www.elsevier.es/ejpsy
ORIGINAL
ARTICLE
Efficacy
of
light
therapy
on
non-seasonal
depression
and
inflammatory
markers
M.E.
Demirkol
a,∗,
Z.
Namlı
b,
L.
Tamam
aaDepartmentofPsychiatry,C¸ukurovaUniversityBalcalıHospital,Sarıc¸am,Adana,Turkey bDepartmentofPsychiatry,MehmetAkifInanGovernmentHospital,S¸anlıurfa,Turkey
Received16July2018;accepted11March2019 Availableonline23March2019
KEYWORDS Lighttherapy; Majordepressive disorder; Inflammatory markers; Neutrophil/lymphocyte ratio; Platelet/lymphocyte ratio;
Meanplateletvolume
Abstract
Backgroundandobjectives: Theevidenceforefficacyoflighttherapyinnon-seasonal depres-sionremainscontroversial.Theprimaryaimofthisstudy wastoinvestigate theefficacyof brightlighttherapywhenitwascombinedwithantidepressanttreatmentinthecourseofmajor depressivedisorderwithoutseasonalpattern.Thesecondaryaimwastoassesstheinflammatory responsetobrightlighttherapy.
Methods:PatientswhohadaHamiltonDepressionscalescoreof17orabove,whowere receiv-ingantidepressantmonotherapyforatleast4weekswereincludedinthestudy(n=74).Patients wereassignedtoeitherantidepressantmonotherapy(n=40)orcombinationofantidepressant andbrightlighttherapy(n=34).Theseverityofthedepressionandsuicidalideationwas eval-uatedbyHamiltonDepressionScaleandTheBeckScaleforsuicideideation.Theeffectoflight therapyoninflammatorymarkerswasinvestigatedbasedontheneutrophil/lymphocyteratio, platelet/lymphocyteratio,plateletcountsandmeanplateletvolume.Theirclinicalstatewas monitoredatthebaseline,1dayand2weeksaftertreatment.
Results:Independentfromtreatmentgroup,patientsshoweddecreaseddepressionandsuicidal ideationscoresaftertreatment.Theresultsofstatisticalanalysisoftime×groupinteractions regardingdepressionandsuicidalideationscoresalsoshowedsignificantdifferencesbetween groupsovertime.Forinflammatorymarkers,onlythelymphocytecountshowedsignificant dif-ferencebetweengroupsovertime.Exceptplatelet/lymphocyteratio,allinflammatorymarkers showedsignificantalterationswithtimeindependentfromtreatmentarm.
Conclusion:Combininglighttherapywithoralantidepressantscanbehelpfulinnon-seasonal depressionaswell.
©2019Asociaci´onUniversitariadeZaragozaparaelProgresodelaPsiquiatr´ıaylaSaludMental. PublishedbyElsevierEspa˜na,S.L.U.Allrightsreserved.
∗Correspondingauthor.
E-mailaddress:emindemirkol@gmail.com(M.E.Demirkol). https://doi.org/10.1016/j.ejpsy.2019.03.002
0213-6163/©2019Asociaci´onUniversitariadeZaragozaparaelProgresodelaPsiquiatr´ıaylaSaludMental.PublishedbyElsevierEspa˜na, S.L.U.Allrightsreserved.
Introduction
Depressionisacommonpsychiatricdisorderaffectingover 300millionpeoplearoundtheworldandbytheyear2010, it is expected to be the second most common cause of disability following thecardiovascular diseases.1,2 Despite
a wide range of treatment options including antidepres-santsand psychotherapy,many patients arestillresistant totreatmentortheydevelopadverseeffectscausing treat-ment interruption.3 Almost half of the patients do not
respondtofirst-linetreatmentsadequately,andafteran 8-weeksofantidepressanttreatment,only35---40%ofpatients experienceremissionofsymptoms.4,5Therefore,alternative
treatment modalitiesarerequired forthemanagementof depressivesymptoms.
Bright light therapy (BLT) is a choice of treatment which is used mostly to treat seasonal affective disor-der (SAD). It comprises exposure to artificial bright light for a given period of time particularly in the mornings.6
Patients with non-seasonal depression also experience symptomsof irregularsleep---wake patterns, diurnal mood swings, altered circadian patterns of hormones and core bodytemperature problems whichcan beassociatedwith circadian abnormalities. These abnormalities provide a rationale for the use of light therapy in non-seasonal depression.7---9
Previousstudieshaveinvestigatedtheclinicalpotential of light therapy in patients with non-seasonal depressive disorders.10---12 However,theresultsfromthesestudiesare
contradictory.Anewmeta-analysisand systematicreview resultedabeneficialeffectoflighttherapyinnon-seasonal depression but the overall quality of the evidence was poor due to high risk of bias and inconsistency.So, more studies are needed in order to address this significant gap.
Thereisincreasingevidencefromstudieswhichsupport the roleof inflammatory responseand immune system in the pathophysiology of mood disorders.13---15 Neutrophil to
lymphocyte ratio (NLR) and platelet to lymphocyte ratio (PLR)aresimple,relativelycheapandreproducible param-eterswhich can easily be obtained fromwhite blood cell essay.16 Arecentmeta-analysisreportedthatpatientswith
major depressivedisorder (MDD) had higher NLR as com-paredtohealthycontrolsandoverallresultssupportedthe hypothesis that NLR and PLR might be useful to detect the inflammatory activation seen in mood disorders.16
The relationship between majordepressionand increased plateletactivityhasalsobeenpreviouslyreportedby sev-eral studies. They found that increased mean platelet volume (MPV) is associated with the diagnosis of major depression.
The primary aim of this study was to investigate the efficacy of BLT when it was combined with antidepres-sant treatment in the management of patients with a current depressive episode in the course of MDD with-out seasonal pattern. The secondary aim was to assess the inflammatory response to BLT in these patients. So, treatment response wasevaluatedwith both clinical out-comes (Hamilton Depression Scale and The Beck Scale forsuicideideation)andinflammatorymarkers (NLR,PLR, MPV).
Patients
and
methods
Patients
This study was approved by C¸ukurova University School ofMedicine (C¸USM) EthicsCommittee. Allpatients signed written informed consent before participation into the study.Patientswererecruitedfromthepsychiatricinpatient clinics of Balcali Hospital, Adana, Turkey between March andOctober 2017. All patients were diagnosed withMDD basedon Diagnostic andStatistical Manual of Mental Dis-orders(DSM)-5diagnosisandclassificationsystem.Patients between18and65yearsofage,whohadaHamilton Depres-sionScale (HDS)scoreof17orabove,whowerereceiving selectiveserotonin reuptake inhibitor (SSRI) or serotonin-norepinephrinereuptakeinhibitor (SNRI) monotherapy for atleast4weekswereincludedinthestudy.86patientswho mettheinclusioncriteriawentonwithaclinicalinterview. Patientswhohadcomorbidpsychiatricdisorders(n=3),or whowereusingantipsychotics or receiving electroconvul-sive therapy (ECT) (n=4) were excluded from the study because the efficacy of light therapy and antidepressant drugs on depression could not be clearly understood in thesepatients.Patientswhohadchronicinflammatory dis-ease (n=2), who had a history of smokingor alcohol use disorder (n=3) were also excluded because of the possi-ble effects of these situations on inflammatory markers. Thus,finalanalysis included74 depressivepatients,40 of whom received antidepressant (AD) monotherapy and 34 patientsreceivedcombinationofAD+BLT.Thepatientswere randomizedaccording totheir admissionorder. Allof the patientscompletedalloftheassessmentsandnodrop-out wasoccurred.
Procedure
Socio-demographicalinformationwascollectedwithaform whichwascreatedbytheinvestigators.Theseverityofthe depressionwasevaluatedbyHDSandsuicidalideationwas evaluatedbyTheBeckScaleforsuicideideation(BSSI).
Bloodsamplesweredrawnfromtheantecubitalveinat 06.30inthemorningafter12hfastingbeforethetreatment. Follow up sampleswere collected withthe same method just one day and two weeks after the light therapy. The effectoflighttherapyoninflammatorymarkerswas inves-tigatedbasedontheneutrophil,lymphocyte,andplatelet counts.NLR,PLRwerecalculatedbyusingthesevalues.The clinicalscalesandlaboratorytestswereperformed before treatment, oneday after treatment and two weeksafter treatment.
BLT was applied in a sitting position at a distance of 40cm fromthe patient and a 60-degree angle for 60min for14dayswithaglanceatthelighteveryminuteusinga lightintensityof10,000lxwithadevicedesignedfor medi-caluse(Klarstein,Model10006251).Treatmentprotocolwas determinedbasedoninstructionsprovidedbythe manufac-turerofthelighttherapy device.Wewokeupallpatients (bothAD+BLTandADmonotherapygroups)at06.30amand thetreatmentwascarriedouteverymorningfrom07:00to 07:30,atleast30minafterpatient’swakeup.
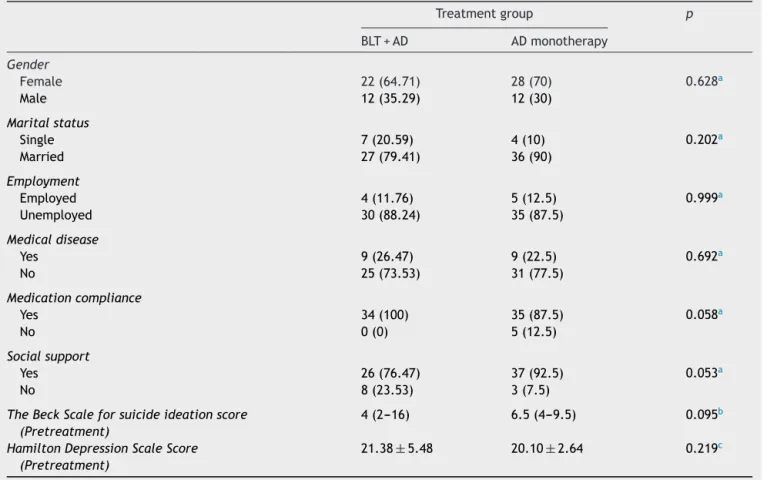
Table1 Socio-demographicalandclinicalcharacteristicsofparticipants. Treatmentgroup p BLT+AD ADmonotherapy Gender Female 22(64.71) 28(70) 0.628a Male 12(35.29) 12(30) Maritalstatus Single 7(20.59) 4(10) 0.202a Married 27(79.41) 36(90) Employment Employed 4(11.76) 5(12.5) 0.999a Unemployed 30(88.24) 35(87.5) Medicaldisease Yes 9(26.47) 9(22.5) 0.692a No 25(73.53) 31(77.5) Medicationcompliance Yes 34(100) 35(87.5) 0.058a No 0(0) 5(12.5) Socialsupport Yes 26(76.47) 37(92.5) 0.053a No 8(23.53) 3(7.5)
TheBeckScaleforsuicideideationscore (Pretreatment)
4(2---16) 6.5(4---9.5) 0.095b
HamiltonDepressionScaleScore (Pretreatment)
21.38±5.48 20.10±2.64 0.219c
aFisherExacttest.Descriptivestatisticspresentedasnumber(percentage). b MannWhitneyUtest.Descriptivestatisticspresentedasmedian(Q1−Q3).
c IndependentSamplest-test.Descriptivestatisticspresentedasmean±standarddeviation.
During the BLT, the patients continued to take their antidepressantswithoutanychangeindosageormedication time.Allthepatientssleptanaverageof7---8h/dayandno sleeprestrictionhasbeenappliedtoavoidanypossible con-foundingsituation.Asallthepatientswerehospitalizedat inpatientpsychiatryclinicsatthetimeofthestudy,wecould strictly controltheir drugadherence and sleepdurations. Nomedicationthathasthepotentialtoalterinflammatory markerlevelswasgiventothepatients.
Statisticalanalysis
74 depressed patients were enrolled to the study. Fis-cher exact test, Mann---Whitney U test and independent samplesofttest areusedinordertocompare the socio-demographicaland clinical characteristics of two groups. The outcome parameters (inflammatory markers and BSSI andHAMD scale) were evaluatedbefore treatment, after treatmentand2weeksaftertreatment.Two-wayrepeated measures of analysis of variance (ANOVA) was used for comparison of time dependent alterations in outcome parametersbetween twogroups. Foroutcome parameters thatviolatedtheANOVAassumptions,anRpackagecalled npaRLDfornon-parametriclongitudinaldatawasusedinthe analysis.Thelimitforstatisticalsignificancewasaccepted
asp<0.05. SPSSStatistics,version23.0 andRversion 3.0 wereusedtoperformtheanalyses.
Results
Thesocio-demographicalandclinicalcharacteristicsoftwo groupsarepresentedinTable1.Therewerenosignificant differences between groups in terms of gender, mari-tal status, employmentstatus, historyof ECT, medication compliance,socialsupportandscoresofHDSandBSSIbefore treatment(p>0.05).
Time dependent alterations in HDS score, BSSI score and serum inflammatory marker levels are presented in Table 2. Independent from treatment group, patients showed decreased HDS and BSSI scores after treatment (p<0.001).Independentfromtreatmentgroup,serumlevels ofinflammatorymarkersalsoshowedsignificantalterations aftertreatment.Neutrophilcountincreasedonedayafter treatment and it decreased significantly 2 weeks after treatment(p=0.003)whereaslymphocytecountincreased gradually(p<0.001);thus,NLRdecreasedasaresultafter treatment(p<0.001).Twoweeksafterthetreatment,MPV was found significantly decreased (p<0.001) among all patients.Independentfromtreatmentgroup,therewasno significantdifferenceinPLRovertime(p>0.05).
Table2 Timedependentalterationsofoutcomeparameterswithtime×groupinteractionresults.
Allpatients p Treatmentgroup p
BLT+AD ADmonotherapy
TheBeckScaleforsuicideideation
Pretreatment 5(3---10) <0.001 4(2---16) 6.5(4---9.5) <0.001a
Aftertreatment 5(1---9) 1(0---5) 6.5(5---9)
2weeksaftertreatment 3.5(0---7) 0(0---4) 5(3---7)
HamiltonDepressionScale
Pretreatment 20.69±4.21 <0.001b 21.38±5.48 20.1±2.64 <0.001b
Aftertreatment 16.69±5.96 13.18±6.69 19.68±2.96
2weeksaftertreatment 15.14±5.33 11.88±5.95 17.9±2.47 Platelet/Lymphocyteratio
Pretreatment 118.61±39.01 0.985b 111.38±27.91 124.75±45.88 0.785b
Aftertreatment 118.16±40.57 109.92±38.62 125.17±41.33
2weeksaftertreatment 117.96±40.82 112.29±42.04 122.78±39.65 Meanplateletvolume
Pretreatment 10.29±0.98 <0.001b 10.4±1.03 10.21±0.94 0.141b
Aftertreatment 9.7±0.72 9.63±0.64 9.76±0.77
2weeksaftertreatment 9.81±0.8 9.88±0.84 9.76±0.77
Neutrophilcount
Pretreatment 5582.7±1931.37 0.003b 5495.29±1653.43 5657±2157.91 0.751b Aftertreatment 5706.46±1865.24 5633.24±1555.18 5768.7±2111.17
2weeksaftertreatment 5069.19±2037.42 5122.35±1886.24 5024±2180.57 Lymphocytecount
Pretreatment 2597.7±760.6 <0.001b 2596.18±675.74 2599±834.56 <0.001b Aftertreatment 2722.84±776.85 2810.88±661.08 2648±864.48
2weeksaftertreatment 2897.57±958.19 3239.71±896.96 2606.75±921.4 Neutrophil/Lymphocyteratio
Pretreatment 2.31±1.05 <0.001b 2.27±0.95 2.35±1.13 0.136b
Aftertreatment 2.25±0.96 2.11±0.75 2.36±1.11
2weeksaftertreatment 1.9±0.9 1.65±0.63 2.11±1.04
a AnRsoftwarepackagenpaRLD(NonparametricAnalysisofLongitudinalDatainFactorialExperiments). b TwowayrepeatedmeasuresANOVA.
The resultsof statisticalanalysisof time×group inter-actions are also presented in Table 2 and in Figs. 1---3. HDSandBSSIscoresshowedsignificantdifferencesbetween groups over time (p<0.001). BLT+AD combined therapy groupshowedmoresignificantdecreasesinbothscores com-paredtoADmonotherapygroup.Forinflammatorymarkers, only the lymphocyte count showed significant difference between groups over time (p<0.001). BLT+AD combined therapygroupshowedgradualincreaseinlymphocytecount overtimewhereasADmonotherapygroupdidnot.
Table3presentsthecorrelationbetweenclinicalscales andinflammatorymarkers. PretreatmentBSSIscores were found positively correlated with mean platelet volume (r=0.375,p<0.001).PretreatmentHDSscoreswerefound negatively correlated with lymphocyte count (r=−0.229, p<0.05).
Discussion
This study aimed to investigate the efficacy and safety
of BLT in non-seasonal MDD. The primary outcome
measurement was HDS score and secondary outcome
measurements were BSSI scores and serum inflammatory markers.As aprimaryoutcome,HDSscoresdecreased sig-nificantly one day after the treatment and continued to decrease two weeks after the treatment in both groups. It means that both AD monotherapy and BLT+AD com-bined therapy groups showed significant improvements in depressionseverityaftertreatment.Thisimprovementwas significantly more prominent in combined therapy group compared to AD monotherapy, indicating that BLT can be a helpful additional therapeutic intervention for non-seasonal depression. The mechanism of BLT is not fully understoodyet,butmajorhypothesesinSADinvolves resyn-chronizingcircadianrhythmsandrestoringneurotransmitter dysfunction.17---19 It is proposedthatbright light has
circa-dianphase---shiftingeffects inhumans.20 However,studies
investigating light therapy in SAD have not consistently demonstratedthe correlationsof phaseshift withclinical response.18,21 Also,astheantidepressanteffectofBLTcan
beseen inpatientswithoutdelayedcircadianrhythms, an additionalmechanismofactionmaybeinplace.22 Sinceit
22,00 20,00 18,00 16,00 14,00 12,00
Pretreatment After Treatment 2 Weeks After Treatment Hamilton Depression Scale
Estimated Marginal Means
Treatment Group
BLT+AD AD monotherapy
Figure1 ChangeinHamiltonDepressionScoreinBLT+ADandADmonotherapygroupswithtime.BLT:brightlighttherapy.AD:
antidepressants.
3200,00
Treatment Group BLT+AD
Pertreatment After Treatment 2 Weeks After Treatment
Lymphocyte Count
Estimated Marginal Means
AD monotherapy
3000,00
2800,00
2600,00
Figure2 ChangeinlymphocytecountinBLT+ADandADmonotherapygroupswithtime.
serotonincanreversethebeneficialeffectsoflighttherapy
inSAD,23---25 itis alsosuggestedthatbrightlight mayhave
directmonoaminergiceffects whicharesimilarto antide-pressant effect.26 Although there are observational and
randomizedcontrolledstudies showingthatBLTdecreases suicidalideation, several case reports27,28 have presented
a number of cases who attempted suicide after BLT. The presentstudyassessedsuicidalideationbeforeandafterthe treatmentand foundthat suicidalideas decreased signifi-cantlyaftertreatmentwithbothADandAD+BLT.However, patientswhoreceivedcombinedtherapyshowedmore sig-nificantremissioninsuicidalideationcomparedtopatients
receivingADmonotherapy.So,adjuvantBLTcanalsobeused safelyindepressivepatientswithsuicidalideation.
ExceptthePLR,alltheinflammatoryparameterschanged significantlyovertime,meaningthatbothtreatmentoptions have an effect on inflammatory response in depressive patients. The neutrophil countdecreased withtwoweeks of treatment whereas lymphocyte countincreased gradu-ally resulting in decreased NLR among all patients. NLR is a routinely used marker calculated from the neu-trophilandlymphocytecountsinthecompletebloodcount whichclearlyindicates theseverityofsystemic inflamma-tion indiseases such ascoronaryartery disease,diabetes
9,00 8,00 7,00 6,00 5,00 4,00 3,00 Pretreatment Treatment Group BLT+AD AD monotherapy
After Treatment 2 Weeks After Treatment The Beck Scale for Suicide Ideation
Estimated Marginal Means
Figure3 ChangeinBeckScaleforsuicideideationinBLT+ADandADmonotherapygroupswithtime.
Table3 Correlationbetweenclinicaloutcomeparametersandinflammatorymarkers.
Beforetreatment AfterTreatment 2weeksafter treatment
r p r p r p
BSSI --- Platelet/Lymphocyteratio −0.184 0.117b 0.012 0.920b−0.017 0.887b BSSI --- Meanplateletvolume 0.375 <0.001b−0.035 0.768b 0.021 0.862b BSSI --- Neutrophilcount −0.113 0.338b 0.043 0.717b−0.146 0.215b BSSI --- Lymphocytecount 0.124 0.294b 0.124 0.292b−0.165 0.161b BSSI --- Neutrophil/Lymphocyteratio −0.196 0.094b−0.051 0.664b 0.017 0.888b HAMDscale --- Platelet/Lymphocyteratio 0.188 0.110a 0.225 0.054a 0.108 0.362a HAMDscale --- Meanplateletvolume 0.163 0.166a 0.009 0.937a−0.005 0.965a HAMDscale --- Neutrophilcount −0.049 0.678a 0.023 0.843a 0.018 0.878a HAMDscale --- Lymphocytecount −0.229 0.049a−0.109 0.356a−0.035 0.767a HAMDscale --- Neutrophil/Lymphocyteratio 0.092 0.434a 0.119 0.313a 0.036 0.760a
a Pearsoncorrelationcoefficient. b SpearmanRhocorrelationcoefficient.
mellitus, Alzheimer’s disease, ulcerativecolitis, cirrhosis, and cancer.29---32 NLR has prognostic value in
cardiovas-cular diseases and various cancers independent of other factors.33---35MDDpatientswithhigherHDSscorewerefound
tohavehigherNLRvalues.36Itwasreportedthatincreasein
NLRwasassociatedwithmoreseveredepression.36Although
ourresultsshowedasignificantdecreaseinNLRwitheither treatments,wedidnotfindacorrelationbetweenNLRand depression severity. Similar to NLR, PLR is also a novel inflammatorymarkerwhichcanbeusedasaprognostic fac-torforcardiovasculardiseasesandcancer.Arecentstudy37
reportedthatthePLRwerehigherinpatientswithsevere major depression with psychotic features than in other patients and this can be useful for assessing the progno-sisofmajordepression.However,ourstudyneitherfound a significant differencein PLR in response to both treat-mentoptions,noracorrelationbetweenPLRanddepression severity. MPV is an indicator of platelet activity, the
relationship between MDD and increased platelet activity hasbeenpreviouslyreportedbyseveralstudies.38,39Patients
withmajordepression werefound tohave increasedMPV levelsincomparisonwithparticipantswithoutdepression39
andMPV wasfound significantly decreased after escitalo-pramtreatment.38Consistentwiththesefindings,ourstudy
showedthat,independentfromtreatmentarm,patientshad decreasedMPV twoweeksafter thetreatment, but there wasnosignificant correlationbetweendepressionseverity andMPV.
Theresults oftime×groupinteractionanalysisshowed nosignificant differencesbetweengroups apartfrom lym-phocyte count. After 2 weeks of treatment, patients whowere receiving AD monotherapy showed a negligible increase in lymphocyte count whereas patients receiving combinedtherapyshowedamarkedincreaseinlymphocyte number.ThisresultshowsthattheeffectofBLTisdissimilar totheeffectsofantidepressantsonlymphocytes.
Bright light can affect the immune system by two separate mechanisms:skin mediated and eye-brain medi-ated.Wavelengthsthatareabove400nanometer(nm)can penetrate into epidermal and dermal layers of the skin. Withintheselayers,lightcandirectlyinteractwith circulat-inglymphocyteswhichareresponsiblefromthepersistence ofimmunefunction.Anotherpossiblemechanismisan indi-rect way which involves transmission of light (400nm or above)throughretinatothebrain.Whenitreachestothe brain,itstimulatesspecificbrainareassuchasthepituitary, hypothalamus,andthepinealglandsinordertoproduce cer-tainneurochemicals such ashormones, neurotransmitters and neuropeptides. These neurochemicals might directly causealterationsinimmunefunction.40 Theskin-mediated
responsemightberesponsiblefor alterationsseenin lym-phocyte number in our combinedtherapy group which is notexpectedtobeobservedwithantidepressant monother-apy.Findingofthenegativecorrelationbetweenlymphocyte numberand severityof depression also supports the idea that lymphocyte count can be an important indicator of adjuvantBLTresponseinnon-seasonaldepression.
This study has several limitations. First, since the patients have been assigned totreatment alternatives by anon-randomizedmethod,thiscanresultindifferencesin baselinecharacteristicsbetweentwogroupscausingarisk ofselectionbias.Theseconfoundingfactorscanbeeither known or unknown factors. Although most of the known factors such as gender, employment status, medication compliance, social support and pretreatment depression severity were not significantly different between groups, it is impossible to control unknown factors without ran-domization.Second, sincethe patients were not blind to treatmentalternatives,placeboeffectcannotberuledout inobservedimprovementofdepressivesymptomswithlight therapy. Future randomized, sham controlled and double blindedclinicalstudieswillprovidehigherlevelofevidences fortheefficacyofBLTinnon-seasonaldepression.
Conclusion
Inconclusion,studies examining theeffectof BLTin non-seasonaldepressionarelimitedandinflammatoryresponses in these patients have not been studied yet. To the best ofourknowledge,thisstudyisthefirstwhichinvestigates theefficacyofBLTinnon-seasonaldepressionwithafocus oninflammatorymarkers.Presentstudyindicatedthat com-biningBLT,asawell-toleratedtreatment alternative,with classicalantidepressanttreatmentmodalitiescanbehelpful inpatientssufferingfromnon-seasonaldepressivedisorder aswell. Futurerandomized, shamcontrolled and double-blindclinicalstudieswillprovidehigherlevelofevidences fortheefficacyofBLTinnon-seasonaldepression.
Funding
Thisresearchdidnotreceiveanyspecificgrantfromfunding agenciesinthepublic,commercial,ornot-for-profitsectors.
Conflict
of
interest
Theauthorshavenoconflictofinteresttodeclare.
Acknowledgment
None.
References
1.LópezAD,MurrayCJL.Theglobalburdenofdisease:a compre-hensiveassessmentofmortalityanddisabilityfromdiseases, injuries,andriskfactorsin1990andprojectedto2020. Cam-bridge:HarvardUniversityPress;1996.
2.WorldHealthOrganization(WHO).Depressionfactsheet;2015 http://www.who.int/mediacentre/factsheets/fs369/en/ 3.American PsychiatricAssociation. Practiceguidelines for the
treatmentofpatientswithdelirium.AmJPsychiatry.1999;156 Suppl.:1---20.
4.ConnollyKR,ThaseME.Ifatfirstyoudon’tsucceed:areview oftheevidenceforantidepressantaugmentation,combination andswitchingstrategies.Drugs.2011;71:43---64.
5.FavaM.Diagnosisanddefinitionoftreatment-resistant depres-sion.BiolPsychiatry.2003;53:649---59.
6.TermanM,TermanJS.Lighttherapyforseasonaland nonsea-sonaldepression: efficacy,protocol,safety,andside effects. CNSSpectr.2005;10:647---63.
7.LieverseR,VanSomerenEJ,NielenMM,UitdehaagBM,SmitJH, HoogendijkWJ.Brightlighttreatmentinelderlypatientswith nonseasonalmajordepressivedisorder:arandomized placebo-controlledtrial.ArchGenPsychiatry.2011;68:61---70.
8.OldhamMA,CirauloDA.Brightlighttherapyfordepression:a reviewofitseffectsonchronobiologyandtheautonomic ner-voussystem.ChronobiolInt.2014;31:305---19.
9.PailG,HufW,PjrekE,WinklerD,WilleitM,Praschak-RiederN, etal.Bright-lighttherapyinthetreatmentofmooddisorders. Neuropsychobiology.2011;64:152---62.
10.EvenC,SchroderCM,FriedmanS,RouillonF.Efficacyoflight therapyinnonseasonaldepression:asystematicreview.JAffect Disord.2008;108:11---23.
11.GoldenRN,GaynesBN,EkstromRD,HamerRM,JacobsenFM, SuppesT,etal.Theefficacyoflighttherapyinthetreatment ofmooddisorders:areviewandmeta-analysisoftheevidence. AmJPsychiatry.2005;162:656---62.
12.TuunainenA,KripkeDF,EndoT.Lighttherapyfornon-seasonal depression.CochraneDatabaseSystRev.2004:CD004050. 13.KrishnadasR,CavanaghJ.Depression:aninflammatoryillness?
JNeurolNeurosurgPsychiatry.2012;83:495---502.
14.NajjarS,Pearlman DM,Alper K, NajjarA, Devinsky O. Neu-roinflammationand psychiatric illness.JNeuroinflammation. 2013;10:43.
15.Sayana P, Colpo GD, SimoesLR, Giridharan VV, Teixeira AL, QuevedoJ,etal.Asystematicreviewofevidencefortherole ofinflammatorybiomarkersinbipolarpatients.JPsychiatrRes. 2017;92:160---82.
16.MazzaMG,LucchiS,TringaliAGM,RossettiA,BottiER,ClericiM. Neutrophil/lymphocyteratioandplatelet/lymphocyteratioin mooddisorders:ameta-analysis.ProgNeuropsychopharmacol BiolPsychiatry.2018;84:229---36.
17.Levitan RD. The chronobiology and neurobiology of win-ter seasonal affective disorder. Dialogues Clin Neurosci. 2007;9:315---24.
18.LewyAJ,LeflerBJ,EmensJS,BauerVK.Thecircadianbasisof winterdepression.ProcNatlAcadSciUSA.2006;103:7414---9.
19.SohnCH,LamRW.Updateonthebiologyofseasonalaffective disorder.CNSSpectr.2005;10:635---46.
20.SkeneDJ,ArendtJ.Humancircadianrhythms:physiologicaland therapeuticrelevanceoflightandmelatonin.AnnClinBiochem. 2006;43:344---53.
21.BurgessHJ,FoggLF,YoungMA,EastmanCI.Brightlighttherapy forwinterdepression---isphaseadvancingbeneficial? Chrono-biolInt.2004;21:759---75.
22.Geoffroy PA, Schroder CM, Bourgin P. Light treatment in depression: an antique treatment with new insights. Sleep Med Rev. 2018;40:218---9, http://dx.doi.org/10.1016/ j.smrv.2018.03.002.
23.LamRW,ZisAP,GrewalA,DelgadoPL,CharneyDS,KrystalJH. Effectsofrapidtryptophandepletioninpatientswithseasonal affectivedisorder inremissionafterlight therapy. ArchGen Psychiatry.1996;53:41---4.
24.Neumeister A, Praschak-Rieder N, Besselmann B, Rao ML, Gluck J, Kasper S. Effects of tryptophan depletion on drug-free patients withseasonal affective disorderduring a stableresponse tobright lighttherapy. ArchGen Psychiatry. 1997;54:133---8.
25.Neumeister A, Turner EH, Matthews JR, Postolache TT, Bar-nettRL, Rauh M, et al. Effects of tryptophan depletion vs catecholamine depletion in patients with seasonal affective disorderinremissionwithlighttherapy.ArchGenPsychiatry. 1998;55:524---30.
26.NeumeisterA.Tryptophandepletion,serotonin,anddepression: wheredowestand?PsychopharmacolBull.2003;37:99---115. 27.HaffmansJ,LuciusS,HamN.Suicideafterbrightlight
treat-ment in seasonal affective disorder: a case report. J Clin Psychiatry.1998;59:478.
28.Praschak-RiederN,NeumeisterA,HesselmannB,WilleitM, Bar-nasC,KasperS.Suicidaltendenciesasacomplicationoflight therapyforseasonalaffectivedisorder:areportofthreecases. JClinPsychiatry.1997;58:389---92.
29.Kuyumcu ME, Yesil Y, Ozturk ZA, Kizilarslanoglu C, Etgul S, Halil M, et al. The evaluation of neutrophil---lymphocyte ratio in Alzheimer’s disease. Dement Geriatr Cogn Disord. 2012;34:69---74.
30.OzturkZA, Kuyumcu ME, Yesil Y, Savas E, Yildiz H, Kepekci Y,etal.Istherealink betweenneutrophil---lymphocyteratio
andmicrovascularcomplicationsingeriatricdiabeticpatients? JEndocrinolInvest.2013;36:593---9.
31.Tamhane UU, Aneja S,Montgomery D,Rogers EK,Eagle KA, Gurm HS. Association between admission neutrophil to lym-phocyteratio and outcomes in patientswithacutecoronary syndrome.AmJCardiol.2008;102:653---7.
32.TorunS, Tunc BD, Suvak B,Yildiz H, TasA, Sayilir A, et al. Assessmentofneutrophil---lymphocyteratioinulcerative coli-tis:apromisingmarkerinpredictingdiseaseseverity.ClinRes HepatolGastroenterol.2012;36:491---7.
33.BiyikM,UcarR,SolakY,GungorG,PolatI,GaipovA,etal.Blood neutrophil-to-lymphocyteratioindependentlypredictssurvival inpatients withlivercirrhosis.EurJGastroenterol Hepatol. 2013;25:435---41.
34.FowlerAJ,AghaRA.Neutrophil/lymphocyteratioisrelatedto theseverity ofcoronaryartery diseaseand clinicaloutcome inpatientsundergoingangiography---thegrowingversatilityof NLR.Atherosclerosis.2013;228:44---5.
35.ProctorMJ,McMillanDC,MorrisonDS,FletcherCD,HorganPG, ClarkeSJ. Aderivedneutrophil to lymphocyteratio predicts survivalinpatientswithcancer.BrJCancer.2012;107:695---9. 36.DemirS,AtliA,BulutM,IbilogluAO,GunesM,KayaMC,etal.
Neutrophil---lymphocyteratioinpatientswithmajordepressive disorderundergoingnopharmacologicaltherapy. Neuropsychi-atrDisTreat.2015;11:2253---8.
37.KayhanF,GunduzS,ErsoySA,KandegerA,AnnagurBB. Rela-tionships of neutrophil---lymphocyteand platelet---lymphocyte ratios withthe severityofmajordepression. PsychiatryRes. 2017;247:332---5.
38.Ataoglu A, Canan F. Mean platelet volume in patients with majordepression:effectofescitalopramtreatment.JClin Psy-chopharmacol.2009;29:368---71.
39.CananF,DikiciS,KutlucanA,CelbekG,CoskunH,GungorA, etal.AssociationofmeanplateletvolumewithDSM-IVmajor depressioninalargecommunity-basedpopulation:theMELEN study.JPsychiatrRes.2012;46:298---302.
40.Roberts JE.Lightand immunomodulation.Ann NYAcadSci. 2000;917:435---45.