within the fibrous capsule, a part of the fibrous capsule was thought to have become calcified like a ring (Fig 3).
Comment
Calcification is sometimes found in thymomas on CT. In particular, calcification is found in more than half of type B2 and type B3 thymomas[1]. Calcification is found more frequently in invasive thymomas than in noninvasive thymomas[2].
The pattern of calcification in thymomas is usually stippled or nodular[2]. A ring-shaped calcification is very rare, with only 3 cases reported to date.
Harris and colleagues[3]reported a type B2 thymoma with a calcified rim that was excised and classified as modified Masaoka stage IIa. They presented the CT and positron emission tomography findings. Tumor with a standard uptake value of 3.9 on positron emission tomography was found outside the calcified ring. Although they presented the pathologic findings, calcification in the specimen was not described. Low and associates [4] presented the chest roentgenographic and CT images of a thymoma with ring calcification. Their patient did not have invasion beyond the ring calcification on CT.
Siraj and coworkers [5] presented a case of invasive type B3 thymoma contained within the ring calcification. Although the calcification was ring shaped, the calcification was within the tumor, not on its rim.
In our case, the ring calcification was located on the edge of the tumor, and microscopically, the calcified layer was within thefibrous capsule layer. A part of the fibrous capsule was thought to have become calcified like a ring. Based on previous reports and our case, ring calcifica-tion is found in type B2 or type B3 thymoma such as other patterns of calcification. The ring calcification is some-times located within the thymoma and somesome-times in the fibrous capsule. The pathologic and clinical significance of ring calcification in thymoma remains unknown because it is very rare. More cases need to be reported in the literature.
References
1. Tomiyama N, Johkoh T, Mihara N, et al. Using the World Health Organization classification of thymic epithelial neo-plasms to describe CT findings. AJR Am J Roentgenol 2002;179:881–6.
2. Jung K, Lee K, Han J, Kim J, Kim T, Kim E. Malignant thymic epithelial tumors: CT-pathologic correlation. AJR Am J Roentgenol 2001;176:433–9.
3. Harris K, Elsayegh D, Azab B, Alkaied H, Chalhoub M. Thy-moma calcification: is it clinically meaningful? World J Surg Oncol 2011;9:95.
4. Low A, Abbas A, Medford ARL. A ring calcified benign thy-moma in a patient with asbestos exposure. QJM 2013;106: 371–2.
5. Siraj F, Dhawan S, Jain D. Invasive thymoma with osseous metaplasia and cystic change in a case of myasthenia gravis: a rare presentation. Gen Thorac Cardiovasc Surg 2011;59: 583–6.
Surgical Correction of a Fistula
Between Left Pulmonary Artery
and Innominate Vein
Tevfik Kaplan, MD, Gokce Kaan Atac, MD, Perihan Ekmekci, MD, Emel Ozturk, MD, and Serdar Han, MD
Departments of Thoracic Surgery, Radiology, Anesthesiology, and Nuclear Medicine, Ufuk University School of Medicine, Ankara, Turkey
A 48-year-old woman with chronic dyspnea complaints was referred to the thoracic surgery clinic for a surgical lung biopsy to make a definitive diagnosis of interstitial lung disease. Thoracic computed tomography imaging revealed a vascular structure located anterior to the aorta, between the left innominate vein and the pulmonary artery. Magnetic resonance angiography showed the abnormal vessel connection in detail. Pulmonary perfu-sion scintigraphy showed decreased perfuperfu-sion of the left upper lobe and the superior lingular segment. A fistu-lectomy was performed through a mini thoracotomy. The patient no longer had any dyspnea symptoms after the operation.
(Ann Thorac Surg 2014;98:2204–6) Ó 2014 by The Society of Thoracic Surgeons
A
pulmonary arteriovenous fistula is a malformation characterized by abnormal vascular communication between main mediastinal arteries and veins [1]. Mediastinal involvement by such fistulas is rare, and a connection to systemic veins has been reported before in only one case [2]. In this case report, a patient with a fistula between the left pulmonary artery and the innominate vein was presented, and the cross-sectional imaging findings including pulmonary perfusion scin-tigraphy were described. The patient was treated suc-cessfully with mini thoracotomy.A 48-year-old woman with chronic dyspnea and sus-pected interstitial lung disease was referred to our clinic for a surgical lung biopsy to make a final diagnosis. There were no significant medical problems or con-genital malformations in the patient’s family history. She had no symptoms of heart failure. Her blood pres-sure was 110/75 mm Hg, and her pulse rate was 75 beats/min. Physical examination revealed no significant findings except a grade 2/6 continuous machinery murmur, which was heard over the left third intercostal space along the left sternal border during cardiac auscultation.
Accepted for publication Jan 14, 2014.
Address correspondence to Dr Kaplan, Department of Thoracic Surgery, Ufuk University School of Medicine, Dr Ridvan Ege Training and Research Hospital, Mevlana Bulvarı (Konya Yolu) No:86-88, 06520 Balgat, Ankara, Turkey; e-mail:tevfikkaplan@yahoo.com.
Ó 2014 by The Society of Thoracic Surgeons 0003-4975/$36.00
Published by Elsevier http://dx.doi.org/10.1016/j.athoracsur.2014.01.070
2204 CASE REPORT KAPLAN ET AL Ann Thorac Surg
PULMONARY ARTERIOVENOUS FISTULA 2014;98:2204–6
FEATURE
ARTICLE
S
Downloaded for Anonymous User (n/a) at Ufuk Universitesi from ClinicalKey.com by Elsevier on August 01, 2018. For personal use only. No other uses without permission. Copyright ©2018. Elsevier Inc. All rights reserved.
Laboratory findings were within normal limits, and electrocardiographic evaluation revealed no pathologic findings. Left ventricular size and function were normal during echocardiographic evaluation. Right cardiac chambers were slightly dilated, and pulmonary artery pressure was 40 mm Hg. There was no abnormal intra-cardiac left to right shunting.
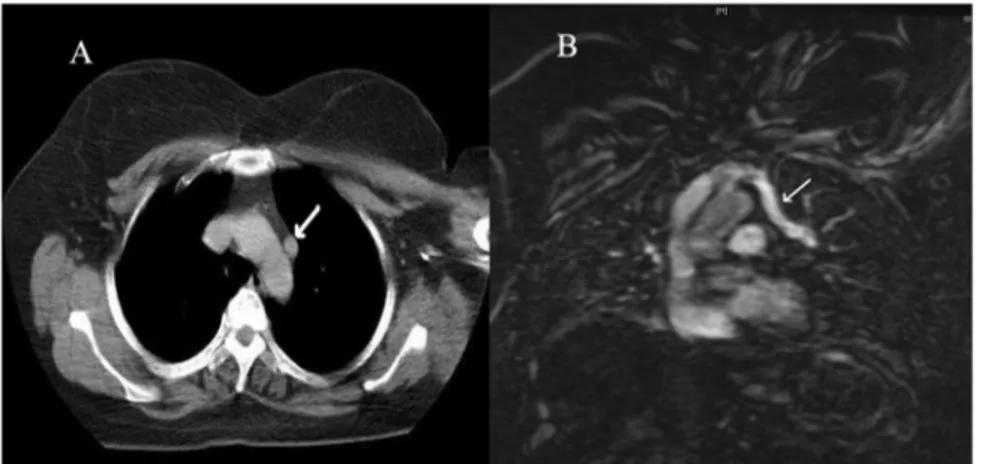
The posteroanterior chest radiograph was normal. A multidetector computed tomography (CT) scan of the thorax was performed using intravenous nonionic iodinated contrast medium. The consecutive sections of the scan showed a circular tubular lesion anterior to the descending aorta starting from the left pulmonary hilum to the innominate vein. Density of the lesion was similar to the aortic content (Fig 1A). The image indicated a vascular connection between the left pulmonary artery and innominate vein. The patient was examined with a 1.5-T magnetic resonance imaging (MRI) vascular communication between the left pulmonary artery and the innominate vein, shown (Fig 1B) by axial T2-weighted and MRI angiography sequences in detail. Three-dimensional reconstruction from multiple images was
also created (Fig 2A). Thefistula was 11 mm in diameter and 6 cm in length. No other cardiac or vascular abnormality was detected. Hypoperfusion on the left upper lobe and lingula superior segment was discovered by pulmonary perfusion scintigraphy study in the nuclear medicine department (Fig 2B). No other invasive pulmonary or cardiac imaging study was performed.
A decision to close this vascular connection between pulmonary and systemic venous circuits with video-assisted thoracoscopy was made after obtaining informed consent from the patient. Because of an un-successful attempt at single-lung ventilation during anesthesia initiation, we performed a mini thoracotomy. The fistula between the left pulmonary artery and innominate vein was sutured. A wedge resection of the left lung was performed during the same session to exclude the diagnosis of interstitial lung disease, even if the pulmonary CT images were inconclusive. The final information gathered from pathologic examination of the lung biopsy was nonspecific inflammation of alveolar structures. The patient had no symptoms of dyspnea
Fig 1. (A) Computed tomography section through upper chest reveals tubular structure showing similar density with aortic arch lumen (white arrow). (B) Coronal MRI angiographic section through the hilum shows the aberrant vessel (white arrow) originating from left pulmonary artery extending to the top of the aortic curve and joining superior innominate vein.
Fig 2. (A) Anteroposterior volume rendering view of hearth and pulmonary vessels reconstructed from MRI angiography. Time-resolved imaging of contrast kinetics (TRICKS) images shows the complete rela-tionship of an aberrant vessel (white arrow) to the pulmonary artery and innominate vein. (B) Pulmonary perfusion scintigraphy shows hypoperfusion on the left upper lobe and lingula superior segment (white arrows).
2205
Ann Thorac Surg CASE REPORT KAPLAN ET AL
2014;98:2204–6 PULMONARY ARTERIOVENOUS FISTULA
FEATUR
E
AR
TICLES
Downloaded for Anonymous User (n/a) at Ufuk Universitesi from ClinicalKey.com by Elsevier on August 01, 2018. For personal use only. No other uses without permission. Copyright ©2018. Elsevier Inc. All rights reserved.
after the surgery. Postsurgical control echocardiogram revealed that pulmonary artery pressure was decreased to 30 mm Hg. The postoperative period of the patient was uneventful, and she was discharged on the seventh postoperative day. The patient’s latest follow-up visit was 6 months after the operation, and no signs or symptoms were found.
Comment
A fistula between the systemic artery or vein and the pulmonary vessel is rare abnormal communication. A small number of cases were described in the literature before. They are usually congenital, but can be iatrogenic or traumatic or occur because of tumors or inflammatory diseases [3]. As our patient had no previous history of trauma, tumor or placement of a central venous catheter, this case was considered congenital.
The feeding arteries of a fistula can originate from abnormal aortic branches or subclavian, axillary, dia-phragmatic, mediastinal, or coronary arteries. Outflow of afistula can be through the pulmonary artery, pulmonary vein, or both [4]. As stated earlier, this type of communication between the pulmonary artery and innominate vein is rare. According to the literature search performed during the preparation of this manuscript, only one similar case was reported[2].
The possibility of enlargement of the untreatedfistula leading to high-output congestive heart failure and presenting with acute pulmonary symptoms owing to increased preload must be kept in mind in the man-agement of the fistula [5, 6]. Treatment options should include surgical ligation and intravascular coil emboli-zation with interventional techniques. In this case, the fistula between the left pulmonary artery and innominate vein was causing dyspnea, pulmonary hypertension, and mild right heart dilatation secondary to a shortcut be-tween cardiac chambers creating volume overload.
CT images should be investigated carefully, because preaortic round lesions can be confused with lymph nodes, which can lead to misdiagnosis, as occurred in our case during an earlier CT evaluation by another radiolo-gist. The continuity of this tubular structure in the consecutive images of the scan directs the physician to diagnosis. Axial images of the chest with MRI may show similarfindings, but consecutively repeated angiographic sequences help to reconstruct the three-dimensional im-ages. Moreover, coronal images of the chest may reveal the abnormal vascular communication. MRI angiography is as helpful as CT, but with the benefit of non-ionizing radiation[5].
Interstitial lung disease was suspected clinically and could not be ruled out as an etiology of the patient’s symptoms. Even if imaging studies were revealed the nature of anatomic and functional details of anomalous vascular structure connecting the pulmonary artery with innominate vein, the expectation of an alternative diag-nosis directed us to perform a lung biopsy in addition to surgical ligation.
In conclusion, mediastinal arteriovenous fistula is a rare, congenital malformation of high variability. In this report, we describe an adult patient with chronic dyspnea owing to afistula from the left pulmonary artery to the innominate vein. She recovered completely from her symptoms after the surgical ligation.
References
1. Iqbal M, Rossoff LJ, Steinberg HN, Marzouk KA, Siegel DN. Pulmonary arteriovenous malformations: a clinical review. Postgrad Med J 2000;76:390–4.
2. Aydogdu S, Ozdemir M, Diker E, Korkmaz S, K€ut€uk E, G€oksel S. Fistulous connection between the left pulmonary artery and the innominate vein. Cathet Cardiovasc Diagn 1996;39:80–1.
3. Hadjimiltiades S, Antonitsis P, Kaitzis D, Klimatsidas M, Mantelas M, Moros I. Endovascular repair of a left axillary-left pulmonary arteryfistula: report of a case. Surg Today 2007;37: 980–3.
4. Riehl G, Chaffanjon P, Frey G, Sessa C, Brichon PY. Post-operative systemic artery to pulmonary vesselfistula: analysis of three cases. Ann Thorac Surg 2003;76:1873–7.
5. Prasad SK, Soukias N, Hornung T, et al. Role of magnetic resonance angiography in the diagnosis of major aortopulmo-nary collateral arteries and partial anomalous pulmoaortopulmo-nary venous drainage. Circulation 2004;109:207–14.
6. Sears E, Aliotta JM, Klinger JR. Partial anomalous pulmonary venous return presenting with adult-onset pulmonary hypertension. Pulm Circ 2012;2:250–5.
An Unexpected Complication of
Titanium Rib Clips
Tevfik Kaplan, MD, Gultekin Gulbahar, MD,
Ahmet Gokhan Gundogdu, MD, and Serdar Han, MD
Department of Thoracic Surgery, Ufuk University School of Medicine; and Department of Thoracic Surgery, Sincan Nafiz Korez State Hospital, Ankara, Turkey
Surgical stabilization of the rib fractures has been suc-cessfully performed for the management of pain in multiple rib fractures, fixation of chronically painful nonunion, reduction of overriding ribs, and flail chest cases. Herein we report a patient who was treated with titanium rib clips after a motor vehicle accident leading to pulmonary parenchymal laceration and multiple painful rib fractures. Three of the rib clips were broken 4 months after the operation. The patient underwent the second operation for restabilization of the broken ribs. We re-view the relevant literature, with particular emphasis on the management of this complication.
(Ann Thorac Surg 2014;98:2206–9) Ó 2014 by The Society of Thoracic Surgeons
Accepted for publication Feb 4, 2014.
Address correspondence to Dr Kaplan, Department of Thoracic Surgery, Ufuk University School of Medicine, Dr Ridvan Ege Teaching and Research Hospital, Mevlana Bulvarı (Konya Yolu) No: 86-88, 06520 Balgat, Ankara, Turkey; e-mail:tevfikkaplan@yahoo.com.
Ó 2014 by The Society of Thoracic Surgeons 0003-4975/$36.00
Published by Elsevier http://dx.doi.org/10.1016/j.athoracsur.2014.02.054
2206 CASE REPORT KAPLAN ET AL Ann Thorac Surg
FRACTURE OF TITANIUM RIB CLIPS 2014;98:2206–9
FEATURE
ARTICLE
S
Downloaded for Anonymous User (n/a) at Ufuk Universitesi from ClinicalKey.com by Elsevier on August 01, 2018. For personal use only. No other uses without permission. Copyright ©2018. Elsevier Inc. All rights reserved.