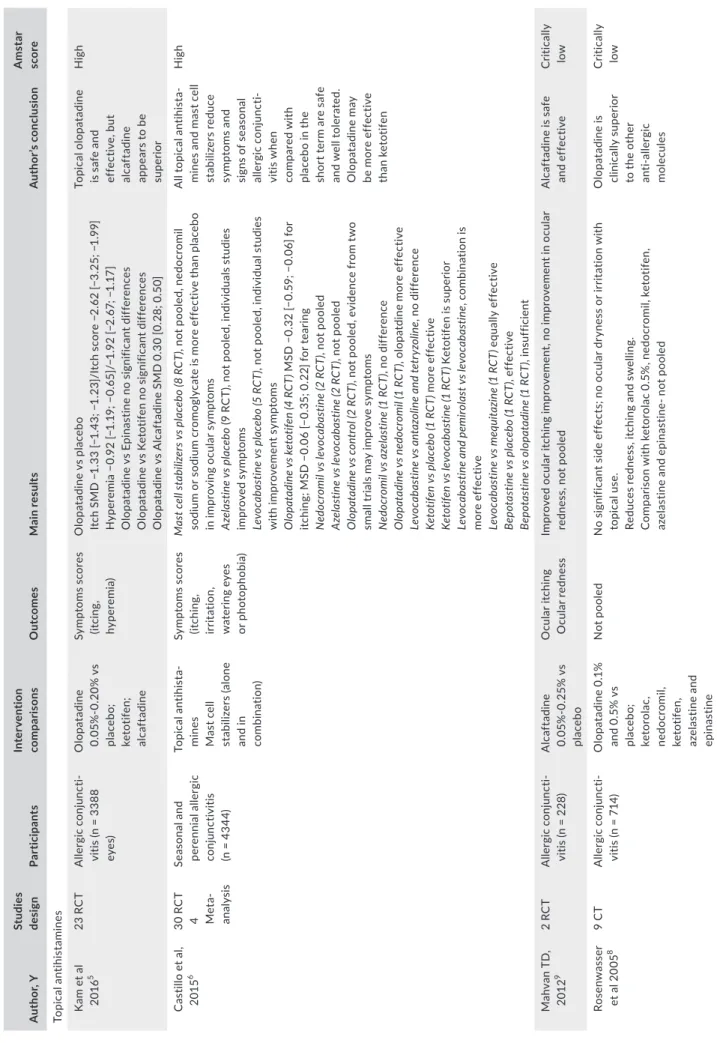
Three SR addressed the use of topical antihistamines, topi‐ cal mast cell stabilizers, or topical dual‐acting agents for the
treatment of SAC and PAC (Table 2): One included 23 RCTs,5 the second 30 RCTs6 in a head‐to‐head study, and the third 41 RCTs.7 All the three reviews concluded that these drugs were effective in reducing ocular symptoms vs placebo.7 Direct comparisons of different antihistamines and mast cell stabilizers showed in‐ sufficient evidence to recommend one drug over another6 even though the peer‐reviewed literature suggested that olopatadine may be clinically superior to the other anti‐allergic molecules,8 and alcaftadine may be superior to olopatadine in reducing ocu‐ lar itch.5 A fourth SR9 comparing olopatadine with other topical antihistamines (epinastine, ketotifen, and alcaftadine) showed a significant benefit from the use of alcaftadine in reducing symp‐ toms scores when compared to the others drugs. Alcaftadine is only currently approved and available in the United States. Since the publication of the last SR, a further clinical trial has been pub‐ lished demonstrating efficacy of epinastine in controlling symp‐ toms of birch pollen allergic patients.10 TA B L E 1 Topical ocular allergy approved medications
Class Drug Dosing Indication Considerations
Antihistamines (second generation) Levocabastine Emedastine 4× daily • Relief of itching • Relief of signs and symptoms • Short duration of action • Frequently not enough to treat alone the entire disease Mast cell stabilizers Cromolyn Nedocromil Lodoxamide NAAGA
4× daily • Relief of signs and symptoms • Long‐term usage • Slow onset of action • Prophylactic dosing • Frequently not enough to treat alone the entire disease Dual‐acting agents (Antihistamine/ mast cell stabilizers) Alcaftadine Azelastine Bepotastine Epinastine Ketotifen Olopatadine 2× daily • Relief of itching • Relief of signs and symptoms • Bitter taste (azelastine) • No reported serious side effects • Frequently not enough to treat alone the entire disease Vasoconstrictor/ vasoconstrictor‐anti‐ histamine combinations Naphazoline/ Pheniramine 2‐4× daily • Rapid onset of action • Episodic itching and redness • Short duration of action • Tachyphylaxis • Mydriasis • Ocular irritation • Hypersensitivity • Systemic hypertension • Potential for inappropriate patient use Corticosteroids (listed in ascending potency order) Hydrocortisone Loteprednol Fluorometholone Desonide Rimexolone Prednisolone Dexamethasone Betamethasone As required • Treatment of allergic inflammation • Use in moderate‐to‐severe forms • Risk of long‐term side effects • No mast cell stabilization • Potential for inappropriate patient use • Requires close monitoring Calcineurin inhibitors Cyclosporine A Tacrolimus 2‐4× daily • Treatment of severe VKC and AKC not responding anti‐allergic drugs • Off label in OA (tacrolimus approved for VKC only in Japan) • CsA 0.1% received marketing authoriza‐ tion by EMA in July 2018 for severe VKC • Magistral/officinals preparations are different from center to center • Quality control and availability of magistral preparations are poor
T A B LE 2 To pi ca l a nt ih is ta m in es , m as t c el l s ta bi liz er s, d ua l‐a ct in g ag en ts A ut ho r, Y St ud ies de sig n Pa rti ci pa nt s Int er ve nt io n co m pa ris ons O ut co me s M ain re su lt s A ut ho r’s c onc lus io n A m st ar sco re To pic al a nt ih is ta min es K am e t a l 20 16 5 23 R C T A ller gi c co nj unc ti‐ vi tis (n = 3 38 8 ey es) O lo pa ta di ne 0. 05 % ‐0 .2 0% v s pl ac eb o; ke to tif en ; al ca ft ad in e Sy m pt om s sc or es (it cin g, hy per em ia ) O lo pa ta di ne v s pl ac eb o Itc h SM D − 1. 33 [− 1. 43 ; − 1. 23 ]/ Itc h sc or e −2 .6 2 [− 3. 25 ; − 1. 99 ] H yp er em ia − 0. 92 [− 1. 19 ; − 0. 65 ]/ −1 .9 2 [− 2. 67 ; − 1. 17 ] O lo pa ta di ne v s Ep in as tin e no s ig ni fic an t d iff er en ce s O lo pa ta di ne v s Ke to tif en n o si gn ifi ca nt d iff er en ce s O lo pa ta di ne v s A lc af ta di ne S M D 0 .3 0 [0 .2 8; 0 .5 0] To pi ca l o lo pa ta di ne is s af e an d ef fe ct iv e, b ut al ca ft ad in e ap pe ar s to b e su pe rio r H ig h C as til lo e t a l, 201 5 6 30 R C T 4 Met a‐ an al ys is Se as on al a nd pe re nn ia l a lle rg ic co nj unc tiv iti s (n = 4 34 4) To pic al a nt ih is ta ‐ min es M as t c el l st ab ili ze rs (a lo ne an d i n co m bina tio n) Sy m pt om s sc or es (it ch in g, irr ita tio n, w at er in g ey es or p ho to ph ob ia ) M as t c el l s ta bi liz er s v s p la ce bo (8 R C T) , n ot p oo le d, n ed oc ro m il so di um o r s od iu m c ro m og ly ca te is m or e ef fe ct iv e th an p la ce bo in im pr ov in g oc ul ar s ym pt om s A ze la st in e v s p la ce bo (9 R C T) , n ot p oo le d, in di vi du al s st ud ie s imp ro ve d sy mp to m s Le vo ca ba st in e v s p la ce bo ( 5 R C T) , n ot p oo le d, in di vi du al s tu di es w ith im pr ov em en t s ym pt om s O lo pa ta di ne v s k et ot ife n ( 4 R C T) M SD − 0. 32 [− 0. 59 ; − 0. 06 ] f or itc hi ng ; M SD − 0. 06 [− 0. 35 ; 0 .2 2] fo r t ea rin g N ed oc ro m il v s l ev oc ab as tin e ( 2 R C T) , n ot p oo le d A ze la st in e v s l ev oc ab as tin e ( 2 R C T) , n ot p oo le d O lo pa ta di ne v s c on tr ol ( 2 R C T) , n ot p oo le d, e vi de nc e fr om tw o sm al l t ria ls m ay im pr ov e sy m pt om s N ed oc ro m il v s a ze la st in e ( 1 R C T) , n o di ff er en ce O lo pa ta di ne v s n ed oc ro m il ( 1 R C T) , o lo pa td in e m or e ef fe ct iv e Le vo ca ba st in e v s a nt az ol in e a nd t et ry zo lin e, n o di ff er en ce Ke to tif en v s p la ce bo ( 1 R C T) m or e ef fe ct iv e Ke to tif en v s l ev oc ab as tin e ( 1 R C T) Ke to tif en is s up er io r Le vo ca ba st in e a nd p em iro la st v s l ev oc ab as tin e, c om bi na tio n is m or e ef fe ct iv e Le vo ca ba st in e v s m eq ui ta zi ne ( 1 R C T) eq ua lly e ff ec tiv e Be po ta st in e v s p la ce bo ( 1 R C T) , e ff ec tiv e Be po ta st in e v s o lo pa ta di ne ( 1 R C T) , i nsu ff icie nt A ll to pi ca l a nt ih is ta ‐ m in es a nd m as t c el l st ab ili ze rs re du ce sy m pt om s an d si gn s of s ea so na l al ler gi c co nj unc ti‐ vi tis wh en co mpa re d w ith pl ac eb o in th e sh or t t er m a re s af e an d w el l t ol er at ed . O lo pa ta di ne m ay be m or e ef fe ct iv e th an k et ot ife n H ig h M ah va n TD , 201 2 9 2 RC T A ller gi c co nj unc ti‐ vi tis (n = 2 28 ) A lc af ta din e 0. 05 % ‐0 .2 5% v s pl ac eb o O cula r i tch in g O cula r r ed ne ss Im pr ov ed o cu la r i tc hi ng im pr ov em en t, no im pr ov em en t i n oc ul ar re dn es s, n ot p oo le d A lc af ta di ne is s af e an d ef fe ct iv e Cr iti ca lly low Ro se nw as se r et a l 2 00 5 8 9 C T A ller gi c co nj unc ti‐ vi tis (n = 7 14 ) O lo pa ta di ne 0 .1 % an d 0. 5% v s pl ac eb o; ket oro la c, ne do cr omi l, ke to tif en , aze la st in e an d epina st in e N ot p oo le d N o si gn ifi ca nt s id e ef fe ct s; n o oc ul ar d ry ne ss o r i rr ita tio n w ith to pic al us e. Re du ce s re dn es s, it ch in g an d sw el lin g. C om pa ris on w ith k et or ol ac 0 .5 % , n ed oc ro m il, k et ot ife n, aze la st in e an d ep in as tin e‐ n ot p oo le d O lo pa ta di ne is cli ni ca lly su pe rio r to th e ot he r an ti‐ al le rg ic m ole cu le s Cr iti ca lly low (Co nt in ue s)
A ut ho r, Y St ud ies de sig n Pa rti ci pa nt s Int er ve nt io n co m pa ris ons O ut co me s M ain re su lt s A ut ho r’s c onc lus io n A m st ar sco re To pi ca l m as t c el l s ta bi lize rs O w en e t a l, 20 04 7 40 R C T Se as on al a lle rg ic co nj unc tiv iti s (n = 7 90 ) To pi ca l m as t c el l st ab ili ze rs ; t op ic al an tih is ta min es an d to pi ca l m as t ce ll st ab ili ze rs w ith an tih is ta min es O cu la r s ym pt om sc or e (it ch in g, bu rn ing , la cr im at io n an d so re ne ss ) So diu m c ro m og ly ca te v s pl ac eb o (8 R C T) O R = 17 [4 ; 78 ] t o be ne fit fr om tr ea tm en t N ed oc ro m il s od iu m v s p la ce bo ( 5 R C T) O R = 1. 8 [1 .3 ; 2 .6 ] Lo do xa mi de tr om et ha mi ne v s pl ac eb o (1 R C T) Top ic al a nt ih is ta mi ne s v s pl ac eb o (9 R C T; 6 le vo ca ba st in e; 1 aze la st in e; 1 e m ed as tin e; 1 a nt az ol in e) n ot p oo le d To pi ca l m as t c el l s ta bi lize rs v s to pi ca l a nt ih is ta m in es (8 R C T) Le vo ca ba st in e vs m as t c el l s ta bi lize rs O R 1. 3 [0 .8 ; 2 .2 ] C on fir m th e be ne fit of to pi ca l m as t c el l st ab ili ze rs a nd an tih is ta min es o ve r pl ac eb o fo r t he tr ea tm en t o f al ler gi c co nj unc ti‐ vi tis . T he re is insu ff icie nt ev idenc e to re co m m en d th e us e of o ne ty pe o f m ed ic at io n ov er an ot he r. M od er ate M an te lli e t a l, 20 07 12 27 R C T 10 met a‐ an al ys is Ve rn al Ker at oc on ju nc iti vi s (n = 1 09 2 pa tie nt s, 21 84 e ye s) M ea n ag e 13 .3 (4 .5 y ) M as t c el l st ab ili ze rs v s pl ac eb o (n = 1 0) M as t c el l st ab ili ze rs v s an ot he r ( n = 8) M as t c el l st ab ili ze rs v s co rt ic os te ro ids (n = 2 ) M as t c el l st ab ili ze rs v s an tih is ta min es (n = 1 ) N SA ID v s pl ac eb o (n = 2 ) N SA ID v s C C T (n = 1 ) A nt im ito tic d ru g (n = 1 ) Itc hi ng , t ea rin g, fo to fo bia , hy per em ia , ta rs al pa pi llae , limba l d ise ase an d c or ne al in vo lv emen t Itc hi ng (m ito m yc in ; s od iu m c ro m og lic at e, c yc lo sp or in e 2% , ke to ro la c) S M D − 1. 43 [− 1. 76 ; − 1. 10 ] Te ar in g (mi to m yc in , s odi um cr om ogl ic at e, c yc lo sp or in e 2% ) S M D −0 .8 4 [− 1. 20 ; − 0. 49 ] Ph ot op ho bi a (m ito m yc in , s od iu m c ro m og lic at e, c yc lo sp or in e 2% ) −0 .2 7 [− 0. 82 ; 0 .3 9] To ta l s ig ns (c yc lo sp or in e an d so di um c ro m og lic at e) S M D − 0. 94 [− 1. 34 ; − 0. 54 ] To ta l s ym pt om s (c yc lo sp or in e 2% a nd s od iu m c ro m og lic at e) SM D − 0. 73 [− 1. 14 ; − 0. 32 ] Ta rs al p ap ill ae (m ito m yc in , s od iu m c ro m og lic at e, c yc lo sp or in e) SM D − 0. 32 [− 0. 64 :− 0.0 0] C or ne al in vo lv em en t ( m ito m yc in , s od iu m c ro m og lic at e, cy cl os po rin e) S M D − 1. 15 [− 1. 50 ; − 0. 80 ] Li m ba l d is ea se (m ito m yc in , s od iu m c ro m og lic at e, c yc lo sp or in e) SM D − 1. 17 [− 1. 50 ; − 0. 83 ] H yp er em ia (m ito m yc in , s od iu m c ro m og lic at e, c yc lo sp or in e, m ip ra go si de 0 .5 ) S M D − 1. 07 [− 1. 38 ; − 0. 76 ] Th e cu rr en tly av ai la bl e to pi ca l dr ug s ar e ef fe ct iv e in tr ea tin g ac ut e ph as es o f V KC . Th er e is a la ck o f ev idenc e to su pp or t t he re co mm en da tio n of o ne s pe ci fic ty pe o f m ed ic at io n fo r t re at in g th is di so rder Low C C T, c or tic os te ro id s; N SA ID , n on ‐s te ro id al a nt i‐i nf la m m at or y dr ug ; R C T, ra nd om ize d cl in ic al tr ia ls ; S M D , s ta nd ar di ze d m ea n di ff er en ce . N ed oc ro m il so di um o r s od iu m c ro m og ly ca te , o lo pa ta di ne , k et ot ife n, a ze la st in e, e m ed as tin e, le vo ca ba st in e (o r l ev oc ab as tin e) , m eq ui ta zi ne , b ep ot as tin e be si la te , c om bi na tio n of a nt az ol in e an d te tr yz ol in e, co m bi na tio n of le vo ca ba st in e an d pe m iro la st p ot as si um . T A B LE 2 (Co nti nue d)
T A B LE 3 N on ‐s te ro id al a nt i‐i nf la m m at or y dr ug s (to pi ca l p ro st ag la nd in a nd o ra l l eu ko tr ie ne in hi bi to rs ) A ut ho r, Y St ud ies d es ig n Pa rti ci pa nt s Int er ve nt io n co m pa ris ons O ut co me s M ain re su lt s A ut ho r’s c onc lus io n A ms ta r s co re N on ‐s te ro id al a nt i‐i nf la m m at or y dr ug Sw am y et a l, 20 07 15 8 RC T A ller gi c co nj unc tiv iti s (n = 7 12 ) O ph ta lmic N SA ID ((k et oro la c, dic lo fe na c, flu rbip ro fe n) pi ro xi ca m a nd hy dr oc or tis on e) v s pl ac eb o Sy m pt om s, o cu la r itc hi ng , a nd co nj un ct ival in je ct io n Si de e ff ec ts Itc hi ng S M D − 0. 54 [− 0. 84 ; − 0. 24 ] La cr im at io n SM D −0 .2 1 [− 0. 41 ; − 0. 01 ] C on ju nc tival in je ct io n SM D − 0. 52 [− 0. 97 ; − 0.0 5] O cu la r d is co m fo rt w ith tr ea tm en t S M D 3. 97 [2 .6 7; 5 .8 9] N SA ID a re m or e ef fe ct iv e th an pl ac eb o in re du ci ng co nj un ct ival it ch ing an d im pr ov in g a ca rdina l s ig n Low W ils on e t a l, 20 15 16 8 cl in ic al tr ia ls 2 re vi ew s Se as on al a lle rg ic co nj unc tiv iti s (n um be r o f pa rt ic ipa nt s no t sp ecif ie d) O pht al m ic n on‐ ste ro i‐ da l a nt i‐i nf la m m a‐ to ry d ru gs (K et or ol ac 0. 5% a nd d ic lo fe na c 0.1 % ) Sy m pt om s sc or e cha ng e D ec re as e sh or t‐ te rm tr ea tm en t i n co mpa riso n w ith pl ac eb o (7 ‐1 4 d) in 3 st ud ie s; 2 c ro ss ‐o ve r w ith ou t b en ef it ke to ro la c 0. 5% . D ic lo fe na c 0. 1% be tt er th an k et or ol ac 0. 5% in 1 tr ia l f or sy m pt om s. D at a no t po ole d. Ef fe ct iv e in d ec re as ‐ in g sh or t‐ te rm sy mp to m s C rit ic al ly lo w Le uk ot rie ne a nt ag on is t ( m on te lu ka st ) G an e et a l, 20 13 17 18 R C T 6 m et a‐ an al ys is O cu la r e ye d is ea se 12 S A C , 5 P A C (n = 9 01 7 ad ul t) (n = 1 75 c hi ld re n 2‐ 14 y ) Le uk ot rie ne re ce pt or an ta go ni st s (m on te lu ka st) O cu la r s ym pt om sc or es LT RA v s p la ce bo (6 RC T) S M D − 0. 10 [− 0. 14 :− 0.0 7] LT RA v s o ra l an tih is ta m in e ( 3 R C T) 0. 08 [0 .0 2; 0 .1 4] in fa vo r o f a nt ih is ta ‐ min es LT RA a nd o ra l an tih is ta m in e v s pl ac eb o (2 R C T) −0 .3 0 [− 0. 38 ; − 0. 21 ] In s ea so na l A C , L TR A s ar e m or e ef fic ac io us th an p la ce bo b ut le ss ef fic ac io us th an o ra l an tih is ta min es in ad ul t p at ie nt s. M od er ate A C , a lll er gi c co nj un ct iv iti s; C C T, c or tic os te ro id s; L TR A , l eu ko tr ie ne re ce pt or a nt ag on is ts ; N SA ID , n on ‐s te ro id al a nt i‐i nf la m m at or y dr ug ; P A C , p er en ni al a lle rg ic c on ju nc tiv iti s; R C T, ra nd om ize d cl in ic al tr ia ls ; S A C , s ea so na l a lle rg ic c on ju nc tiv iti s; S M D , s ta nd ar di ze d m ea n di ff er en ce .
Overall, topical antihistamines and mast cell stabilizers appear to be safe and well tolerated.6,11 The most frequently reported side effects from the use of these agents were burning and stinging sen‐ sation, blurred vision and unacceptable aftertaste.5,6 Data on their long‐term efficacy and safety are still lacking. To minimize possible toxic effects of preservative compounds on the ocular surface, single‐ dose preservative‐free eye drops should be used whenever possible. A SR of 20 RCT evaluated the efficacy of topical antihistamines and mast cell stabilizers for the treatment of VKC showing an improvement of ocular symptoms score with use of all these drugs.12 The pooled data were unable to recommend use of one agent over the other. A RCT published after this SR showed benefit with improved inflamma‐ tory biomarkers and total symptom score using preservative‐free N‐ acetyl‐aspartyl‐glutamic acid (NAAGA) compared to levocabastine.13 The treatment of AKC with antihistamines and mast cell stabiliz‐ ers has only been reported in a few case reports and case series.14 Recommendations
• All topical drugs are effective in reducing signs and symptoms ⨁⨁⨁⨁↑↑ • Topical antihistamines and dual‐acting drugs may have lead to a quicker onset symptom relief when compared to mast cell stabi‐ lizers ⨁◯◯◯↑? • Dual‐acting agents with combined mast cell stabilizer and antihis‐ taminic function provide better symptom control ⨁◯◯◯↑? • Mast cell stabilizers such as chromones require multiple daily
doses and have a delayed onset of action, hence are less prefera‐ ble ⨁◯◯◯↑?
• SAC and PAC can be managed using the same drugs ⨁⨁⨁⨁ ↑↑ • The duration of treatment is longer in PAC compared to SAC
⨁◯◯◯↑?
• Topical antihistamines and mast cell stabilizers can be used in VKC ⨁⨁◯◯↑ and AKC ⨁◯◯◯↑?
• All these drugs can be used in combination ⨁◯◯◯↑?
3.1.2 | Topical alpha‐adrenergic agonists
(vasoconstrictors)
Topical decongestants are frequently used as first‐line treatment due to their availability over the counter.4 They merely alleviate
hyperemia, having little to no relief from itch and a short duration of action.7 In a recent randomized controlled trial comparing several treatment options, the use of naphazoline/antazoline was associ‐ ated with lower tolerability profile of all treatment. They may cause side effects such as rebound redness, chronic follicular conjunctivi‐ tis, and tachyphylaxis. In older formulations, ocular decongestants are paired with topical first‐generation antihistamines, such as phe‐ niramine and antazoline, to relieve both itching and redness. Recommendations • Vasoconstrictors alleviate only hyperemia ⨁◯◯◯ ↑?
• They should be used with caution and for a short period of 5‐7 days because of side effects and tachyphylaxis (TF expert opinion)↑↑
3.1.3 | Non‐steroidal anti‐inflammatory drugs
NSAID (topical prostaglandin and oral leukotriene
inhibitors)
One SR15 based on 8 RCTs concluded that topical NSAIDS are more effective than placebo in reducing ocular itching and redness. Use of varied outcome parameters did not permit a comparison15,16 (Table 3). NSAIDs are rarely used due to their local side effects, such as burning/stinging after application.
The oral leukotriene inhibitor montelukast has shown to be use‐ ful in the treatment of ocular symptoms in SAC and PAC, but less effective than oral antihistamines.17
Recommendations from the TF group
• NSAIDs are effective for their short‐term use but do not target specific inflammatory mechanisms ⨁◯◯◯↓? • In adult SAC patients, leukotriene inhibitors are less efficacious than oral antihistamines ⨁◯◯◯↑?
3.1.4 | Systemic antihistamines
Oral antihistamines are frequently used in case of allergic comorbidi‐ ties such as rhinitis and are used in almost one‐third of the patients with ocular symptoms.4 Drugs such as loratadine, desloratadine,18 and fexofenadine19 are highly effective for the treatment of allergic TA B L E 4 Systemic antihistaminesAuthor, Y Studies design Participants
Intervention
comparisons Outcomes Main results
Author’s conclusion Amstar score Compalati et al, 201320 4 RCT Allergic rhinoconjunc‐ tivitis (n = 1135) Rupatadine vs ebastine; placebo (n = 473) Rupatadine vs loratadine; placebo (n = 283) Rupatadine vs desloratadine; placebo (n = 379) Itchy and watery eyes Itch eyes SMD: −0.29, 95% CI −0.45 to −0.14 Watery eyes reduction SMD: −0.25, 95% CI −0.45 to −0.06 Improvement ocular symptom of rupatadine vs placebo. Low RCT, randomized clinical trials; SMD, standardized mean difference.
T A B LE 5 C or tic os te ro ids a nd c al cin eu rin in hibi to rs A ut ho r, Y St ud ies de sig n Pa rti ci pa nt s Int er ve nt io n co m pa ris ons O ut co me s M ain re su lt s A ut ho r’s c onc lus io n A ms ta r s co re To pic al c or tic os te ro ids O 'G al la gh er e t a l, 20 17 84 1 RC T B lep ha ro co nj unc tiv iti s (n = 1 37 c hi ld re n) Lo tep re dno l et ab on ate Im pr ov em en t o f s ym pt om s El imina tio n cl in ic al s ig ns A dv er se e ff ec ts N o su ff ic ie nt d at a on th e im pr ov em en t i n sy m pt om s or si gn s; n o di ff er en ce o n ad ve rs e ef fe ct s N o hi gh ‐q ua lit y ev id en ce reg ar din g sa fe ty a nd e ff ic ac y of to pi ca l t re at m en ts fo r B KC H ig h Sh ep pa rd e t a l 20 16 24 40 c lin ic al tr ia ls SA C (4 ) PA C (1 ) V KC (1 ) B KC (3 ) SA C (n = 8 56 ) PA C (n = 1 59 ) V KC (n = 3 7) B KC (n = 3 55 ) Lo tep re dno l et ab on ate Inc idenc e of IOP 0. 2% s us pe ns io n th er e w as n o in cr ea se in IO P fo r S A C o r P A C ; 0. 5% s us pe ns io n th er e w as n o in cr ea se in V KC o r S A C (b ot h in co mpa riso n w ith v eh ic le ) Fa vo ra bl e IO P sa fe ty pr of ile fo r l ot ep re dn ol et ab on at e w ith b ot h sh or t‐ te rm a nd lo ng ‐t er m u se C rit ic al ly lo w W u et a l, 20 15 23 8 RC T SA C (4 RC T), G PC (3 RC T) V KC (1 RC T) (n = 1 44 5) Lo tep re dno l et ab on at e vs pl ac eb o; to pi ca l olo pa ta di ne ; t op ic al flu or om et ho lo ne ac et ate O cu la r s ym pt om s (o cu la r itc hi ng ) S ig n (b ul ba r co nj un ct iv al in je ct io n or pa pi llae ) In cr ea se d in tr ao cula r pr es su re (I O P) C om pa re d to p la ce bo: Si gn s ev er ity S M D − 0. 85 [− 1. 35 ; −0 .3 5] (a ll) SA C − 0. 45 [− 0. 62 ; − 0. 28 ]; on ly on e tr ia l G PC a nd V KC W ei gh te d m ea n di ff er en ce − 0. 66 [− 0. 97 ; − 0. 35 ] ( al l) SA C − 0. 43 [− 0. 46 ; − 0. 31 ]; on ly on e tr ia l G PC a nd V KC IO P O R 3. 03 [1 .0 4; 8 .8 0] C ompa re d to to pi ca l o lo pa ta di ne : Si gn s ev er ity S M D − 3. 78 [− 10 .6 1; 3. 04] W M D − 0. 98 [− 2. 00 ; 0 .0 5] (a ll inte rv ent io ns ) To pi ca l l ot ep re dn ol et ab on at e is e ff ec tiv e in tr ea tin g al le rg ic co nj unc tiv iti s H ig h N as al c or tic os te ro id s W ei ne r e t a l, 19 98 26 16 R C T A lle rgi c rhi no co nj un c‐ tiv iti s (n = 2 26 7) N as al c or tic os te ro id s vs o ra l a nt ih is ta ‐ min es (t er fe na din e; as te m iz ole ; lo ra ta di ne ; ce tir iz in e) O cula r s ym pt om s (in cl ud ed 11 s tu di es ) N as al s te ro id v s or al a nt ih is ta ‐ min es SM D − 0. 04 3 [− 0. 15 7; 0 .0 72 ] Th er e w as n o si gn ifi ca nt di ff er enc e be tw een in tr ana sa l c or tic os te r‐ oi ds a nd o ra l an tih is ta m ine s on oc ul ar s ymp to m s Low H on g et a l, 20 11 27 32 s tu di es RC T SA C a nd P A C (n = 6 57 3) N as al c or tic os te ro ids To ta l o cu la r s ym pt om sc or e (T O SS ) D at a no t p oo le d Im pr ov em en t o f T O SS in 9 o ut o f 10 s tu di es To ta l e ye s ym pt om s 5 ou t o f 1 3 st ud ie s In tr an as al c or tic os te r‐ oi ds h av e a po si tiv e im pa ct o n th e on th e TO SS o f A R C rit ic al ly lo w (Co nt in ue s)
A ut ho r, Y St ud ies de sig n Pa rti ci pa nt s Int er ve nt io n co m pa ris ons O ut co me s M ain re su lt s A ut ho r’s c onc lus io n A ms ta r s co re N ac le rio e t a l, 20 08 28 3 SR 5 RC T A lle rgi c rhi no co nj un c‐ tiv iti s TA A (n = 3 75 ) FP (n = 1 64 5) M F (n = 1 19 8) FF (n = 9 40 ) B U D (n = 2 80 ) N as al c or tic os te ro ids Tr ia m ci no lo ne ac et on id e (n = 3 75 ) Pr opi ona te Fl ut ic as on e (7 R C T da ta a ss oc ia tio n) M om et aso ne fu ro at e (2 R S 1 RC T) Fu ro at e flu tic as on e (2 R C T) B ud es on id e (1 R C T) To ta l o cu la r s ym pt om sc or e D at a no t p oo le d, a n im pr ov em en t of to ta l e ye s ym pt om s co re w as se en v s pl ac eb o w as s ee n in a ll cl in ic al tr ia ls a nd m et a‐ an al ys is In tr an as al c or tic os te r‐ oi ds a re e ff ec tiv e an d w el l t ol er at ed in th e tr ea tm en t o f o cu la r sy m pt om s as so ci at ed w ith a lle rgi c rhi nit is . C rit ic al ly lo w Yá ne z et a l, 20 02 29 4 RC T A lle rgi c rhi nit is B ec lo m et ha so ne (n = 1 66 ) B U D (n = 3 1) Fl ut ic as on e (n = 1 93 ) Fl un is ol id e (n = 3 8) A ze la st in e (n = 2 40 ) Le vo ca ba st ine (n = 4 08 ) B ec lo m et ha so ne o r flu ni so lid e vs aze la st in e (n = 2 RC T) B ud es on id e or flu tic as on e vs le vo ca ba st in e (n = 2 RC T) Ey e sy m pt om s N as al s te ro id v s na sa l a nt ih is ta ‐ m in es S M D − 0. 07 [− 0. 27 ; 0 .1 2, P = 0. 4] Th er e w as n o di ff er en ce be tw een in ter ven tio ns in th e re lie f o f o cu la r sy mp to m s C rit ic al ly lo w To pi ca l c yc lo sp or ine W an e t a l, 20 13 32 7 RC T A ller gi c co nj unc tiv iti s (n = 3 06 e ye s of 1 53 pa tie nt s) 3 s tu di es re cr uit ed s te ro id ‐d e‐ pen den t a ller gi c co nj unc tiv iti s To pi ca l c yc lo sp or ine in c on ce nt ra tio n fr om 0 .0 5% to 2 % C om po si te s ig n sc or e (a ve ra ge o f a t l ea st o ne o f th e fo llo w in g si gn s: hy pe re m ia , s w el lin g, pa pi llae a nd g ia nt pa pi llae on th e ta rs al c on ju nc tiv a, hy pe re m ia a nd e de m a of the b ul ba r co nj un ct iv a, o r c or ne al in vo lv em en t) C om po si te sy m pt om s co re (a ve ra ge of : r ed ne ss , t ea rin g, bu rn in g, d is co m fo rt , fo re ig n bo dy s en sa tio n, di sc ha rg e, a nd p ho to ph o‐ bi a) M ed ic at io n us e Com pa re d t o p lac eb o: C om po si te s ig n sc or e: S M D − 1. 21 95 % C I, [− 1. 80 ; − 0. 62 ] Co m po sit e s ym pt om sco re : S M D −0 .8 4 95 % C I[− 1. 51 ; − 0. 16 ] Re du ct io n o n s te ro id e ye d ro p (3 RC T) S M D − 61 .2 [− 10 1. 6; − 20 .7 ] To pi ca l c yc lo sp or ine co ul d be a n ef fe ct iv e an d sa fe tr ea tm en t m et ho d fo r a lle rg ic co nj unc tiv iti s Low T A B LE 5 (Co nti nue d) (C on tin ue s)
A ut ho r, Y St ud ies de sig n Pa rti ci pa nt s Int er ve nt io n co m pa ris ons O ut co me s M ain re su lt s A ut ho r’s c onc lus io n A ms ta r s co re G on zá lez ‐L ópez e t al , 2 01 2 33 3 RC T A to pi c ke ra to co nj un c‐ tiv iti s (n = 5 8) C yc lo sp or in e 0. 05 % or c yc lo sp or in e 2% in m ai ze o il vs pr es er va tiv e‐ fr ee ar tif ic ia l t ea rs o r pl ac eb o Sy m pt om s im pr ov em en t (re po rt ed b y th e pa rt ic ip an t) itch in g, te ar in g, d is co m fo rt , m uc ous di scha rg e, ph ot op ho bi a or p ai n To pi ca l s te ro id u se C lin ic al s ig ns A dv er se e ff ec ts N ot p oo le d Sy m pt om s co m po si te s co re si gn ifi ca nt ly im pr ov ed fo r a ll as so ci at ed , b ut n ot fo r s pe ci fic sy m pt om s in o ne s tu dy (C lin ic al si gn s im pr ov ed in th e co m po si te sc or e in o ne s tu dy ) Re du ct io n of to pi ca l s te ro id u se in o ne s tu dy To pi ca l C sA m ay pr ov id e cl in ic al a nd sy m pt om at ic re lie f i n A KC a nd m ay h el p to re du ce to pi ca l s te ro id us e in p at ie nt s w ith st er oi d‐ dep en den t o r st er oi d‐ re si st an t A KC . N o se rio us a dv er se ev en ts w er e re po rt ed H ig h M an te lli e t a l, 20 07 12 27 R C T 10 met a‐a na l‐ ys is Ve rn al Ker at oc on ju nc iti vi s (n = 1 09 2 pa tie nt s, 21 84 e ye s) m ea n ag e 13 .3 (4 .5 y ) M as t c el l s ta bi lize rs vs p la ce bo (n = 1 0) M as t c el l s ta bi lize rs vs a no th er (n = 8 ) M as t c el l s ta bi lize rs vs c or tic os te ro id s (n = 2 ) M as t c el l s ta bi lize rs vs a nt ih is ta m in es (n = 1 ) N SA ID v s pl ac eb o (n = 2 ) N SA ID v s C C T (n = 1 ) A nt im ito tic d ru g (n = 1 ) Itc hi ng , t ea rin g, fo to fo bi a, hy pe re m ia , t ar sa l p ap ill ae , lim ba l d is ea se , a nd co rn ea l i nv olv emen t Itc hi ng (m ito m yc in ; s od iu m cr om og lic at e, c yc lo sp or in e 2% , ke to ro la c) S M D − 1. 43 [− 1. 76 ; −1 .1 0] Te ar in g (m ito m yc in , s od iu m cr om og lic at e, c yc lo sp or in e 2% ) SM D − 0. 84 [− 1. 20 ; − 0. 49 ] Ph ot op ho bi a (m ito m yc in , s od iu m cr om og lic at e, c yc lo sp or in e 2% ) −0 .2 7 [− 0. 82 ; 0 .3 9] To ta l s ig ns (c yc lo sp or in e an d so di um c ro m og lic at e) S M D − 0. 94 [− 1. 34 ; − 0. 54 ] To ta l s ym pt om s (c yc lo sp or in e 2% an d so di um c ro m og lic at e) S M D −0 .7 3 [− 1. 14 ; − 0. 32 ] Ta rs al p ap ill ae (m ito m yc in , so di um c ro m og lic at e, c yc lo ‐ sp or in e) S M D − 0. 32 [− 0. 64 :− 0.0 0] C or ne al In vo lv em en t ( m ito m yc in , so di um c ro m og lic at e, c yc lo ‐ sp or in e) S M D − 1. 15 [− 1. 50 ; −0 .8 0] Li m ba l d is ea se (m ito m yc in , so di um c ro m og lic at e, c yc lo ‐ sp or in e) S M D − 1. 17 [− 1. 50 ; −0 .8 3] H yp er em ia (m ito m yc in , s od iu m cr om ogl ic at e, c yc lo sp or in e, m ip ra go si de 0 .5 ) S M D − 1. 07 [− 1. 38 ; − 0. 76 ] Th e cu rr en tly a va ila bl e to pi ca l d ru gs a re ef fe ct iv e in tr ea tin g ac ut e ph as es o f V KC . H ow ev er , t he re is a la ck o f e vi de nc e to su pp or t t he re co m ‐ m en da tio n of o ne sp ec ifi c ty pe o f m ed ic at io n fo r t re at in g th is d is or der Low (C on tin ue s) T A B LE 5 (Co nti nue d)
rhinoconjunctivitis (ARC) (Table 4). Most of the SRs have addressed total symptoms scores,18,19 without evaluating impact on specific ocular symptoms. Itching and watery eye symptoms significantly im‐ proved after rupatadine treatment compared to placebo.20
While the drowsiness so commonly noted with the older first‐ generation systemic antihistamines has improved in the newer second‐generation antihistamines, some of the new molecules still inhibit muscarinic receptors, leading to mucosal dryness.21,22 Moreover, patients with dry eye have reduced barrier function at the mucosal interface against environmental allergens and pollut‐ ants and possibly a lower threshold for allergen response. Some oral antihistamines may exacerbate OA by lowering the barrier defense offered by a healthy tear film. Recommendations • Systemic antihistamines should be used in case of comorbidities that require it use ⨁◯◯◯↑? • Some systemic antihistamines may induce drying effects, particu‐ larly relevant at the ocular surface barrier ⨁◯◯◯↑?
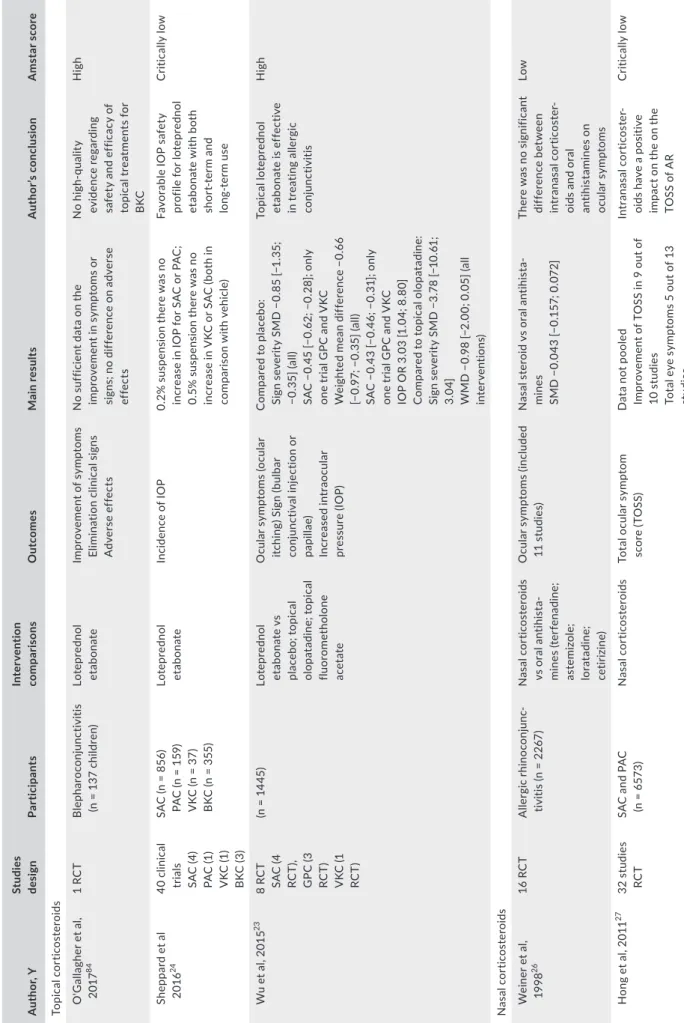
3.1.5 | Corticosteroids
Should not be the first choice of therapy for OA. In clinical practice, they are the most effective anti‐inflammatory agents in active OA. Because of potential adverse effects (increased intraocular pressure, with a potential evolution toward glaucoma, cataract formation, bacterial, viral and fungal superinfections), their use must be moni‐ tored by an ophthalmologist (especially in prolonged treatments). A SR (Table 5) on the use of a loteprednol eye drops for treating SAC (4 RCTs) and VKC (1 RCT) reached a high level of confidence using AMSTAR2 score,23 supporting the efficacy of this treatment. Loteprednol 0.5% and 0.2% were considered effective in treating signs and symptoms of SAC, but should be used with caution due to the higher incidence of intraocular pressure (IOP) elevation (pooled odds ratio = 3.03) compared with placebo and olopatadine.23 A sec‐ ond review demonstrated significantly lower rates of IOP elevation (≥10 mm Hg) when compared to topical prednisolone 1% or dexa‐ methasone 0.1%, suggesting a favorable IOP safety profile for lotep‐ rednol with both short‐term and long‐term use. However, this review received a critically low AMSTAR score.24A wide variety of corticosteroid eye drops of different poten‐ cies are available across the world (Table 1).1 There are no studies directly comparing formulation, strength or regimen of any specific corticosteroid over another for the treatment of OA. There are two main regimens used in OA: (a) pulsed therapy of 3‐4 drops per day for 3‐5 days and (b) prolonged treatment of 1‐3 weeks, tapered slowly over several days. Pulsed therapy is the favored treatment of acute exacerbations of VKC and AKC, especially when the cornea is involved. The potency and treatment duration of the topical corti‐ costeroid should be chosen clinically based on the severity of ocular inflammation and corneal involvement.
The beneficial effect of intranasal corticosteroids (INCs) on ocular symptoms has been demonstrated in several studies suggesting that
A ut ho r, Y St ud ies de sig n Pa rti ci pa nt s Int er ve nt io n co m pa ris ons O ut co me s M ain re su lt s A ut ho r’s c onc lus io n A ms ta r s co re Ta cr ol im us Zh ai e t a l 2 01 0 36 2 RC T 4 C as e se rie s V KC (n = 8 7) A KC (n = 3 5) PA C (n = 2 0) 0. 1% ta cr ol im us op ht ha lmic su sp ens io n 0. 03 % ta cr ol im us Ta cr ol im us oi nt m en t v s cl ob et as ol A KC To ta l o bj ec tiv e sc or e Sy mp to m sc or e U lc er im pr ov emen t N ot p oo le d Im pr ov em en t o f t ot al s co re w ith ta cr ol im us v s pl ac eb o (− 5. 6 ± 5. 1 fo r t acr ol im us o ph tha lmic su sp en si on v s −0 .1 ± 4 .5 fo r pl ac eb o) Si m ila r e ff ec t t o to pi ca l co rt ic os te ro id s fo r A KC N ee de d m or e st ud ie s C rit ic al ly lo w C C T, c or tic os te ro id s; IO P, in tr ao cu la r p re ss ur e; N SA ID , n on ‐s te ro id al a nt i‐i nf la m m at or y dr ug ; R C T, ra nd om ize d cl in ic al tr ia ls ; T O SS , t ot al o cu la r s ym pt om s co re . T A B LE 5 (Co nti nue d)
T A B LE 6 A lle rg en ‐s pe ci fic im mu no th er ap y A ut ho r, Y St ud ies d es ig n Pa rti ci pa nt s Int er ve nt io n co m pa ris ons O ut co me s M ain re su lt s A ut ho r’s c onc lus io n A m st ar sco re Imm un ot he ra py D ha m i e t a l, 20 17 45 16 0, 1 34 D B RC T 61 S C IT ; 7 1 SL IT A lle rg ic rhi no co nj un c‐ tiv iti s or al le rgi c rhi nit is 63 79 p at ie nt s SCI T 13 6 36 pa tien ts SL IT W ee d, tr ee a nd g ra ss po lle ns , m ol ds , c at an d do g da nd er , an d ho us e du st m ite s D iff er en ce s ym pt om sc or e Di ff er enc e me di ca tio n sc or e Di ff er enc e Q oL Sy mp to m sc or e [S M D − 0. 53 (9 5% C I − 0. 63 to − 0. 42 ); SC IT −0 .6 5 (− 0. 86 to − 0. 36 ) v s SL IT − 0. 48 (9 5% C I −0 .6 1 to − 0. 36 ); Se as on al a lle rg en s −0 .3 7 (9 5% C I − 0. 45 to − 0. 28 )] Me di ca tio n sc or e SM D o f − 0. 38 (9 5% C I − 0. 49 , − 0. 26 ) [ SC IT SM D − 0. 52 (9 5% C I − 0. 75 , − 0. 29 ); SL IT − 0. 31 (9 5% C I − 0. 44 , − 0. 18 )] A IT is e ff ec tiv e in ac hie vi ng c lin ic all y imp or ta nt sho rt ‐t er m im pr ov em en ts in sy mp to m , m ed ic at io n, a nd co mb ine d sy m pt om a nd me di ca tio n sc or es H ig h D i B on a et al 47 2 01 5 13 R C T Se as on al al le rg ic rhi no co nj un c‐ tiv iti s (n = 4 65 9) G ra ss p ol le n SL IT v s pl ac eb o Ph le um p 5 or 5 gr as s ex tr ac ts D iff er en ce in s ym pt om sc or e Di ff er enc e me di ca tio n sc or e N um be r a dv er se ev ent s Sy m pt om s co re (S M D , − 0. 28 ; 9 5% C I, −0 .3 7 to −0 .1 9; P < 0 .0 01 ) M ed ic at io n sc or e (S M D , − 0. 24 ; 9 5% C I, −0 .3 1 to − 0. 17 ; P < 0 .0 01 ) O R ad ve rs e ev en ts 2 .9 1 Sm al l b en ef it of gr as s SL IT ta bl et s in th e tr ea tm en t o f S A RC M od er ate N el so n et a l, 201 5 48 37 R C T 14 S LI T ta bl et ; 1 4 SL IT d ro p; 9 SC IT A lle rgi c rhi nit is tr ea te d w ith IT (n = 4 01 6) a nd pl ac eb o (n = 3 74 3) SC IT v s SL IT g ra ss pol le n IT v s pl ac eb o SL IT ta bl et s vs S LI T dro ps D iff er en ce in s ym pt om sc or e (rh ino co nj unc ti‐ vit is s co re p re fe rre d) Di ff er enc e me di ca tio n sc or e Sy m pt om s co re [S C IT v s pl ac eb o SM D s (9 5% C I): −0 .3 2 (− 0. 45 to − 0. 18 ); SL IT v s pl ac eb o SM D s (9 5% C I): − 0. 32 (− 0. 41 to − 0. 23 )] M ed ic at io n sc or e [S C IT v s pl ac eb o SM D s (9 5% C I): − 0. 33 (− 0. 52 to − 0. 13 ); SL IT v s Pl ac eb o SM D s (9 5% C I): − 0. 44 (− 0. 83 to − 0. 06 )] N o di ff er en ce b et w ee n SC IT o r S LI T C ompa ra bl e re du ct io n in al ler gi c co nj unc ti‐ vi tis s ym pt om s w ith S LI T an d SC IT M od er ate D ev ill ie r e t a l, 20 14 49 38 D B RC T 28 m ed 10 S LI T Se as on al al le rgi c rhi nit is (n = 2 1 22 3) A nt ih is ta min es (d es lo ra ta di ne ; bi la st in e; lo ra ta di ne ; fe xo fe na din e; ce tir iz in e); N as al C C T; m on te lu ka st a nd gr as s po lle n SL IT ta bl et, Sy mp to m s sc or e C omb ine d sy mp to m ‐ me di ca tio n sc or e Re la tiv e cl in ic al impa ct Re po rt ed p os t‐ tr ea t‐ m en t o r s ea so n‐ lo ng nas al To ta l s ym pt om s co re s. 10 0 × (s co re P la ce bo – sc or e A ct iv e) /s co re Pl ac eb o) Fi ve g ra ss p ol le n SL IT ta bl et s [− 0. 30 (− 0. 36 , −0 .2 3) ]; −2 9. 6% (− 23 % to − 37 % ) Ti m ot hy S LI T ta bl et s −1 9. 2% (− 6% to − 29 % ) N as al c or tic os te ro id s [− 0 .5 5 (− 0. 63 , − 0. 47 )] −2 3. 5% (− 7% to − 54 % ) aze la st in e‐ flu tic as on e [S M D − 1. 00 (− 1. 10 , −0. 90 )] −1 7. 1% (− 15 % to − 20 % ) H 1‐ an tih is ta m in es [S M D − 0. 39 (− 0. 43 , − 0. 35 )] −1 5. 0% (− 3% to − 26 % ) M on te lu ka st [− 0. 23 (− 0. 30 , − 0. 16 )] −6 .5 % (− 3% to − 10 % ) G ra ss p ol le n SL IT ta bl et s ha d a gr ea te r m ea n re la tiv e cl in ic al im pa ct th an se co nd ‐g ene ra tio n an tih is ta m ine s an d m on te lu ka st a nd si m ila r t o th e m ea n re la tiv e cl in ic al im pa ct o f n as al co rt ic os te ro ids M od er ate Li n et a l, 20 13 50 RC T 13 S LI T Co nj unc tiv iti s (n = 1 07 4) SL IT Grass m ix , d us t m ite , p ar ie ta ria , tim ot hy g ra ss , ol iv e, tr ee m ix Sy mp to m sc or e N o po ol ed A ll bu t t w o st ud ie s sh ow ed a g re at er im pr ov e‐ m en t i n SL IT M od er at e st re ng th in s up po rt o f S LI T fo r t re at in g al le rg ic co nj unc tiv iti s H ig h (C on tin ue s)
A ut ho r, Y St ud ies d es ig n Pa rti ci pa nt s Int er ve nt io n co m pa ris ons O ut co me s M ain re su lt s A ut ho r’s c onc lus io n A m st ar sco re C al de ro n et al , 2 01 1 51 RC T 42 A lle rg ic co nj unc tiv iti s se as on al a nd pe re nni al (n = 3 39 9) SL IT G ra ss , m ite s, w ee ds v s pl ac eb o TO SS In di vi du al s ym pt om sc or e Me di ca tio n sc or e C on ju nc tival im m ed ia te a lle rg en sen si tiv ity TO SS (n = 3 6 st ud ie s) S M D − 0. 41 [− 0. 53 ; − 0. 28 ], no t s ig ni fic an t f or p er en ni al a lle rg en s (n = 6 ) an d si gn ifi ca nt fo r c hi ld re n an d ad ul ts Itc h SM D − 0. 31 [− 0. 42 ; − 0. 20 ] W at er y ey es S M D − 0. 23 [− 0. 34 ; − 0. 11 ] Re d ey es S M D − 0. 33 [− 0. 45 ; − 0. 22 ] N o si gn ifi ca nt d iff er en ce s in m ed ic at io n sc or e SL IT is e ff ec tiv e in re du ci ng to ta l a nd in di vi du al sy m pt om s co re in su bj ec ts w ith A RC or c on ju nc tiv iti s. H ig h K im e t a l, 20 13 52 RC T 3 SC IT 5 SL IT Co nj unc tiv iti s (n = 5 13 ) A IT p ol le n an d du st m ite Pe rc en t d iff er en ce in pr e‐ to‐ po st cha ng e fo r c on ju nc tiv iti s sy m pt om s (< 15 % w ea k; 1 5‐ 40 m od er at e; > 40 % st ro ng ) W ith ou t s pe ci fic v al ue s of p er ce nt o f i nc re as e fo r c on ju nc tiv iti s. SC IT s ho w ed a n im pr ov em en t v s pl ac eb o in a ll st ud ie s an d 4 ou t o f 5 s tu di es s ho w ed a n im pr ov em en t w ith S LI T. Th e st re ng th o f ev id en ce is lo w fo r SC IT a nd m od er at e fo r S LI T in c on ju nc tiv iti s sy mp to m s im pr ov emen t M od er ate Rö de r e t a l, 20 08 55 RC T 6 SC IT 4 LN IT 7 O IT 11 S LI T A lle rg ic rhi no co nj un c‐ tiv iti s (n = 1 61 9) 19 tr ia ls w ith se as on al a lle rg en (g ra ss p ol le n) 9 tr ia ls (h ou se d us t m ite) Sy mp to m s sc or es Me di ca tio n sc or es D id n ot p re se nt s pe ci fic d at a; n ot p oo le d Insu ff icie nt ev idenc e th at im m un ot he ra py in an y ad m in is tr at io n ha s a po si tiv e ef fe ct o n sy mp to m s an d/ or m edic at io n Low D B RC T, d ou bl e‐ bl in d ra nd om ize d co nt ro lle d tr ai l; IT , a lle rg en im m un ot he ra py ; L N IT , n as al im m un ot he ra py ; O IT , o ra l i m m un ot he ra py ; R C T, ra nd om ize d cl in ic al tr ia ls ; S C IT , s ub cu ta ne ou s im m un ot he ra py ; SL IT , s ub lin gu al im m un ot he ra py ; S M D , s ta nd ar di ze d m ea n di ff er en ce . T A B LE 6 (Co nti nue d)
their reduction is mediated via the ocular‐nasal reflex inhibition. The variability of the effect depends on the affinity of the drug to its gluco‐ corticoid receptor.25 Four SR evaluated the use of INCs for the treatment of ocular symptoms associated with allergic rhinitis26,27 (Table 5) showing that INCs are well tolerated and effective in reducing the total ocular symptom score (TOSS), even though the outcome measures were not designed to focus specifically on ocular symptoms. It is noted that oral/ topical antihistamines are not superior to INCs in reducing TOSS.28,29 However, despite large patient cohorts, all SR had a low or critically low confidence rating of results according to AMSTAR2. A recent metanal‐ ysis of 3 RCTs noted benefit of a topical nasal combination, fluticasone propionate, and azelastine on TOSS in patients with seasonal ARC.30
There are no studies specifically comparing INCs against each other for the treatment of ocular symptoms. Although data are scarce, there is no evidence that INCs used for prolonged periods of several months increase the risk of cataract formation, intraocular hypertension, and glaucoma, since they have little or no systemic absorption (fluticasone and mometasone).30
The use of corticosteroids as dermatologic applications in OA is reserved for AKC and CBC.1 Lowest appropriate potency cortico‐ steroids, such as hydrocortisone or budesonide on the eyelid skin, are recommended for the treatment of severe acute eyelid eczema.
Supra‐tarsal injections of dexamethasone sodium phosphate, triamcinolone acetonide, or hydrocortisone sodium succinate have been proposed to treat recalcitrant AKC and VKC cases,31 but should only be used by specialists with caution in severe patients unresponsive to other treatments. Systemic corticosteroids may be used as short course in selected severe hyperacute exacerbations involving either eyelid skin or cor‐ nea especially in VKC and AKC. Recommendations • Topical corticosteroids eye drops should be used with caution under ophthalmologist's monitoring and preferably for shorter duration due to the high risk of local and potential blinding side effects ⨁◯◯◯↑↑ • For the treatment of SAC and PAC, topical corticosteroids are
rarely needed ⨁◯◯◯↓↓ • Corticosteroid eye drops can be used preferably as short, pulsed therapy in acute exacerbations of OA, especially in VKC and AKC or when the cornea is involved under ophthalmologist supervision (TF expert opinion)↑↑ • INCs are effective and well tolerated in the treatment of ocular symptoms associated with ARC ⨁◯◯◯ ↑? • INCs should not be used if only ocular signs and symptoms are present (TF expert opinion) ↓↓
• Topical skin corticosteroid applications should be used in the acute phase of eyelid eczema, with a preference for low potency corticosteroids (TF expert opinion) ↑?
3.1.6 | Calcineurin inhibitors
Topical calcineurin inhibitors are the most frequently used treat‐ ments as steroid‐sparing agents in steroid‐dependent cases of
VKC and AKC. Two SR evaluated the use of topical cyclosporine (CsA) in VKC and AKC32,33 (Table 5). The first one showed that topical CsA is effective in alleviating the signs and symptoms of VKC and AKC, reducing the dependency on topical steroid eye drops while maintaining similar safety profile as of placebo. The second SR highlighted the relative scarcity of RCTs assessing the efficacy of topical CsA in AKC and suggested that CsA provides clinical and symptomatic improvement and may help in reducing topical steroid use in patients with steroid‐dependent or non‐ster‐ oid‐responsive AKC.33 Compounded formulations of CsA are prepared in many coun‐ tries by hospital and retail pharmacies with differing excipients, pro‐ cesses, and quality. Drug concentrations range from 0.05% to 2% and posology from 1 to 6 instillations daily.
Cyclosporine 0.1% cationic emulsion (CE) is commercially available for the treatment of severe dry eye disease.34 The same formulation has obtained in 2018 the marketing authorization by EMA for the treatment of severe VKC. Severe VKC patients treated with this formulation achieved significant improvements in signs, symptoms, and QoL compared with patients who received vehicle alone.35
Tacrolimus 0.03%‐0.1% eye drops or ointments have been proposed for the treatment of severe, refractory cases of AKC and VKC. A commercial eye drop preparation is available only in Asia with the indication of severe AKC and VKC. One review, with a critically low quality of evidence score, highlighted the benefits of tacrolimus over placebo in 2 RCTs and 4 case series36 (Table 5). A RCT comparing the effect of tacrolimus 0.1% vs CsA 2%37 showed that both drugs were effective in treating VKC without signifi‐ cant differences between the two. In a second RCT, CsA‐resistant VKC patients,38 treated with tacrolimus 0.1%, showed a signifi‐ cant improvement in clinical scores over CsA 1%. A recent trial comparing the effect of 0.1% topical tacrolimus alone or in com‐ bination with topical corticosteroids in refractory allergic ocular diseases also showed a potential steroid‐sparing effect.39 In addi‐ tion, tacrolimus skin ointments 0.03% or 0.1% have been shown to be beneficial in the treatment of lid eczema in AKC patients.40‐42 Tolerability of topical calcineurin inhibitors is a concern as burn‐ ing sensation is frequently reported. Infections with molluscum contagiosum, papilloma virus, and herpes are infrequent but are recognized risks. A systemic immunosuppressive treatment may be prescribed in most refractory cases of AKC threatening vision. Cyclosporine is the most frequently used drug.43 Tacrolimus and mycophenolate mofetil are alternative options. Recommendations • CsA eye drops are not recommended for SAC and PAC (TF expert opinion)↑↑ • CsA eye drops may be used as a steroid‐sparing agent in steroid‐ dependent cases of VKC or AKC ⨁⨁◯◯ ↑↑ • Tacrolimus off‐label eye drops/ointment should be reserved for use in severe VKC and AKC cases refractory to CsA ⨁◯◯◯↑?
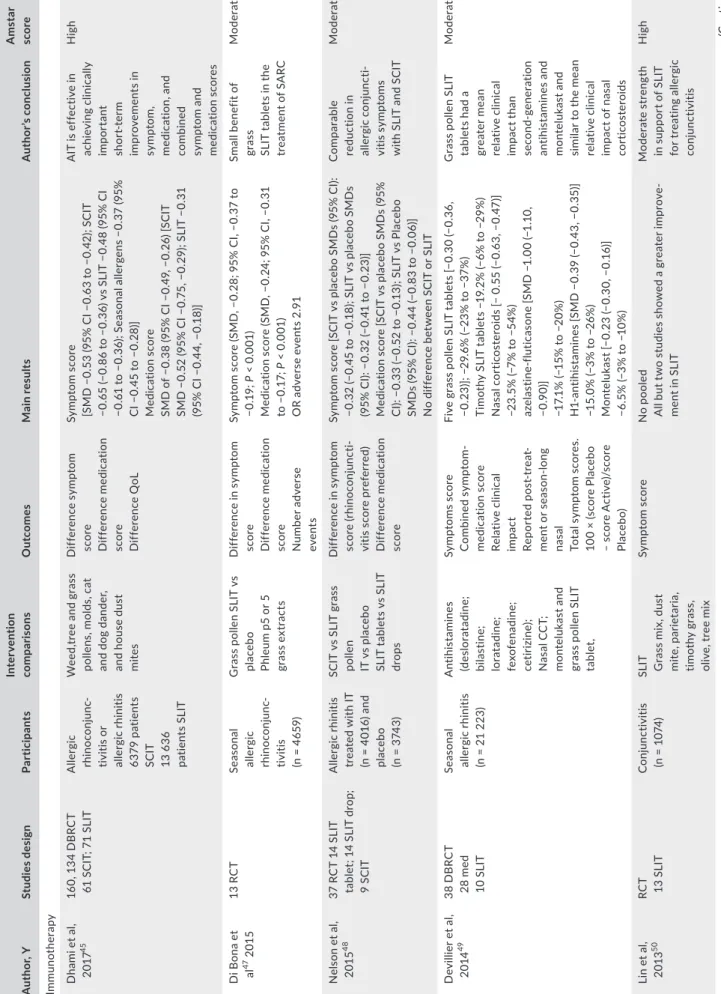
3.1.7 | Allergen‐specific immunotherapy
Since in most patients OA is associated with AR, criteria for al‐ lergen immunotherapy (AIT) should follow the recommendations given by the EAACI guidelines.44 AIT should be consider only when IgE‐mediated allergy is evidenced and when all of follow‐ ing criteria are met the following: moderate‐to‐severe symptoms strongly suggestive of ARC, which interfere with usual daily ac‐ tivities or sleep despite regular and appropriate pharmacotherapy and/or avoidance strategies and evidencing of IgE sensitization (positive SPT and/or serum‐specific IgE) to one or more clinically relevant allergens.44,45 In addition, conjunctival allergen provoca‐ tion test may be helpful in detection of the most relevant allergen before initiating and as a follow‐up tool in assessing response of AIT.2 AIT should also be considered in less severe ARC to take ad‐ vantage of the long‐term benefit on AR and potential prevention of asthma.46 Seven of the 8 selected SR with high and moderate AMSTAR2 scores (Table 6) recommended the use of SLIT and SCIT for moderate improvement of ocular symptoms in the treatment of ARC.45,47‐52 In two recent RCT regarding house dust mite immuno‐ therapy, an improvement was seen in ocular symptoms score.53,54 Only one SR (Table 6) (28 RCT including 1619 children and adoles‐ cents with ARC) showed low evidence of the efficacy of SLIT and SCIT on ocular symptoms.55
Meta‐analysis showed evidence for AIT, with some heteroge‐ neity, in both adults and children, with both SLIT and SCIT,52 drop and tablet formulations, in perennial and seasonal allergies, in pre/ co‐seasonal therapy, and with continuous therapy and in various formulations. Concerns were focused on standardization of allergen extracts and formulation of SLIT preparations. In cases of isolated allergic conjunctivitis, AIT may be considered. TOSS was evaluated as the primary outcome parameter in 36 studies (1725 SLIT and 1674 placebo)51; TOSS was significantly reduced when compared with placebo, as well as individual ocular symptoms scores (redness, itchy and watery eyes). No significant reduction in ocular eye drops use was observed, whereas the threshold dose for conjunctival immediate allergen sensitivity was increased. Two other SRs focusing on ocular symptoms50 concluded that the evidence was of moderate strength in support of SLIT and low for SCIT for treating allergic con‐ junctivitis. No publication was found assessing impact of AIT in VKC and AKC. Recommendation
• AIT may be considered in cases of failure of first‐line treat‐ ments or to modify the natural course of ocular allergic disease ⨁⨁◯◯↑?
• AIT can only be considered only when IgE‐mediated hypersensi‐ tivity is evidenced ⨁⨁⨁⨁ ↑↑
• Before AIT is recommended, control of symptoms of allergic conjunctivitis and other systemic symptoms to assess suitability should be taken into account. ⨁⨁◯◯↑? • AIT is effective for the treatment of allergic conjunctivitis due to grass pollen (⨁⨁⨁⨁ ↑↑) and house dust mite (⨁⨁⨁◯↑?) • SLIT is effective in reducing total and individual ocular symptom score in subjects with allergic conjunctivitis ⨁⨁⨁⨁ ↑? • There are no studies on AIT in VKC and AKC patients. In these forms, AIT requires case‐to‐case assessment by experts (TF ex‐ pert opinion)↑?
3.1.8 | Biologicals
Omalizumab, a systemic anti‐IgE antibody approved for severe asthma, has been used in refractory VKC and AKC and reported in a few case reports/series.56 Control of the disease was partial or com‐ plete in most patients, but poor response was noted in some with very severe presentation.57
Dupilumab is a promising intervention in the management of atopic dermatitis and asthma; however, dupilumab‐associated ocu‐ lar inflammation leading to cicatricial ectropion has been reported suggesting that this drug may not be ideal for the treatment of AKC with eyelid eczema.58
3.2 | Nonpharmacological management
Patients and caregivers should receive educative support regarding the anticipated duration and prognosis of the OA, and possible com‐ plications from suboptimal control.1 The first line of management is the identification of offending allergens and avoidance measures. Particularly during exacerbations in VKC, to minimize the exposure to nonspecific triggering factors, such as sun, wind, and salty water, patients should use measures such as sunglasses, hats with visors, and swimming goggles. Frequent hand, face, lid hygiene, and eye washing should also be suggested. Cold compresses may provide decongestant effect. Tear substitutes aid in stabilization of the tear film providing a better mucosal barrier against allergens, acting as an eyewash and diluting the concentration of mediators in the tear film in contact with the ocular surface. Products with herbal extracts such as chamomile‐containing eye drops should be avoided as they may cross‐react with allergens (for example, Artemisia vulgaris).59Psychological support may be necessary in severe cases of VKC and AKC. The psychodynamic research on OA is currently poor. For patients with AKC and VKC, a collaborative approach between the family doctor, the medical specialist, the psycholo‐ gist, and occupational therapists should be considered.60 There are reports of impact on QoL in different types of OA. There is a dearth of reported interventions of mitigation of psychological impact of the disease.3
3.3 | Management in specific populations
3.3.1 | Pregnancy
Few reports are available in literature concerning the management of OA in pregnant or lactating women. Careful evaluation of aller‐ gic status and need of drug administration is warranted. Allergen
avoidance and environmental measures are the first step, before mast cells stabilizers eye drops can be used. Topical antihistamines or double‐acting drugs can be safely tried. As yet there is no evi‐ dence of severe adverse events with their use, although US‐FDA has assigned many of them to the C category (use with caution if benefits outweigh risks). Short courses of topical corticoster‐ oids if required are cautiously permitted. Vasoconstrictors and decongestants are generally avoided during pregnancy. The use of systemic medications should be minimized if possible. Pregnant (especially in the first trimester) and lactating women can receive
second‐generation oral antihistamine treatment (no teratogenic effects have been described), and low concentrations of these drugs are secreted in breast milk.61,62 Immunotherapy may be continued but not initiated in pregnancy.63