Original Investigation
Published Online: 19.10.2018Corresponding author: Utku ADILAY
utkuadilay@hotmail.comUtku ADILAY
1, Bulent GUCLU
2, Levent DENIZ
3, Ramazan KAHVECI
1 1Balikesir University, School of Medicine, Department of Neurosurgery, Balikesir, Turkey2Ministry of Health, Dr. Lutfi Kirdar Kartal Research and Training Hospital, Neurosurgery Clinic, Istanbul, Turkey 3Marmara Pain Center, Istanbul, Turkey
This study has been presented as an oral presentation at the 24th Uludag Anesthesia Winter Symposium on March 2-4, 2018 at Bursa, Turkey.
Comparison of the Effect of Single Lumbar Transforaminal
Epidural Steroid Injections for the Treatment of L4-5 and
L5-S1 Paramedian Disc Herniation
ABSTRACT
deficit. Sometimes the pain can be unbearable but the patient does not want surgical intervention. Nerve root compression may stimulate inflammatory processes (14,17), providing a rationale for the use of corticosteroids to inhibit inflammation and alleviate pain. The transforaminal epidural injection of corticosteroids under fluoroscopic guidance delivers high concentrations of therapeutic agents to the site of pathology (5). Appropriately performed transforaminal epidural steroid
█
INTRODUCTION
R
adicular pain is most commonly caused by mechanicalcompression of the nerve root by lumbar disc herniation or peripheral foraminal stenosis and has considerable economic significance (7). In most cases, the pain stops spontaneously or can be relieved with conservative treatment. However, some lumbar disc herniation cases require surgical intervention because of persistent severe pain or neurological
AIM: To compare the outcomes of fluoroscopically guided transforaminal epidural steroid injections between L4-L5 paramedian
disc herniation and L5-S1 paramedian disc herniation for the treatment of radicular pain.
MATERIAL and METHODS: A total of 593 patients treated by transforaminal epidural steroid injections for the treatment of L4-5
paramedian disc herniation and 504 patients treated by transforaminal epidural steroid injections for the treatment of L5-S1 paramedian disc herniation were included in the study. All the patients were regularly followed up for 12 weeks. Preprocedural Visual Analogue Scale (VAS) scores, 12-week post-procedural VAS scores and complications were recorded.
RESULTS: The mean preprocedural and postprocedural VAS scores for L4-5 paramedian disc herniation were 63.09 ± 5.37 and
15.81 ± 3.58, respectively, and the mean preprocedural and postprocedural VAS scores for L5-S1paramedian disc herniation were 61.15 ± 5.45 and 27.06 ± 3.62, respectively, for radicular pain. There was a statistically significant difference between preprocedural and postprocedural VAS scores for L4-5 and L5-S1 paramedian disc herniation (p<0.05). Transforaminal epidural steroid injections for L4-5 paramedian disc herniation were more effective than transforaminal epidural steroid injections for L5-S1 paramedian disc herniation.
CONCLUSION: This study showed that transforaminal epidural steroid injections for L4-5 paramedian disc herniation were more
effective than transforaminal epidural steroid injections for L5-S1 paramedian disc herniation in the 12-week follow-up period.
KEYWORDS: Lumbar disc herniation, L4-L5, L5-S1, Paramedian disc herniation, Transforaminal epidural steroid injection
Utku ADILAY : 0000-0003-4867-244X
injections are clinically effective for treating lumbar and radicular pain (8,16,19). Epidural injection of steroids is a neural blockade which alters or interrupts nociceptive input, the reflex mechanism of the afferent fibres, self-sustaining activity of the neurons, and the pattern of central neuronal activities (6,11). Corticosteroids have also been shown to reduce inflammation by inhibiting either the synthesis or release of a number of pro-inflammatory mediators and by causing a reversible local anesthetic effect (6,18). Transforaminal epidural injections result in a significant reduction of pain scores in patients with lumbar radiculopathy when compared with pain scores of patients receiving no treatment, conservative management without injection therapy, and lumbar interlaminar epidural injections (15). Transforaminal injection of steroids may be dangerous if carelessly performed (3,10). The risks are low, and transforaminal epidural steroid injections appear to be cost effective, particularly in comparison with the costs associated with surgical intervention. The difference of the effect of transforaminal epidural steroid injections for the treatment of L4-5 and L5-S1 paramedian lumbar disc herniation has not been studied before. The aim of this study was to compare outcomes of fluoroscopically guided transforaminal epidural steroid injections of L4-5 paramedian disc herniation with L5-S1 paramedian disc herniation for the treatment of radicular pain.
█
MATERIAL and METHODS
Patients
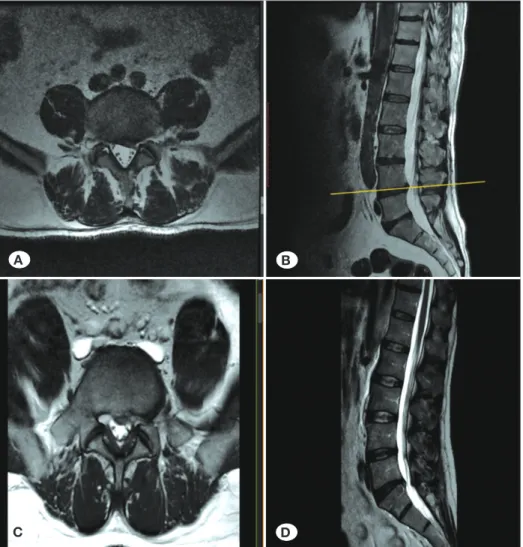
In total, 1097 patients with radicular pain because of L4-L5 or L5-S1 paramedian disc herniation, who did not benefit from previous medical treatments and who did not want surgical intervention, were included in this study. These patients were treated by transforaminal epidural steroid injections between March 2012 and May 2015. Injections were performed on the basis of radicular leg pain, magnetic resonance imaging (MRI) confirmation of relevant paramedian lumbar disc herniation, and failure of conservative therapy after an adequate trial. Inclusion criteria for the patients to be included in this study were: radicular leg pain; magnetic resonance imaging (MRI) confirmation of paramedian lumbar disc herniation of L4-L5 or L5-S1 (Figure 1A-D); failure of conservative therapy after an adequate trial; and at least one site of transforaminal epidural steroid injection. Patients were excluded from the study if they had previous spinal surgery at the same level; isthmic or degenerative spondylolisthesis; bony midsagittal diameter of spinal canal <8 mm; dynamic instability determined by the presence of sagittal vertebral translation >3 mm and angulation >10° on dynamic radiography; cauda equina syndrome; or lumbar disc herniation in >1 level.
Figure 1: Paramedian lumbar disc
herniations. A) Axial, and B) sagittal T2W MRI scans of L4-5 disc herniation.
C) Axial, and D) sagittal T2W MRI scans
of L5-S1 disc herniation.
A B
Our study was performed retrospectively. The whole study was conducted in accordance with the Declaration of Helsinki (1964). The procedure was performed following patients’ understanding and consent. All the patients received oral and written information regarding the treatment of lumbar disc herniation using transforaminal epidural steroid injections, and written informed consent was obtained from each patient. The major presenting symptoms of the patients were leg pain and low back pain. The mean duration of radicular pain before surgery was 6 months ± 0.3 months. Before injections, all patients received nonsteroidal anti-inflammatory or analgesic drugs.
MRI Data Analyses
All lumbar spine MRI examinations were performed on a 1.5 Tesla magnet (Philips Medical Systems, Eindhoven, the Netherlands). Images that were obtained at the level of the nerve root engagement were correlated with radicular pain. Preprocedural magnetic resonance images were analyzed by a well-experienced radiologist. The radiologist, who was blinded to all clinical information, analyzed the existence of L4-L5 or L5-S1 paramedian disc herniation. Postprocedural MRI was not obtained for every patient.
Procedure
Patients were placed in the prone position, and the procedure was performed using aseptic technique; 1% lidocaine was diffused at the needle insertion site. A 22-gauge Quincke spinal needle (Tae-Chang Industrial Co., Korea) was inserted using a preganglionic transforaminal approach under fluoroscopic
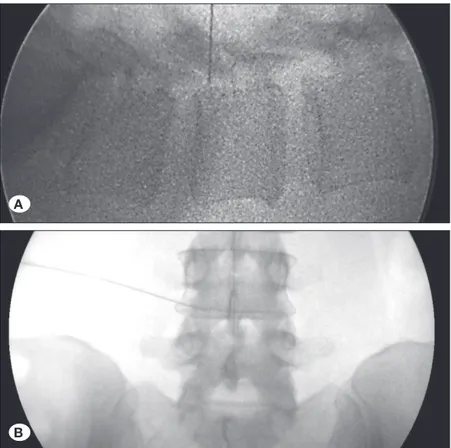
guidance. A syringe with a filter needle (Donghwa C&M, Korea) was used to prepare the solution as dexamethasone was stored in glass ampoules. Approximately 1 mL of contrast media (Pamiray, Dongkook Lifescience, Korea) was used to confirm epidural spread, and 3 mL of 0.33% lidocaine (Lidocaine HCl, Huons, Korea) with 4 mg dexamethasone (dexamethasone disodium phosphate, Yuhan, Korea) were injected (Figure 2A, B).
All the patients were reexamined 12 weeks after the procedure. Preprocedural and postprocedural Visual Analogue Scale (VAS) scores for radicular pain (20), and preprocedural and postprocedural neurologic examinations were recorded, along with any complications.
VAS Score Assessment
Preprocedural and postprocedural average VAS scores for radicular pain were calculated for each patient. Three different measures of radicular pain were obtained using a horizontal VAS, with 0 mm indicating no pain and 100 mm the worst imaginable pain. These measures were self-rated radicular leg pain (thigh and more distal) at present, and the minimum and maximum self-rated radicular leg pain during the last 3 days. An average score of pain (VAS score for radicular pain) was calculated from these three measures.
Statistical Method
Statistical analysis was performed using paired sample t test (for VAS). SPSS (21.0) software was used for statistical analysis. A p value and t value were obtained from the analysis.
Figure 2: Lumbar transforaminal epidural steroid
injection under C-arm guidance. A) Lateral view,
B) anteroposterior view.
A
increased neurological deficit. Two patients needed surgical intervention because the pain was relieved for 3 days after transforaminal epidural steroid injection but increased after 3 days; the pain was intense and these patients were operated for paramedian disc herniation. The other 3 patients were operated for increased neurological deficit. One of them had A p value of less than 0.05 was considered statistically
significant. To compare the outcomes of fluoroscopically guided transforaminal epidural steroid injections of L4-L5 paramedian disc herniation with L5-S1 paramedian disc herniation, the repeated measures ANOVA test was used.
█
RESULTS
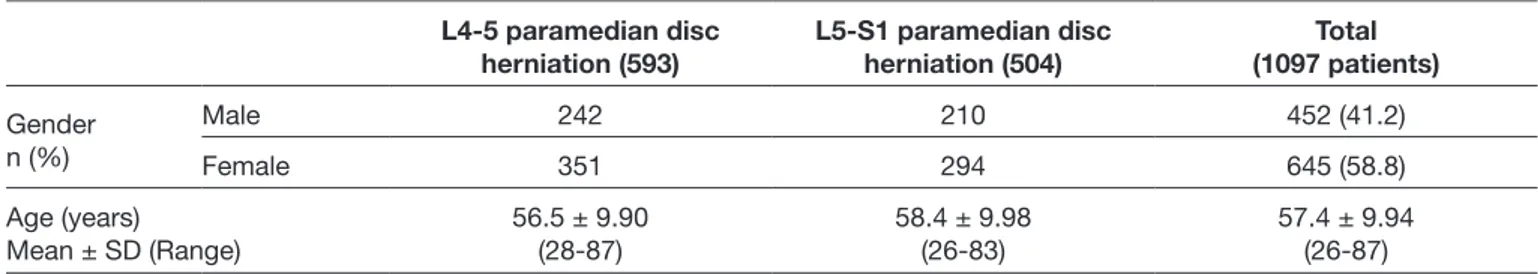
Of the 1097 patients in this study, 452 were male and 645 were female, with a mean age was 57.4 ± 9.94 (range, 26–87) years. 593 patients had 4-5 paramedian disc herniation and 504 patients had L5-S1 paramedian disc herniation (Table I). All the patients reported radicular pain. All the patients were treated using lumbar transforaminal epidural steroid injections. All the patients received regular follow up for 12 weeks after the procedure. For radicular pain, the mean pre-procedural and post-procedural VAS scores for L4-5 paramedian disc herniation were 63.09 ± 5.37 and 15.81 ± 3.58, respectively, and the mean pre-procedural and post-procedural VAS scores for L5-S1 paramedian disc herniation were 61.15 ± 5.45 and 27.06 ± 3.62, respectively. There was a statistically significant difference between preprocedural and postprocedural VAS scores for L4-5 and L5-S1 paramedian disc herniation, and p values were p<0.05 (Table II). Transforaminal epidural steroid injections for L4-5 paramedian disc herniation was more effective than transforaminal epidural steroid injections for L5-S1 paramedian disc herniation (Figure 3). There were no major complications; however, transforaminal epidural steroid injections group for the L4-5 paramedian disc herniation had 19 (4.7%) minor complications (including infection and cerebrospinal fluid fistula), and the L5-S1 paramedian disc herniation group had 16 (3.5%) minor complications. In total, 5 patients needed surgical intervention for unrelieved pain or
Table II: The Evaluation of the Preprocedural and Postprocedural VAS Scores and Number of Complications in L4-5 and L5-S1
Paramedian Lumbar Disc Herniation Patients Who Underwent Single Lumbar Transforaminal Epidural Steroid Injections
L4-5 paramedian TFESI patients
(593 patients) L5-S1 paramedian TFESI patients (504 patients) p
Before TFSEI After TFSEI Before TFSEI After TFSEI
VAS Score 63.09 ± 5.37 15.81 ± 3.58 61.15 ± 5.45 27.06 ± 3.62 p<0.05
No of Complications (%) 19 (4.7) 16 (3.5) p>0.05
TFESI: Transforaminal epidural steroid injection, VAS: Visual Analog Scale.
Table I: Demographic Features of the Paramedian Lumbar Disc Herniation Patients Who Underwent Transforaminal Epidural
Steroid Injection
L4-5 paramedian disc
herniation (593) L5-S1 paramedian disc herniation (504) (1097 patients)Total
Gender n (%) Male 242 210 452 (41.2) Female 351 294 645 (58.8) Age (years) Mean ± SD (Range) 56.5 ± 9.90(28-87) 58.4 ± 9.98 (26-83) 57.4 ± 9.94(26-87)
L: lumbar, SD: standard deviation.
Figure 3: Repeated measure ANOVA test showing that
transforaminal epidural steroid injections for L4-5 paramedian disc herniation was more effective than transforaminal epidural steroid injections for L5-S1 paramedian disc herniation.
Estimated Mar
ginal Means for V
AS Scor e 70.00 60.00 50.00 40.00 30.00 20.00 10.00 Preprocedural Postprocedural herniation level L4-5 L5-S1
S1 paramedian disc herniation group had 16 (3.5%) minor complications. This showed that that transforaminal epidural steroid injections is a safe procedure.
█
CONCLUSION
Paramedian disc herniations may cause severe pain and it may not be possible to relieve this pain with conservative treatment. Surgical treatment should be considered as the last resort in the treatment of lumbar herniated patients. Moreover some patients do not want any surgical treatment even if they have severe pain and sometimes neurological deficit. Some patients may not want to undergo surgery because they are old or are not suitable for general and/or spinal anesthesia. Transforaminal epidural steroid injection is a safe procedure for appropriate patients with paramedian lumbar disc herniation, as well as an effective method to relieve radicular pain and this study showed that transforaminal epidural steroid injections for L4-5 paramedian disc herniation was more effective than transforaminal epidural steroid injections for L5-S1 paramedian disc herniation in a 12-week follow-up period.
█
REFERENCES
1. Bhatia A, Flamer D, Shah PS, Cohen SP: Transforaminal epidural steroid injections for treating lumbosacral radicular pain from herniated intervertebral discs: A systematic review and meta-analysis. Anesth Analg 122(3):857-870, 2016 2. Bogduk N, Brazenor G, Christophides N, Cherry D, Fraser
R, Jenkins J: Epidural steroids in the management of low back pain and sciatica of spinal origin: Report of the working party. 2nd ed. National Health and Medical Research Council, Sydney, 1993:102–106
3. Bogduk N, Dreyfuss P, Baker R: Complications of spinal diagnostic and treatment procedures. Pain Med 9(1):11–34, 2008
4. Byun JM, Park HS, Woo JH, Kim J: The effects of a forceful transforaminal epidural steroid injection on radicular pain: A preliminary study. Korean J Pain 27(4):334-338, 2014
5. Derby R, Kine G, Saal J.A, Reynolds J, Goldthwaite N, White AH, Hsu K, Zucherman J: Response to steroid and duration of radicular pain as predictors of surgical outcome. Spine 17(6):176–183, 1992
6. Dietrich CL, Smith CE: Epidural granuloma and intracranial hypotension resulting from cervical epidural steroid injection. Anesthesiology 100(2):445–447, 2004
7. Frymoyer JW: Back pain and sciatica. N Engl J Med 318(5):291–300, 1988
8. Ghahreman A, Ferch R, Bogduk N: The efficacy of transforam-inal injection of steroids for the treatment of lumbar radicular pain. Pain Med 11(8):1149–1168, 2010
9. Kawada T: Lumbar transforaminal epidural steroid injection in patients with chronic unilateral radicular pain. Am J Phys Med Rehabil 97(3):e17,2018
10. Kennedy DJ, Dreyfuss P, Aprill CN, Bogduk N: Paraplegia following image-guided transforaminal lumbar spine epidural steroid injection: Two case reports. Pain Med 10(8):1389– 1394, 2009
neurological deficit at plantar flexion of the foot, tand he other two patients had neurological deficit at dorsiflexion of the foot.
█
DISCUSSION
The primary aim of our study was to compare the outcomes of fluoroscopically guided transforaminal epidural steroid injections of L4-L5 paramedian disc herniation with L5-S1 paramedian disc herniation for the treatment of radicular pain. For radicular pain, the mean preprocedural and postprocedural VAS scores for for L4-5 paramedian disc herniation were 63.09 ± 5.37 and 15.81 ± 3.58, respectively. and the mean preprocedural and postprocedural VAS scores for for L5-S1 paramedian disc herniation were 61.15 ± 5.45 and 27.06 ± 3.62, respectively. There was a statistically significant difference between preprocedural and postprocedural VAS scores for L4-5 and L5-S1 paramedian disc herniation (p<0.05). Transforaminal epidural steroid injections for L4-5 paramedian disc herniation was more effective than transforaminal epidural steroid injections for L5-S1 paramedian disc herniation. In the literature, the efficacy of lumbar epidural spinal injections for radicular pain ranges from 0 % to 100 % and lasts nearly 3 months (2,21). In some patients with lumbar disc herniations, conservative treatment and physical therapy may not provide adequate pain relief. More aggressive treatments such as transforaminal epidural steroid injection may be helpful to the patient before considering surgical therapy. Transforaminal epidural steroid injection provides significant short-term pain relief in patients suffering from a single level lumbar herniated disc and is a viable, effective short-term analgesic tool to address pain and may retard an early surgical intervention (13). An epidural steroid injection can decrease inflammation in the epidural space and can decrease pain in the affected nerve root. The steroid may be given epidurally but the transforaminal approach offers more benefit for increased analgesic efficacy. This may be due to increased spread of steroid solution and better contact of the steroid with the ventral side of the root and extruded disc material.
Various studies have shown the efficacy of transforaminal epidural steroid injections for the treatment radicular pain due to lumbar disc herniation (1,4,9,12). However, transforaminal epidural steroid injection may not show the same pain relieving effect for different levels of lumbar disc herniations. This may be due to anatomical and biomechanical reasons. In the literature, there is no article comparing the outcomes of fluoroscopically guided transforaminal epidural steroid injections of L4-L5 paramedian lumbar disc herniation with L5-S1 paramedian lumbar disc herniation for the treatment of radicular pain. Our study is first in the literature to compare the outcomes of fluoroscopically guided transforaminal epidural steroid injections of L4-L5 paramedian disc herniation with L5-S1 paramedian disc herniation for the treatment of radicular pain.
There were no major complications in our study; however, transforaminal epidural steroid injections group for the L4-5 paramedian disc herniation had 19 (4.7%) minor complications (including infection and cerebrospinal fluid fistula), and the
L5-16. Riew KD, Park JB, Cho YS, Gilula L, Patel A, Lenke LG, Bridwell KH: Nerve root blocks in the treatment of lumbar radicular pain. A minimum five-year follow. J Bone Joint Surg Am 88(8):1722-1725, 2006
17. Saal JS: The role of inflammation in lumbar pain. Spine 20(16):1821–1827, 1995
18. Tachihara H, Sekiguchi M, Kikuchi S, Konno S: Do corticosteroids produce additional benefit in nerve root infiltration for lumbar disc herniation. Spine 33:743–747, 2008 19. Vad VB, Bhat AL, Lutz GE, Cammisa F: Transforaminal epidural
steroid injections in lumbosacral radiculopathy: A prospective randomized study. Spine 27(1):11–16, 2002
20. Wewers ME, Lowe NK: A critical review of visual analogue scales in the measurement of clinical phenomena. Res Nurs Health 13:227-236, 1990
21. White AH, Derby R, Wynne G: Epidural injections in the diagnosis and treatment of low back pain. Spine 5:78–86, 1980
11. Manchikanti L: Role of neuraxial steroids in interventional pain management. Pain Physician 5(2):182–199, 2002
12. Manchikanti L, Cash KA, Pampati V, Falco FJ: Transforaminal epidural injections in chronic lumbar disc herniation: A randomized, double-blind, active-control trial. Pain Physician 17(4):489-501,2014
13. Natarajan S, Anjan Venkataraman Krishnamurthy, Kalanithi R, Ilavarasan MD: Study on the functional outcome of fluoroscopically guided transforaminal epidural steroid injections in patients suffering from lumbar disc herniation. Int J Res Orthop 3(3):607-613, 2017
14. Olmarker K, Størkson R, Berge OG: Pathogenesis of sciatic pain: A study of spontaneous behaviour in rats exposed to experimental disc herniation. Spine 27(12): 1312–1317, 2002 15. Parr AT, Diwan S, Abdi S: Lumbar interlaminar epidural
injections in managing chronic low back and lower extremity pain: A systematic review. Pain Physician 12(1):163–188, 2009