www.bjorl.org
Brazilian
Journal
of
OTORHINOLARYNGOLOGY
ORIGINAL
ARTICLE
Cervical
paragangliomas:
experience
of
114
cases
in
14
years
夽
Halil
Basel
a,∗,
Nazim
Bozan
baLokmanHekimUniversityFacultyofMedicine,DepartmentofCardiovascularSurgery,Ankara,Turkey bYuzuncuYilUniversityFacultyofMedicine,DepartmentofOtorhinolaryngology,Van,Turkey
Received15January2018;accepted1May2018
KEYWORDS Angiographic embolization; Carotidbifurcation; Cervical paragangliomas; Shamblin classification Abstract
Introductionandobjective:Toreportasinglecenterexperiencewithcarotidbody paragan-glioma cases that were treated by the same surgeon in a city with high prevalence of paragangliomasduetohighaltitude.
Methods:Weretrospectivelyinvestigatedthedemographic,clinicopathologicaland radiologi-caldataof104patientsdiagnosedwithcervicalparagangliomasbetween2003and2017.The patientswereclassifiedaccordingtotheShamblinclassification.
Results:In this study atotal of104 patients (33male and71 female, witha meanage of 54.6±13years)diagnosedwithcervicalparagangliomaslocatedoncarotidbifurcationbetween 2003and2017wereincluded.Amongthosepatients,10presentedwithbilateraltumorsandin total,114paragangliomasweremanagedinthisperiod.Themeandiameterofthetumorswas 5.12±1.45cm.Malignanttumorwasdeterminedinonlyone(0.9%)patient.Allpatientswere operated.In12patientswiththetumordiameterlargerthan5cm,preoperativecoil emboliza-tionwasachieved.In14patients,preoperativeangiographicembolizationwasemployedand in4patientsintraoperativesclerosingagentinjectionswereperformed.Facialparalysiswas observedin2patientsanddysphagiawaspresentin1patient,Hornersyndromewasseenin 1patientandhoarsenesswasreportedin7patientsafteroperation. Allthosecomplications improvedduringfollow-up.Mortalitywasnotreportedinanycases.
Conclusion: Surgery is the definitive treatment for patients with cervical paragangliomas. Although, itmay bedifficultinpatients withthe advancedShamblintypes,inexperienced hands,complicationratesareverylow.
© 2018 Publishedby Elsevier Editora Ltda. onbehalf of Associação Brasileira de Otorrino-laringologiaeCirurgiaCérvico-Facial.ThisisanopenaccessarticleundertheCCBYlicense (http://creativecommons.org/licenses/by/4.0/).
夽 Pleasecitethisarticleas:BaselH,BozanN.Cervicalparagangliomas:experienceof114casesin14years.BrazJOtorhinolaryngol.2018. https://doi.org/10.1016/j.bjorl.2018.05.001
∗Correspondingauthor.
E-mail:hbasel@mynet.com(H.Basel).
PeerReviewundertheresponsibilityofAssociac¸ãoBrasileirade OtorrinolaringologiaeCirurgiaCérvico-Facial.
https://doi.org/10.1016/j.bjorl.2018.05.001
1808-8694/©2018PublishedbyElsevierEditoraLtda.onbehalfofAssociaçãoBrasileiradeOtorrinolaringologiaeCirurgiaCérvico-Facial. ThisisanopenaccessarticleundertheCCBYlicense(http://creativecommons.org/licenses/by/4.0/).
Embolizac¸ão angiográfica;
Bifurcac¸ãocarotídea; Paragangliomas cervicais; Classificac¸ãode Shamblin
Resumo
Introduc¸ãoeobjetivo: Relatarumexperimentoemúnicocentrodecasosdeparagangliomado corpocarotídeoqueforamtratadospelomesmocirurgiãoemumacidadecomaltaprevalência deparagangliomasdevidoàaltaaltitude.
Método: Foraminvestigadosretrospectivamente,osdadosdemográficos,clinico-patológicose radiológicosde104pacientescomdiagnósticodeparagangliomascervicaisentre2003e2017. Ospacientesforamclassificadosdeacordocomaclassificac¸ãodeShamblin.
Resultados: Nesteestudo,foramincluídos104pacientes(33homense71mulheres,commédia deidadede54,6±13anos)comdiagnósticodeparagangliomacervicallocalizadonabifurcac¸ão carotídeaentre2003e2017.Entreessespacientes,10tinhamtumoresbilateraise,nototal, 114paragangliomasforamtratadosnesseperíodo.Odiâmetromédiodostumoresfoide5,12± 1,45cm.Umtumormalignofoideterminadoemapenasum(0,9%)paciente.Todosospacientes foramoperados.Em12pacientescomdiâmetrodotumormaiorque5cm,foipossívelrealizar embolizac¸ãopré-operatóriacommolas;em14pacientes,foirealizadaembolizac¸ãoangiográfica eem4pacientes,injec¸ões deagentesesclerosantes.Apósotratamentocirúrgico, paralisia facialfoiobservadoem2pacientes,disfagiaem1paciente,síndromedeHornerem1paciente erouquidãoem7pacientes.Todasessascomplicac¸õesmelhoraramduranteoacompanhamento. Nãofoirelatadamortalidadeemnenhumcaso.
Conclusão:Acirurgia éotratamentodefinitivoempacientescomparagangliomas cervicais. Emborapossaserdifícilempacientescomostiposavanc¸adosdeShamblin,emmãos experi-entes,astaxasdecomplicac¸õessãomuitobaixas.
©2018Publicado porElsevier EditoraLtda. emnome daAssociaçãoBrasileira de Otorrino-laringologiaeCirurgiaCérvico-Facial. Esteéumartigo OpenAccess sobalicençadeCC BY (http://creativecommons.org/licenses/by/4.0/).
Introduction
Paragangliomas are rare, highly vascular neuro-endocrine
tumors originating from neural crest cells that can be
located anywhere from skullbase to the sacrum.1 About
one-thirdofparagangliomasarehereditary;afewofthem
accompanying familial tumors suchas multiple endocrine
neoplasiaType2(MEN2),vonHippel-Lindau(vHL)diseaseor
neurofibromatosistype.2Metastasis,definedasthespread
of tumor tothe sites where chromaffintissue is normally
absent,suchaslymphnodes,liver,bone,andlungshasbeen
reportedinless than5% ofcarotidbodyparagangliomas.3
Duetothe slowprogressionof thedisease, malignancyis
notalwaysassociatedwithapoorshort-termprognosis.
About2/3ofparagangliomasarelocatedintheadrenal
gland and remaining extra-adrenal tumors were reported
inthe abdomen, thorax,andrarely inthe head andneck
region.4 Head and neck paragangliomas generally grow
slowlyandmayremainsilentforyears.5Themostcommon
head and neck paragangliomas arecarotid body tumors.6
About70---80%ofheadandneckparagangliomasare
asymp-tomaticanddependingonthelocation,theymaymanifest
differentfindingsandsymptoms, suchaspainlesscervical
mass, cranial nerve paralysis, dysphagia and hoarseness,
pulsatiletinnitusandhearingloss,ordifficultiesinspeech,
swallowing, and airway function.7 Carotid tumors grow
slowly. Although they are benign in general, they cause
symptoms due to compression on neighboring vascular or
neuralstructures.Forthatreason,theirsurgicalexploration
isrequired.Ifsurgicallycompleteexplorationisnotpossible
duetothefactorsassociatedwiththepatientortumor
local-ization,radiotherapyshouldbeconsidered.Althoughcarotid
tumorsareradiosensitive,totalresolutionwithradiotherapy
israre.Ingeneral,withradiotherapy,tumorstabilizationor
partialregressionisthegoal.8
Inthisstudy,wewillreport asinglecenterexperience
of114 cervicalparagangliomacasesin 14yearsthatwere
treatedbythesamesurgeoninacitywithhighprevalence
ofparagangliomasduetohighaltitude.
Materials
and
methods
We retrospectively investigated the demographic,
clinic-pathologicalandradiologicaldataof104patientsdiagnosed
with and operated for cervical paragangliomas between
2003 and 2017 in Van Trainingand Research Hospital and
Van Lokman Hekim Private Hospital. Postoperative results
andoperativecomplicationswerealsorecorded.
Thepatients wereclassified according totheShamblin
classification.9 Only patients operated for cervical
para-gangliomas were included in the study. In preoperative
imagingofthecases,coloredDopplerultrasoundand
mag-netic resonanceimagingwere performed.In patientswho
hadembolization,carotidangiographywasalsoperformed.
In all patients with a tumor larger than 5cm and with
high vascularity, preoperative angiographic embolization
was performed (Fig. 1). The patients were operated the
day after angiographicembolization ifit wasrequired. In
patientswithlargeamountsofbleedingduringoperations,
intraoperative coils were inserted. In all patients with a
tumor largerthan5cm, divisionof internal carotidartery
was performed and end-to-endanastomosis wasachieved
afterremoval(Figs.2and3).InpatientswithShamblinIII
tumors,ifrequired,thearterywasexcisedandaPTFEgraft
orsaphenousgraftinter-positioned.Ifagraftwasrequired
Figure1 (A)Angiographybeforecoilembolization.(B)Angiographyaftercoilembolization.
Figure2 (A)Intraoperativecoilembolization.(B)ShamblinTypeIIIpatient---Carotidinvasion.(C)Divisionofexternalcarotid artery.(D)Re-anastomosisofdivisionofexternalcarotidartery.
Figure3 Macroscopicappearanceofthetumor.
wasstartedfor6months.Inpatients withapositive
fam-ily history, annual controls were performed with Doppler
ultrasoundandmagneticresonanceimaging.
Statisticalanalysis
The datawere analyzedusing SPSS21. Descriptive
statis-ticswereperformed.Numericalvariableswereexpressedas
mean±standard deviation,andcategoricalvariableswere
analyzedasfrequencyandpercentage.p<0.05was
consid-eredstatisticallysignificant.
Results
In this study,a total of 104 patients diagnosed with
cer-vical paragangliomas located on the carotid bifurcation,
treated between 2003 and 2017, were included. Among
thosepatients, 10 presented with bilateral tumors and a
totalof114 paragangliomasweremanaged inthis period.
Themeanfollow-upperiodwas54±30months(range:1---96
months).Amongthosepatients,33weremaleand71were
femalewitha meanage of 54.6±13years (range:18---83
years).Themeanageofmaleswas56.4±12yearsandthe
meanageoffemaleswas53.1±13years;therewasnotany
statisticallysignificantdifferencebetweengenders
regard-ingthemeanageatthediagnosis(p>0.05).In10(3male,
7female)ofthepatients,paragangliomaswerebilateral.In
bothgenders, inabout 9---10% ofthe patients,thetumors
werebilateral.Familyhistorywaspresentin2(2/10)ofthe
patientswithbilateraltumors.
Thedimensionsofthetumorsrangedbetween1.3cmand
10.6cmwithameandiameterof5.12±1.45cm.Malignant
In15(19.9%)patients,therewasafamilyhistoryfor
para-gangliomas.Inallpatients,themainfindingwasamassin
thecervicalregion.Thepatientsweregroupedaccordingto
theShamblinclassificationandregardingthisclassification;
15(13.2%)wereShamblinTypeI,66(57.9%)wereShamblin
TypeII,and33(28.9%)wereShamblinTypeIII.
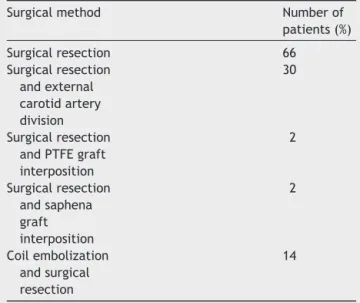
Surgicalmethodsappliedtothepatientsaresummarized
inTable 1. In12 patients withthetumor diameter larger
than5cm,preoperativecoilembolizationwasachieved.In
14patients,preoperativeangiographicembolizationandin4
patientsintraoperativesclerosingagentinjectionswere
per-formed.In30patients,divisionoftheexternalcarotidartery
wasperformedanditwasre-anastomosedaftertheremoval
ofthemass.In4patientswithShamblinIIItumors,internal
andexternalcarotidarterieswereexcisedandrepairedwith
PTFEandsaphenousveingraft.
Thecomplicationsafteroperationswerealsorecorded.
Facialparalysiswasapparentin2(1.9%)patients,
dyspha-giaoccurredin1(0.9%)patient,Horner’ssyndromewasseen
in1(0.9%)patientandhoarsenesswasreportedin7(6.7%)
patients:thosewerenotpersistentinanyofthecases.All
those complications improved during follow-up. Mortality
wasnotreportedinanycases.
Discussion
Inthisstudy,wereportedthegeneralcharacteristicsof104
patientswithcervicalparagangliomaslocatedonthecarotid
bifurcation.Tothebestofourknowledge,thisisoneofthe
largest seriesin the literature reportingthe outcomes of
cervicalparagangliomas.
Femaletomaleratiowas2.15inthisstudy.Afemale
pre-dominancewasalsoreportedpreviouslyinsomestudies.10
However,inaretrospectivestudyon10patients,Darouassi
etal.11 reporteda malepredominance withasex-ratioof
2.33.Aslowgrowing,painlessmasswasthemostcommon
clinical presentation in our study asreported before.11---13
Luna-Ortizetal.14 alsoreportedtheir20yearsexperience
on69 carotid body tumorsand determined that 96.9% of
thepatientswerefemaleandthemostcommon
presenta-tionwasalsoapainlessneckmassdeterminedin78.7%of
Table1 Surgicalmethodsappliedtothepatients. Surgicalmethod Numberof
patients(%) Surgicalresection 66 Surgicalresection andexternal carotidartery division 30 Surgicalresection andPTFEgraft interposition 2 Surgicalresection andsaphena graft interposition 2 Coilembolization andsurgical resection 14
mayalsobethemaincomplaintsatdiagnosis.
In preoperative diagnosis, imaging is crucial since the differential diagnosis includes thyroid nodules, lym-phadenopathy and brachial cysts. Fine-needle aspiration biopsyisnotemployedsinceithasahighcomplicationrisk due to the hyper-vascularization of the tumor and more-overthecytologicalevaluationcannotdifferentiatebenign from malignant lesions. In this study, all patients were diagnosedwiththeimagingtechniquesandfine-needle aspi-rationbiopsywasnotperformedinanypatients.
Theincidenceoffamilialcarotidbifurcationtumorswas reportedas 20% inprevious studies.15,16 In this study,the
ratiooffamilialcaseswas19.9%,whichwascompatiblewith
theliterature.
Mediounietal.17 analyzedthegeneralcharacteristicsof
131benignparagangliomasandcomparedthemto11
malig-nantparagangliomascases.Theyreportedthat;thebenign
paragangliomasweremostlyobservedinwomenwithamean
ageof 45yearsat timeof diagnosis.In thatstudy
tympa-nojugular sites were the most common sites followed by
carotidandvagal sites. Onthe otherhand, themalignant
tumorsweremainlyobservedinyoungerpatientsandthey
werepredominantlycarotidtumors.Inourstudy,therewas
onlyonemalignantparagangliomainafemalepatient
diag-nosedat theage of65 years.Inthis case,the tumorwas
unilateral.
With the development of safe embolization protocols,
surgical resection has become the preferred treatment
option in cervical paragangliomas.15 However, due to
its localization near large vascular structures and
cra-nial nerves, the surgical treatment is challenging. The
surgery shouldbeasconservative aspossible tominimize
the complications.In that aspect,preoperative
emboliza-tion was mainly advised in large and hyper-vascularized
tumors.16 Jianuetal.18 reportedthe treatment outcomes
of 7 patients (5 women, 2 men with a meanage of 54.7
years)diagnosedwithcervicalparagangliomas,whowereall
operatedwithoutanypreoperativeembolization.Theydid
not observeany perioperativecomplications in 6 patients
butin1case,atransientipsilateralvagusnervedeficitwas
reported. There wasno sign of recurrences in 3 years of
follow-upinthatstudy.Chanetal.19analyzedthetreatment
outcomesofpatientswithheadandneckparagangliomasin
a nationwidesurveyand reportedthat 91% ofcases were
treatedwithsurgeryalone,andembolizationalonewas
per-formed in 4% of cases. Postoperative complications were
more common in patients undergoing both embolization
and surgerytogether; while acutemedical complications,
including acute renal failure and pneumonia, were more
likelyreportedinpatientsundergoingembolizationonly.In
ourstudy,although we didnot comparethe patientswho
were treated withor without endovascularinterventions;
wedidnotobserveanassociation.Itshouldalsobekeptin
mindthat, ingeneral embolization isrequired in patients
withlargetumorsanditisnotsurprisingthatlargertumors
wereassociatedwithhighercomplicationrates.
Inaretrospectivestudy,Lamblinetal.20 evaluatedthe
treatment outcomes in 54 carotid body tumor resections
in 49 patients and reported that early (in 1 month after
surgery) complications occurred in 31 cases, including 30
cases of cranial nerve deficit (56%). They also reported
that; 8 patients (17%) showed no cranial nerve deficit
recovery, even after 18 months of follow-up. Dorobisz
etal.21analyzedthemedicaldataof47patientswhowere
diagnosed with and operated for carotid paragangliomas
the tumor was performed, including 11 cases (22%) that
additionally required vascular suturing, and 5 (10%) that
required reconstruction of the internal carotid artery.
Regardingthepostoperativecomplications,3patients(6%)
werere-operatedbecauseofsymptomsofcerebralstroke,
hypoglossalnervepalsywasdeterminedin3cases(6%),and
facial nervepalsy in 2 patients (4%), while postoperative
hematomasinthewoundwasobservedin6patients(12%).
Weobservedfacialparalysisin2(1.9%)patients,dysphagia
in1 (0.9%)patient,Horner’s syndromein1 (0.9%)patient
andhoarsenessin7(6.7%)patients;allthosecomplications
werereversibleinfollow-up.
In this study, in 10 patients, the tumors were
bilat-eral. In bilateral paragangliomas, some risk factors such
asgeneticpredisposition, priornecksurgery or
radiother-apy were defined.22 Family history was present in 2 of
10 patients withbilateral cervical paragangliomas.
Fortu-nately,withthedevelopmentof moreaccuratediagnostic
methods, paragangliomas are diagnosedat earlierstages.
Inourstudy,28.9% ofparagangliomaswereShamblinType
IIIandtherewerenotanyShamblinTypeIVcases.Withan
advancedstage,complicationrisksincludingnerveinjuries
alsoincrease.Inourstudyin7patientsreversible
hoarse-nesswasdeterminedthatwasduetothevagalorhypoglossal
nerveinjury.
Recently,about20---30%ofheadandneckparagangliomas
weredeterminedtobegeneticandassociatedwithgermline
mutations.23 Inespeciallymulticentericor recurrentcases
geneticmutationsshouldbesuspected.However,because
oftheexpense,wedonotroutinelyperformgenetictests
indailypractice.
Conclusion
Inconclusion,surgeryisthedefinitivetreatmentinpatients
withcervicalparagangliomas.Although,itmaybedifficultin
patientswiththeadvancedShamblintypes,inexperienced
hands,complicationratesareverylow.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
References
1.Mendenhall WM, Amdur RJ, Vaysberg M, Mendenhall CM, Werning JW. Head and neck paragangliomas. Head Neck. 2011;33:1530---4.
2.Gimenez-RoqueploAP,DahiaPL,RobledoM.Anupdateonthe geneticsofparaganglioma,pheochromocytoma,andassociated hereditarysyndromes.HormMetabRes.2012;44:328---33. 3.Suárez C,Rodrigo JP, Mendenhall WM, Hamoir M, Silver CE,
GrégoireV,et al.Carotidbodyparagangliomas:a systematic studyonmanagementwithsurgeryandradiotherapy.EurArch Otorhinolaryngol.2014;271:23---34.
4.BurnichonN,CascónA,SchiaviF,MoralesNP,Comino-Méndez I,AbermilN,etal.MAXmutationscausehereditaryand spo-radicpheochromocytomaandparaganglioma.ClinCancerRes. 2012;18:2828---37.
5.JansenJC,vandenBergR,KuiperA,vanderMeyAG, Zwinder-manAH,CornelisseCJ.Headandneckparagangliomasgenerally
grow slowly and may remain silent for years. Estimationof growth rate in patients withhead and neck paragangliomas influencesthetreatmentproposal.Cancer.2000;88:2811---6. 6.Jianu DC,Muresanu DF, PetricaM.Diagnosis ofcarotid body
paragangliomasbyvariousimagingtechniques.RomJNeurol. 2014;7:161---6.
7.Corssmit EP, Romijn JA. Clinical management of paragan-gliomas.EurJEndocrinol.2014;171:231---43.
8.GilboP,Morris CG,AmdurRJ,Werning JW,DziegielewskiPT, KirwanJ,etal.Radiotherapyforbenignheadandneck para-gangliomas:a45-yearexperience.Cancer.2014;120:3738---43. 9.ShamblinWR,ReMineWH,Sheps SG,HarrisonEG Jr.Carotid
body tumor (chemodectoma): clinicopathologic analysis of ninetycases.AmJSurg.1971;122:732---9.
10.Gad A, SayedA, Elwan H, FouadFM, Kamal EldinH, Khairy H, et al.Carotid bodytumors: areview of25years experi-enceindiagnosisandmanagementof56tumors.AnnVascDis. 2014;7:292---9.
11.DarouassiY,AlaouiM,MlihaTouatiM,AlMaghraouiO,En-Nouali A, Bouaity B, et al. Carotid bodytumors: a caseseries and reviewoftheliterature.AnnVascSurg.2017;43:265---70. 12.LeeJH,BarichF,KarnellLH.Nationalcancerdatabasereport
on malignant paragangliomas of head and neck. Cancer. 2002;94:730---7.
13.FerranteAM,BoscarinoG,CreaMA,MinelliF,SniderF.Cervical paragangliomas:singlecentreexperiencewith44cases.Acta OtorhinolaryngolItal.2015;35:88---92.
14.Luna-Ortiz K, Rascon-Ortiz M, Villavicencio-Valencia V, Granados-Garcia M, Herrera-Gomez A. Carotid body tumors: reviewofa20-yearexperience.OralOncol.2005;41:56---61. 15.Ma D, Liu M, Yang H. Diagnosis and surgical treatment of
carotidbodytumor:areportof18cases.JCardiovascDisRes. 2010;1:122---4.
16.QinRF,ShiLF,LiuYP.Diagnosisandsurgicaltreatmentofcarotid bodytumors:25years’experienceinChina.IntJOralMaxillofac Surg.2009;38:713---8.
17.MediouniA,AmmariS,WassefM,Gimenez-RoqueploAP,Laredo JD, Duet M, et al. Malignant head/neck paragangliomas. Comparativestudy.EurAnnOtorhinolaryngolHead NeckDis. 2014;131:159---66.
18.Jianu DC,Jianu SN,MotocAG,DanTF, PoenaruM,T˘abanS, etal.Anevaluationonmultidisciplinarymanagementofcarotid bodyparagangliomas:areportofsevencases.RomJMorphol Embryol.2016;57:853---9.
19.ChanJY,LiRJ,GourinCG.Short-termoutcomesandcostofcare oftreatmentofheadandneckparagangliomas.Laryngoscope. 2013;123:1645---51.
20.LamblinE,AtallahI,ReytE,SchmerberS,MagneJL,Righini CA.Neurovascularcomplicationsfollowingcarotidbody para-gangliomaresection.EurAnnOtorhinolaryngolHeadNeckDis. 2016;133:319---24.
21.Dorobisz K,Dorobisz T,TemporaleH, Zato´nskiT, KubackaM, ChabowskiM,etal.Diagnosticandtherapeuticdifficultiesin carotidbodyparagangliomas,basedonclinicalexperienceand areviewoftheliterature.AdvClinExpMed.2016;25:1173---7. 22.MooreMG,NettervilleJL,MendenhallWM,IsaacsonB,
Nussen-baum B. Head and neck paragangliomas: an update on evaluation and management. Otolaryngol Head Neck Surg. 2016;154:597---605.
23.Kim ES, Kim SY, Mo EY, Jang DK, Moon SD, Han JH. Novel germline SDHDmutationina patientwithrecurrentfamilial carotidbodytumorandconcomitantpheochromocytoma.Head Neck.2014;36:131---5.