Full Terms & Conditions of access and use can be found at
https://www.tandfonline.com/action/journalInformation?journalCode=icbi20
Chronobiology International
The Journal of Biological and Medical Rhythm Research
ISSN: 0742-0528 (Print) 1525-6073 (Online) Journal homepage: https://www.tandfonline.com/loi/icbi20
The relationship between chronotype and obesity
in children and adolescent with attention deficit
hyperactivity disorder
Serhat Türkoğlu & Fatih Hilmi Çetin
To cite this article: Serhat Türkoğlu & Fatih Hilmi Çetin (2019) The relationship between chronotype and obesity in children and adolescent with attention deficit hyperactivity disorder, Chronobiology International, 36:8, 1138-1147, DOI: 10.1080/07420528.2019.1622131
To link to this article: https://doi.org/10.1080/07420528.2019.1622131
Published online: 10 Jun 2019.
Submit your article to this journal
Article views: 390
View related articles
View Crossmark data
The relationship between chronotype and obesity in children and adolescent
with attention deficit hyperactivity disorder
Serhat Türkoğlu and Fatih Hilmi Çetin
Department of Child and Adolescent Psychiatry, Selçuk University Faculty of Medicine, Konya, Turkey
ABSTRACT
Children and adolescents with Attention Deficit Hyperactivity Disorder (ADHD) have a high prevalence of obesity, but the relationship between these two problems is not clear. Chronotype preferences may be one of the possible mechanisms underlying the link between ADHD and obesity. This is the first study to investigate whether chronotype preferences are a mechanism linking ADHD symptoms to obesity in children and adolescents. This cross-sectional study included 110 drug-naive children and adolescents aged 7–17 years with ADHD. The Kiddie Schedule for Affective Disorders and Schizophrenia-Present and Lifetime Version (K-SADS-PL) was used to diagnose ADHD or to exclude psychiatric comorbidity. The Conners’ Parents Rating Scale-Revised Short Version (CPRS-RS) and Children’s Chronotype Questionnaire (CCQ) were used to assess the severity of ADHD symptoms and chronotype preferences. Body mass index (BMI) was calculated and classified according to national age- and gender-specific reference values. The participants were divided into three groups as normal weight (<85%, n = 38), overweight (85%-95%, n = 30) and obesity (>(85%-95%, n = 42) according to their BMI percentile. There were statistically significant differences between the three groups in terms of chronotype preference (p = .000). Morningness preference was 86.84% in the normal BMI group and 26.19% in the obese BMI group. Eveningness preference was 7.89% in the normal BMI group and 61.90% in the obese BMI group. There was a correlation between the BMI percentile scores and the morningness/eveningness scale (M/E) scores. Moreover, there was a correlation between the BMI percentile scores and the oppositional and ADHD index scores. According to logistic regression analysis, the odds ratio of having evening type for obesity was 5.66 and the odds ratio of having morning type for normal weight was 13.03. Independently from ADHD symptoms, eveningness was directly related to obesity and morningness was directly related to normal weight. Prospective studies should be performed to better understand the relationship between ADHD, overweight/obesity and chronotype. ARTICLE HISTORY Received 30 March 2019 Revised 8 May 2019 Accepted 19 May 2019 KEYWORDS chronotype; obesity; attention deficit hyperactivity disorder; child/adolescent Introduction
Attention Deficit Hyperactivity Disorder (ADHD) ADHD is one of the most common neurodevelop-mental disorders in childhood. Worldwide, it ranges from 5.3% to 7.1% in school-age children. It is characterized by developmentally inappropri-ate levels of inattention, hyperactivity, and impul-sivity (Polanczyk et al. 2007). 65% of childhood-onset cases continues into adulthood (Faraone et al. 2006). Due to its characteristic symptoms and related conditions/disorders, ADHD creates a difficult situation for the society in terms of psychological dysfunction, social and financial costs, vocational outcomes, and familial stress (Doshi et al. 2012). ADHD shows prominent
heterogeneity in clinical, etiological and pathophy-siological aspects similar to all complicated medi-cal and psychiatric disorders. Although the comorbidity between ADHD and psychiatric dis-orders was widely investigated, its relationship with somatic problems was less pronounced (Biederman 2005). In recent years, however, there has been strong evidence demonstrating that there is a relationship between neuropsychiatric disor-ders and medical problems. Especially, the rela-tionship between ADHD and obesity has been focused. The idea of this potential linkage is of great importance for public health because of the rising risk of obesity and serious diseases asso-ciated with obesity (including diabetes, cardiovas-cular disease and cancer) (Ng et al. 2014).
CONTACTSerhat Türkoğlu drserhat@gmail.com Department of Child and Adolescent Psychiatry, Selçuk University Faculty of Medicine, Konya 42050, Turkey.
CHRONOBIOLOGY INTERNATIONAL 2019, VOL. 36, NO. 8, 1138–1147
https://doi.org/10.1080/07420528.2019.1622131
Obesity
Obesity is a major growing health problem in chil-dren and adolescents. It has serious and risky con-sequences for morbidity and mortality such as sleep apnea, diabetes mellitus, hyperlipidemia, hyperten-sion, and cancer. In addition to medical problems, obesity causes psychosocial problems such as stig-matization and psychiatric disorders (Daniels et al.
2005). Evidence also suggests that childhood obesity can predict adulthood obesity (Must 2003). The Global Burden of Disease Study 2017 (GBD2017), coordinated by the Institute for Health Metrics and Evaluation (IHME), has recently estimated that obe-sity includes approximately 110 million children and adolescents (Collaborators 2017). Obesity is a complex multifactorial chronic disease affected by both genetic and environmental factors. Previous research focused on the environmental risks asso-ciated with dietary intake and lifestyle (e.g., physical inactivity). However, coexisting psychological symp-toms and disorders including ADHD may play an important role in obesity (Cortese et al. 2015). Recent research has revealed a link between ADHD and obesity. Several studies have demonsrated that childhood and adulthood obesity is associated with childhood ADHD (Cortese et al. 2013). Similarly, a recent study has shown that children with ADHD had higher BMI scores than children without ADHD and that stimulant medications reduced early child-hood BMI rise; however, this reduction was not protective for obesity in the longer term (Schwartz et al. 2014). Fuemmeler et al. reported that both inattention and hyperactive–impulsive symptoms were associated with the prevalence of obesity in individuals with ADHD (Fuemmeler et al.2011).
Chronotype
Humans show cyclical rhythmicity in a variety of cognitive, psychological, physiological, behavioral, and hormonal processes. This cyclic structure called circadian rhythm is affected by exogenous and endo-genous factors. It also changes many processes such as mood, cognition, sleep-wake cycles, hormone levels, and temperature. Chronotype can be defined as a trait determining individual circadian preference in rhythm relative to external light/dark cycles (Adan et al. 2012; Dursun et al. 2015; Nielsen 2010; Selvi
et al. 2007; Wirz-Justice 2003). Chronotypes can generally be grouped into three types as morning, intermediate, and evening types. These types vary according to physical and mental activities, usual meal times, sleep times, waking times, performance, mood, alertness, and appetite. Individuals with morningness go to sleep earlier at night, wake up earlier, and have a relatively stable sleep rhythm than individuals with eveningness. Individuals with morningness prefer starting their daily physical and mental activities earlier and are more productive in the early hours of day. Individuals with eveningness show opposite characteristics in all of the specified fields. Intermediate types exhibit both morningness/ eveningness characteristics (Selvi et al.2017). Study investigating the link between chronotypes and per-sonality traits have reported that eveningness-type individuals become more outward-looking, have lower levels of avoidance behaviours, take more risks, tend to be more impulsive, and have high-sensation seeking personalities in contrast to morn-ingness- and intermediate-type individuals (Díaz-Morales2007).
Chronotype and ADHD
One of the strongest and most consistent data reported in the studies showing the relationship between ADHD and chronotype preference is that there was a correlation between eveningness and ADHD symptoms (Vogel et al. 2015). There is a bidirectional relationship between evening types and ADHD. In addition to ADHD, disruptive and impulsive behaviors are more common in evening-ness-type individuals (Imeraj et al. 2012). Many recent studies have demonsrated that there are asso-ciations between eveningness and irregular sleep-wake rhythm, worse sleep quality, sleep problems (such as difficulty going to sleep), delayed sleep onset, daytime sleepiness, tiredness in children and adolescents with ADHD (Durmuş et al. 2017; Van der Heijden et al.2005). In addition, several studies on eating behaviors and circadian preferences reported that individuals with eveningness had worse control over feeding than individuals with morningness. This evidence suggests that not falling asleep and staying up late at night can lead to excessive intake of foods (Schmidt and Randler
hyperactivity/impulsivity appear to mediate the rela-tionship between chronotype preference and feed-ing. Chronotype preferences (especially evening type) may be a component linking ADHD symp-toms to obesity/overweight. In rhythm disturbances (especially evening type), this relationship indicates that sleep disorders and inappropriate eating pat-terns may lead to obesity in children and adolescents with ADHD in the long term (Arble et al. 2010; McClung2013; O’reardon et al.2004).
Chronotype and obesity
The mechanisms of the relationship between obe-sity and chronotype are not completely under-stood in children and adolescents, but the current data highlight that sleep deprivation/restriction, levels of physical activity, and meal timing/habits in relation to chronotype may explain this connec-tion (Arora and Taheri 2015; Schaal et al. 2010). Some studies have shown that eveningness is sign-ificantly linked to obesity when compared to morningness (Culnan et al. 2013; Lucassen et al.
2013; Yu et al. 2015). In a broad sample of chil-dren, several authors have demonstrated that sleep restriction is significantly associated with increased central adiposity determined by waist circumfer-ence (Chaput and Tremblay2007). Similarly, other authors have showed that eveningness is associated with higher body mass index (BMI) z-scores and unhealthy eating patterns (Arora and Taheri2015; Lucassen et al. 2013). Eveningness has been asso-ciated with poor dietary control, larger portion, high total calorie/cholesterol intake, late-night eat-ing, and a tendency to skip/omit breakfast in rela-tion to unhealthy eating patterns (Mota et al.2016; Nakade et al.2009). It has been also revealed that eveningness is significantly associated with lower levels of physical activity and sedentary lifestyles when compared to morningness (Wennman et al.
2015). Interestingly, adult studies have indicated that bariatric surgery is less effective in evening-type patients than in morning-evening-type patients and that evening-type patients lose less weight than morning-type patients after obesity surgery due to both eating habits and physical activity (Ruiz-Lozano et al.2016).
In the light of these data, it can be said that both circadian system and ADHD can affect sleep–wake cycles, feeding and impulsivite and may cause obesity after a certain period of time. The relation-ship between chronotype preference, obesity, and ADHD has not been studied in children and ado-lescents as far as we know. The aim of this study was to investigate the associations between ADHD symptoms, BMI percentiles/obesity, and circadian rhythm differences in children and adolescents with ADHD.
Materials and methods
Subjects and study design
This cross-sectional study included 110 drug-naive children and adolescents aged 7–17 years with ADHD. It was conducted in the Department of Child and Adolescent Psychiatry at Selcuk University in Turkey. It was approved by the Local Ethics Committee of Selcuk University. Children and adolescents with ADHD who agreed to partici-pate were included in the study. Those with comor-bid psychiatric disorders (e,g., neurodevelopmental disorders, psychosis, depression, generalized anxiety disorder, substance abuse), genetic or neurological disorders (e.g., epilepsy), endocrinological or allergic diseases, and chronic systemic diseases were excluded from the study. While 4 parents rejected to participate in the study, 39 children were excluded from the study based on the exclusion/inclusion criteria. All participants were evaluated for psychia-tric disorders by the Kiddie Schedule for Affective Disorders and Schizophrenia-Present and Lifetime Version (K-SADS-PL). The Sociodemographic Data Collection Form, Conners’ Parents Rating Scale-Revised Short Version (CPRS-RS) and Children’s Chronotype Questionnaire (CCQ) were adminis-tered to them. Body mass index (BMI) was objec-tively calculated for each participant by dividing weight in kilograms (kg) by height in square meters (m2) and classified according to national age-and gender-specific reference values. Considering scientific standards, obesity was defined as ≥95th percentile BMI while overweight was defined as≥ 85th to ≤ 94th percentile.
Kiddie schedule for affective disorders and schizophrenia-present and lifetime version (K-SADS-PL)
It was used to screen for psychopathology in the participants. It is a semi-structured interview used for children and adolescents aged between 6 and 18 years and was prepared according to DSM-III and DSM-IV diagnostic criteria (Kaufman et al.
1997). It contains subheadings such as affective disorders, psychotic disorders, anxiety disorders, externalizing disorders, alcohol/substance abuse, and eating and tic disorders. It was translated and adapted into Turkish in 2004 by Gokler et al. who conducted the validity and reliability study of the Turkish version of the scale (Gökler et al.
2004). In this scale, psychopathologies are exam-ined by combining the data obtaexam-ined from chil-dren/adolescents and their parents by child and adolescent psychiatrists. If there is any conflict or inconsistency between different sources, the phy-sician’s decision is based on clinical evaluation. It assesses both current and past psychopathology.
Children’s chronotype questionnaire (CCQ) It was developed to investigate sleep problems/ habits of children by Owens et al and consists of 33 items (Owens et al.2000). It is the commonly used assessment questionnaire to define circadian rhythm differences. It is a parent-report, 27-item mixed-format questionnaire resulting in multiple measures of chronotype in children: the midsleep point on free days (MSF), a morningness/even-ingness scale (M/E) score, and a five-point chronotype (CT) score. It consists of 16 items on sleep/wake parameters (e.g., bedtime, lightsoff time, sleep latency, wake-up time, get-up time, fully alert time, regular naps) for scheduled days and free days, 10 Likert-type questions (range, 10–48) and a single item on chronotypes. Three different measures of children’s chronotypes are as follows: morningness type, intermediate type and eveningness type, which are classified using an M/E scale score of ≤23, 24–32, and ≥33. Dursun et al. conducted reliability and validity studies of the Turkish form (Dursun et al.2015). Turkish CCQ provided internal consistency with a Cronbach’s alpha of 0.653. After the factor
analysis was performed, it was decided that the scale would be included in evaluations as a whole (single factor).
Conners’ parents rating scale-revised short version (CPRS-RS)
It is the most useful and popular rating scale for ADHD domains. Conners et al. revised this scale (Conners et al. 1998). It contains 27 items and was translated and adapted for Turkish children by Kaner et al. The Turkish version of the scale was found to be reliable, valid, and appropriate for clinical purpose and research (Kaner et al. 2013). Each item is answered to on a 4-point Likert-type scale by parents (0 = never, 1 = rarely, 2 = often, and 3 = always). There are four subscales including oppositional (6 items), cognitive problem/inattention (6 items), hyperactivity (6 items) and ADHD index (12 items). The Cronbach’s alpha coefficient of the scale was deter-mined to be between 0.73 and 0.86. It shows high test– retest reliability (between 0.56 and 0.72).
Statistical analysis
Statistical analysis was performed using IBM SPSS Statistics for Windows Version 22.0 (SPSS Inc; Chicago, IL, USA). Descriptive statistics were used to describe the demographic and clinical character-istics of the participants. For normally distributed variables, ANOVA and Tukey’s post hoc test were used to analyze differences between groups accord-ing to chronotype preference. For non-normally dis-tributed variables, the Kruskal-Wallis test was used to analyze differences between groups according to chronotype preference. The relationships between psychological test scores and clinical variables were evaluated using the Pearson and Spearman correla-tion coefficients. The predictors of BMI percentile score/obesity such as age, gender, ADHD symptom severity, and chronotype preference were deter-mined using logistic regression analysis. A p-value less than 0.05 was considered statistically significant.
Results
The total number of participants in the study was 110. The mean age was 10.30 ± 2.44 years (range, 7–17 years). The study group consisted of 78 boys
(70.9%) and 32 girls (29.10%). The participants were divided into three groups as normal weight (<85%), overweight (85–95%) and obesity (>95%) according to their BMI percentile. There were no statistically significant differences between the three groups in terms of the age, gender, parental educational level, and socioeconomic level. The study group consisted of 61 morning-type patients (55.45%), 13 intermediate-type patients (11.81%) and 36 evening-type patients (32.72%). There were no statistically significant differences between these three groups in terms of age and gender (Table 1).
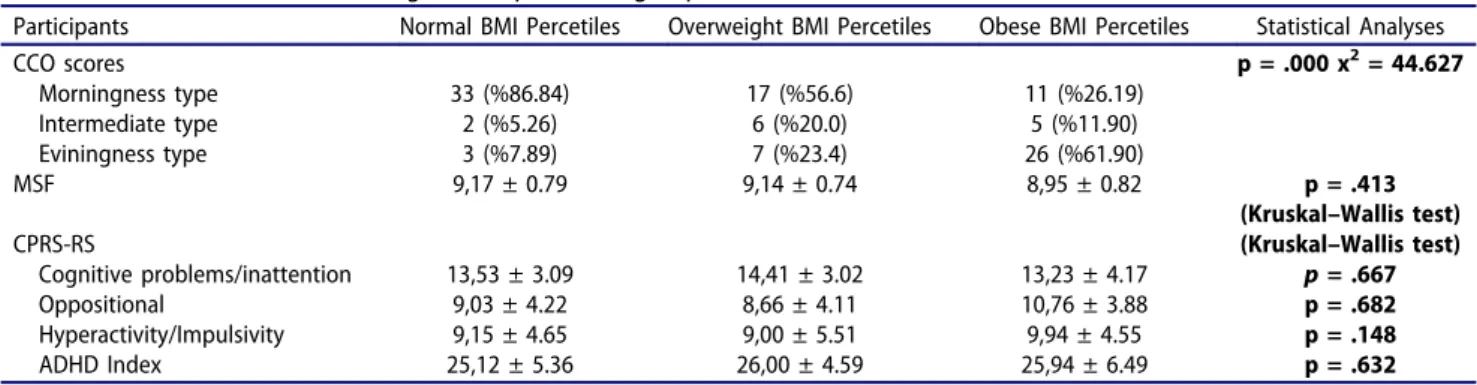
There were no statistically significant differences between the three groups in terms of the CPRS-RS subscale scores (cognitive problems/inattention, oppositional, hyperactivity, and ADHD index)
(Table 2). There were statistically significant differ-ences between the three groups in terms of chron-otype preference (p = .000) (Table 2). Morningness preference was 86.84% in the normal BMI group and 26.19% in the obese BMI group. Eveningness pre-ference was 7.89% in the normal BMI group and 61.90% in the obese BMI group. There were no statistically significant differences between the three groups in terms of the CCQ-MSF score.
The Spearman correlation coefficient was used to analyze the relationships between the BMI per-centile scores and the CPRS-RS subscale scores, the M/E and MSF scores of the CCQ. There was a correlation between the BMI percentile scores and the morningness/eveningness scale (M/E) scores. Moreover, there was a correlation between the BMI percentile scores and the oppositional and
Table 1.Sociodemographic features.
Participants Normal BMI Percetiles Overweight BMI Percetiles Obese BMI Percetiles Statistical Analyses
Male Gender 48 (%75) 8 (%66.6) 22 (%64.7) p = .533 x2= 1.258
Age 10.42 ± 2.49 10.50 ± 2.81 10.02 ± 2.24 p = .769
(Kruskal–Wallis test)
Educational level of the Father p = .712 x2= 3.739
Primary school 13 1 3
Secondary school 9 1 6
High school 19 5 13
University 23 5 12
Educational level of the Mother p = .383 x2= 6.372
Primary school 17 4 4
Secondary school 12 1 9
High school 17 2 12
University 18 5 9
Parents who live together 57 9 29 p = .418 x2= 1.745
Current psychiatric symptoms of fathers 4 0 2 p = .318 x2= 1.578
Current psychiatric symptoms of mothers 9 1 4 p = .457 x2= 1.779
Level of income (per month) p = .191 x2= 6.118
Low 10 6 8
Middle 25 16 30
High 3 7 3
Table 2.CPRS-RS and CCQ according to BMI percentile groups.
Participants Normal BMI Percetiles Overweight BMI Percetiles Obese BMI Percetiles Statistical Analyses
CCO scores p = .000 x2= 44.627 Morningness type 33 (%86.84) 17 (%56.6) 11 (%26.19) Intermediate type 2 (%5.26) 6 (%20.0) 5 (%11.90) Eviningness type 3 (%7.89) 7 (%23.4) 26 (%61.90) MSF 9,17 ± 0.79 9,14 ± 0.74 8,95 ± 0.82 p = .413 (Kruskal–Wallis test) CPRS-RS (Kruskal–Wallis test) Cognitive problems/inattention 13,53 ± 3.09 14,41 ± 3.02 13,23 ± 4.17 p= .667 Oppositional 9,03 ± 4.22 8,66 ± 4.11 10,76 ± 3.88 p = .682 Hyperactivity/Impulsivity 9,15 ± 4.65 9,00 ± 5.51 9,94 ± 4.55 p = .148 ADHD Index 25,12 ± 5.36 26,00 ± 4.59 25,94 ± 6.49 p = .632
CPRS-RS; Conners’ Parents Rating Scale-Revised Short Version. CCQ; Children’s Chronotype Questionnaire
MSF; Midsleep point on free days
ADHD index scores. There was a correlation between the CCQ-MSF times and the oppositional and ADHD index scores. The results of Spearman correlation are presented inTable 3.
Risk factors for obesity (>95th percentile) were evaluated using logistic regression analysis (enter model). According to this analysis, the odds ratio of having evening type for obesity was 5.66 (OR 5.66, Cl 1.91–16.81) and the odds ratio of having morning type for normal weight was 13.03 (OR 13.03, Cl 1.46–116.14) (Table 4).
Discussion
In our study, the participants were divided into three groups according to their BMI percentile and evaluated in terms of BMI percentile and chron-otype, and the associations between factors affect-ing BMI percentile and ADHD symptoms were examined. To our knowledge, this is the first study to investigate the relationship between chronotype preferences and BMI percentiles in children and adolescents with ADHD, which is an important predictor of obesity. The main find-ing of the present study was that there was a definite link between evening type and obesity. Morningness preference was 86.84% in the normal BMI group and 26.19% in the obese BMI group. Eveningness preference was 7.89% in the normal BMI group and 61.90% in the obese BMI group. In addition to these data, the odds ratio of having evening type for obesity was 5.66 and the odds ratio of having morning type for normal weight was 13.03. These are very powerful data that show the importance of chronotype preference.
ADHD has a high level of heritability indicat-ing a significant genetic component (Matthews
et al. 2014). Interestingly, some authors have suggested that sleep/wake behaviour can contri-bute to the core symptoms of ADHD such as inattention, hyperactivity, impulsivity, and cog-nitive/behavioral symptoms (Babkoff et al. 1991; Coogan and McGowan 2017). The strongest and most consistent result reported in several studies on ADHD is that there is an association between later chronotype (evening preference) and ADHD symptoms (Baird et al. 2012; Gruber et al.2012). In our study, the rate of eveningness preference in children and adolescent with ADHD was 32.72%. Studies investigating the link between ADHD and chronotype have demonsrated that increased levels of ADHD symptoms, poorer sustained attention on a continuous performance test, excessive day-time sleepiness/inattention, and unstable timing of days are associated with evening preference in individuals with ADHD (Kooij and Bijlenga
2014; Rybak et al. 2007; Vogel et al. 2015). In our study, there were no significant differ-ences in ADHD symptoms between the three groups, but there were significant differences in chronotype preferences between the three groups. It may demonsrate that chronotype preference has an independent effect on BMI percentile. Our results may support the argument that evening
Table 3.Spearman product–moment correlation coefficients.
1 2 3 4 5 6 7 1. O 1.000 2. C/I .254** 3. H/I .480** .374** 4. ADHDI .346** .752** .587** 5. M/E .212* .115 .001 .147 6. MSF −.207* −.157 −.122 -,281** −.363** 7. PERC .247** .136 .172 .210* .528** −.139 1.000
Correlation is significant at the 0.01 level (2-tailed).**Correlation is significant at the 0.05 level (2-tailed).*
MSF; Midsleep point on free days. M/E; Morningness/eveningness scale score. PERC; Percentile Score. ADHDI; ADHD Index Score. O; Oppositional Score. C/I; Cognitive problem/Inattention Score. H/I; Hyperactivity/Impulsivity Score.
Table 4.Logistic regression analysis enter model for obesity.
B S.E. Wald Sig. Exp(B)
Confidence Interval %95 Age −161 117 1,897 168 851 677–1,071 Gender 229 597 147 701 1,257 390–4.054 Morningness type 2,567 1,116 5,291 021 13,031 1,462–116.148 Eviningness type 1,734 555 9,771 002 5,666 1,910–16.811 ADHD Index −019 045 174 677 982 899–1.071
preference is a mechanism linking ADHD to obe-sity. We believe that the fact that the odds ratio of having morning type for normal weight was 13.03 is associated with this condition. Similar to our results, Vogel et al. demonstrated that both inat-tentive and hyperactive-impulsive symptoms were not directly related to obesity (Vogel et al. 2015). ADHD and circadian rhythm may share a common genetic etiology; however, we believe that their effects on obesity are independent of each other. The circadian rhythm is encoded and regulated at the genetic level by a number of CLOCK genes. CLOCK gene products are con-trolled by the formation of a series of interlocking transcriptional feedback loops (Zhang et al.2014). Some genetic studies have shown that there is an association between circadian CLOCK gene poly-morphisms and ADHD. Kissling et al., Xu et al. and Jeong et al. have reported that some single nucleotide polymorphisms (SNPs) in CLOCK are associated with ADHD symptoms (Jeong et al.
2014; Kissling et al. 2008; Xu et al. 2010). It has been indicated that individuals with eveningness are characterized as being more outward-looking, high risk-takers, high sensation seekers, indepen-dent and having lower levels of avoidance beha-viours and perseverance similar to individuals with ADHD (Adan et al.2010; Ponzi et al.2014). It has been reported that individuals with eveningness have worse control over feeding, are more likely to skip breakfast and exhibit excessive food con-sumption (especially at night) (Fleig and Randler
2009; Schmidt and Randler 2010). The nature of both ADHD and evening preference seems to increase the risk of obesity. This may explain that 61.90% of obese individuals with ADHD in our study had eveningness preference.
In our study, the Spearman correlation analysis revealed a significant correlation between the BMI percentile scores and the oppositional and ADHD index scores. In studies investigating the link between ADHD and obesity, the three pathways were hypothesized: (1) obesity/overweight or health conditions associated with obesity/over-weight such as sleep-disordered breathing and excessive daytime sleepiness may cause ADHD or increase ADHD symptoms, (2) Common biologi-cal dysfunction leads to both ADHD and obesity, and (3) ADHD contributes to obesity (Cortese and
Vincenzi 2012). There are data showing that abnormal eating behaviors cause ADHD symp-toms. Patients with bulimia nervosa or other abnormal eating behaviors may present with impulsive and repeated intervals of their activities to get food. It has been indicated that abnormal activities and intervals lead to ADHD symptoms, such as inattention, impulsivity, disorganization, and restlessness (Cortese et al. 2007). The other hypothesis, explaining the relationship between obesity and ADHD, can be explained by “hypoar-ousal theory”. According to this theory, sleep-disordered breathing and excessive daytime sleepi-ness are more common in individuals with obese and therefore obese people can demand more sleep. They may use motor hyperactivity and impulsivity as a strategy to stay awake and alert (Weinberg and Brumback1990). In relation to this theory, meta-analyses have shown that excessive daytime sleepiness and sleep-disordered breathing are common in patients with ADHD versus con-trols (Cortese et al.2009). The association between obesity and excessive daytime sleepiness has been shown in many studies. It is also seen to be inde-pendent of sleep-disordered breathing or other sleep disturbances. Vgontzas et al. showed that the main cause of excessive daytime sleepiness in obese individuals was circadian rhythm abnormal-ities, not sleep-disordered breathing or other sleep disorders (Vgontzas et al. 2006). Many studies have demonstrated that individuals with evening-ness represent increasing levels of excessive day-time sleepiness and more irregular sleep-wake habits (Adan et al. 2006; Ong et al. 2007). Therefore, it is inevitable that the risk of obesity increases significantly in children and adolescents with ADHD having evening preference. The other potential link between ADHD and obesity is that two conditions are different expressions of com-mon underlying biological mechanisms. “Reward deficiency syndrome” is thought to underlie the etiology of both ADHD and obesity. Substance use, risk-taking, and inappropriate eating are behaviors related to insufficient dopamine-related natural reinforcement (Comings and Blum 2000; Heiligenstein and Keeling 1995). It has been shown that risk-taking behaviors are frequently seen in patients with circadian rhythm abnormal-ities (especially evening type) and are considered
to underlie the etiology of both ADHD and obe-sity. The third hypothesis on the link between ADHD and obesity is that behavioral and cogni-tive deficits of ADHD may show an important effect on inappropriate eating behaviors, which in turn lead to obesity. Davis et al. found that ADHD impulsive behaviors such as deficient inhibitory control and delay aversion were positively corre-lated with binge-eating and emotion-induced eat-ing (Davis et al. 2006; Lourenço et al. 2008). In contrast to our results, Davis et al. demonsrated that ADHD-related inattention and executive function deficits may cause obesity by disrupting a regular eating pattern (Davis et al.2006).
Several limitations of the study need to be con-sidered. Firstly, the assessment of chronotype pre-ference was only gathered from subjective parent/ self-report forms rather than objective measures (such as actigraphy). Other limitation is that the participants were obtained from outpatient clinics. This sample might not reflect the general popula-tion due to biases associated with treatment-seeking samples. Another limitation is that it is cross-sectional rather than longitudinal. Longitudinal studies can clearly demonstrate the relationship between ADHD, circadian preference and obesity.
In summary, we demonstrated that evening pre-ference was directly related to obesity and morn-ing preference was directly related to normal weight independently from ADHD symptoms in children and adolescents with ADHD. Our study also found that hyperactivity/impulsivity and ADHD index which are important for a global view on the severity of ADHD were related to BMI percentile. These findings might explain why at least a subgroup of child and adolescent obese patients might not do well with standard obesity treatment that does not consider sleep-wake cycles and ADHD pathology. We hope that future well-designed prospective studies can better explain the relationship between ADHD, obesity and chronotype.
Conflict of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
References
Adan A, Archer SN, Hidalgo MP, Di Milia L, Natale V,
Randler C. 2012. Circadian typology: a comprehensive
review. Chronobiol Int. 29:1153–1175.
Adan A, Fabbri M, Natale V, Prat G.2006. Sleep Beliefs Scale (SBS) and circadian typology. J Sleep Res. 15:125–132. Adan A, Lachica J, Caci H, Natale V.2010. Circadian
typol-ogy and temperament and character personality
dimensions. Chronobiol Int. 27:181–193.
Arble DM, Ramsey KM, Bass J, Turek FW. 2010. Circadian
disruption and metabolic disease: findings from animal models. Best Pract Res Clin Endocrinol Metab. 24:785–800. Arora T, Taheri S.2015. Associations among late chronotype,
body mass index and dietary behaviors in young adolescents. Int J Obes. 39:39.
Babkoff H, Caspy T, Hishikawa Y, Mikulincer M. 1991.
Subjective sleepiness ratings: the effects of sleep depriva-tion, circadian rhythmicity and cognitive performance. Sleep. 14:534–539.
Baird A, Coogan A, Siddiqui A, Donev R, Thome J. 2012.
Adult attention-deficit hyperactivity disorder is associated with alterations in circadian rhythms at the behavioural, endocrine and molecular levels. Mol Psychiatry. 17:988. Biederman J. 2005. Attention-deficit/hyperactivity disorder:
a selective overview. Biol Psychiatry. 57:1215–1220.
Chaput JP, Tremblay A. 2007. Does short sleep duration
favor abdominal adiposity in children? Int J Pediat Obesity. 2:188–191.
Collaborators GO. 2017. Health effects of overweight and
obesity in 195 countries over 25 years. N Engl J Med. 377:13–27.
Comings DE, Blum K. 2000. Reward deficiency syndrome:
genetic aspects of behavioral disorders. In HBM. Uylings, GG. van Eden, JPC. de Bruin, MGP. Feenstra, CMA. Pennartz (Eds.,), Progress in brain research. Elsevier. 126:3–499.
Conners CK, Sitarenios G, Parker JD, Epstein JN.1998. The
revised Conners’ Parent Rating Scale (CPRS-R): factor
structure, reliability, and criterion validity. J Abnorm Child Psychol. 26:257–268.
Coogan AN, McGowan NM. 2017. A systematic review of
circadian function, chronotype and chronotherapy in attention deficit hyperactivity disorder. ADHD Atten Defic Hyperact Disord. 9:129–147.
Cortese S, Faraone SV, Konofal E, Lecendreux M.2009. Sleep in children with attention-deficit/hyperactivity disorder: meta-analysis of subjective and objective studies. J Am Acad Child Adolesc Psychiatry. 48:894–908.
Cortese S, Isnard P, Frelut M, Michel G, Quantin L,
Guedeney A, Falissard B, Acquaviva E, Dalla
Bernardina B, Mouren M. 2007. Association between
symptoms of attention-deficit/hyperactivity disorder and bulimic behaviors in a clinical sample of severely obese adolescents. Int J Obes. 31:340.
Cortese S, Moreira-Maia CR, St. Fleur D, Morcillo-Pe
between ADHD and obesity: a systematic review and meta-analysis. Am J Psychiatry. 173:34–43.
Cortese S, Olazagasti MAR, Klein RG, Castellanos FX, Proal E, Mannuzza S.2013. Obesity in men with childhood ADHD: a 33-year controlled, prospective, follow-up study. Pediatrics.Peds. 131:e1731–e1738.
Cortese S, Vincenzi B.2012. Obesity and ADHD: clinical and neurobiological implications. Curr Top Behav Neurosci. 9:199–218.
Culnan E, Kloss JD, Grandner M.2013. A prospective study
of weight gain associated with chronotype among college freshmen. Chronobiol Int. 30:682–690.
Daniels SR, Arnett DK, Eckel RH, Gidding SS, Hayman LL, Kumanyika S, Robinson TN, Scott BJ, St. Jeor S,
Williams CL. 2005. Overweight in children and
adoles-cents: pathophysiology, consequences, prevention, and treatment. Circulation. 111:1999–2012.
Davis C, Levitan RD, Smith M, Tweed S, Curtis C. 2006.
Associations among overeating, overweight, and attention deficit/hyperactivity disorder: a structural equation model-ling approach. Eat Behav. 7:266–274.
Díaz-Morales JF.2007. Morning and evening-types:
explor-ing their personality styles. Pers Individ Dif. 43:769–778. Doshi JA, Hodgkins P, Kahle J, Sikirica V, Cangelosi MJ,
Setyawan J, Erder MH, Neumann PJ. 2012. Economic
impact of childhood and adult attention-deficit/hyperac-tivity disorder in the United States. J Am Acad Child Adolesc Psychiatry. 51(990–1002):e1002.
Durmuş FB, Arman AR, Ayaz AB.2017. Chronotype and its
relationship with sleep disorders in children with attention deficit hyperactivity disorder. Chronobiol Int. 34:886–894. Dursun OB, Ogutlu H, Esin IS.2015. Turkish validation and
adaptation of children’s chronotype questionnaire
(CCTQ). Eurasian J Med. 47:56.
Faraone SV, Biederman J, Mick E. 2006. The age-dependent
decline of attention deficit hyperactivity disorder: a meta-analysis of follow-up studies. Psychol Med. 36:159–165.
Fleig D, Randler C. 2009. Association between chronotype
and diet in adolescents based on food logs. Eat Behav. 10:115–118.
Fuemmeler BF, Østbye T, Yang C, McClernon FJ, Kollins SH. 2011. Association between attention-deficit/hyperactivity disorder symptoms and obesity and hypertension in early adulthood: a population-based study. Int J Obes. 35:852. Gökler B, Ünal F, Pehlivantürk B, Kültür EÇ, Akdemir D,
Taner Y. 2004. Reliability and validity of schedule for affective disorders and schizophrenia for school age children-present and lifetime version-Turkish Version (K-SADS-PL-T). Turk J Child Adolesc Ment Health. 11:109–116.
Gruber R, Fontil L, Bergmame L, Wiebe ST, Amsel R, Frenette S, Carrier J. 2012. Contributions of circadian tendencies and behavioral problems to sleep onset pro-blems of children with ADHD. BMC Psychiatry. 12:212. Heiligenstein E, Keeling RP.1995. Presentation of
unrecog-nized attention deficit hyperactivity disorder in college students. J Am Coll Health. 43:226–228.
Imeraj L, Sonuga-Barke E, Antrop I, Roeyers H, Wiersema R,
Bal S, Deboutte D. 2012. Altered circadian profiles in
attention-deficit/hyperactivity disorder: an integrative review and theoretical framework for future studies. Neurosci Biobehav Rev. 36:1897–1919.
Jeong SH, Yu J-C, Lee CH, Choi K-S, Choi J-E, Kim SH,
Joo E-J. 2014. Human CLOCK gene-associated attention
deficit hyperactivity disorder-related features in healthy adults: quantitative association study using Wender Utah Rating Scale. Eur Arch Psychiatry Clin Neurosci. 264:71–81.
Kaner S, Buyukozturk S, Iseri E. 2013. Conners parent
rating scale-revised short: turkish standardization study/ Conners anababa dereceleme olcegi-yenilenmis kisa: tur-kiye stardardizasyon calismasi. Arch Neuropsychiatry. 50:100–110.
Kaufman J, Birmaher B, Brent D, Rao U, Flynn C, Moreci P, Williamson D, Ryan N. 1997. Schedule for affective dis-orders and schizophrenia for school-age children-present and lifetime version (K-SADS-PL): initial reliability and validity data. J Am Acad Child Adolesc Psychiatry. 36:980–988.
Kissling C, Retz W, Wiemann S, Coogan AN, Clement RM, Hünnerkopf R, Conner AC, Freitag CM, Rösler M,
Thome J. 2008. A polymorphism at the 3′-untranslated
region of the CLOCK gene is associated with adult atten-tion-deficit hyperactivity disorder. Am J Med Genet Part B. 147:333–338.
Kooij J, Bijlenga D. 2014. High prevalence of self-reported photophobia in adult ADHD. Front Neurol. 5:256. Lourenço BH, Arthur T, Rodrigues MD, Guazzelli I,
Frazzatto E, Deram S, Nicolau CY, Halpern A,
Villares SM.2008. Binge eating symptoms, diet composi-tion and metabolic characteristics of obese children and adolescents. Appetite. 50:223–230.
Lucassen EA, Zhao X, Rother KI, Mattingly MS,
Courville AB, de Jonge L, Csako G, Cizza G, Group SES.
2013. Evening chronotype is associated with changes in
eating behavior, more sleep apnea, and increased stress hormones in short sleeping obese individuals. PLoS One. 8:e56519.
Matthews M, Nigg JT, Fair DA.2014. Attention deficit hyper-activity disorder. Curr Top Behav Neurosci. 16:235–266.
McClung CA. 2013. How might circadian rhythms control
mood? Let me count the ways. Biol Psychiatry. 74:242–249. Mota MC, Waterhouse J, De-Souza DA, Rossato LT, Silva CM, Araújo MBJ, Tufik S, de Mello MT,
Crispim CA.2016. Association between chronotype, food
intake and physical activity in medical residents.
Chronobiol Int. 33:730–739.
Must A.2003. Does overweight in childhood have an impact
on adult health? Nutr Rev. 61:139.
Nakade M, Takeuchi H, Kurotani M, Harada T.2009. Effects
of meal habits and alcohol/cigarette consumption on morningness-eveningness preference and sleep habits by Japanese female students aged 18–29. J Physiol Anthropol. 28:83–90.
Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, Mullany EC, Biryukov S, Abbafati C, Abera SF. 2014. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet. 384:766–781.
Nielsen T.2010. Nightmares associated with the eveningness chronotype. J Biol Rhythms. 25:53–62.
O’reardon JP, Ringel BL, Dinges DF, Allison KC, Rogers NL, Martino NS, Stunkard AJ.2004. Circadian eating and sleeping patterns in the night eating syndrome. Obes Res. 12:1789–1796.
Ong JC, Huang JS, Kuo TF, Manber R.2007. Characteristics
of insomniacs with self-reported morning and evening chronotypes. J Clin Sleep Med. 3:289–294.
Owens JA, Spirito A, McGuinn M.2000. The Children’s Sleep Habits Questionnaire (CSHQ): psychometric properties of a survey instrument for school-aged children. Sleep-New York-. 23:1043–1052.
Polanczyk G, De Lima MS, Horta BL, Biederman J,
Rohde LA. 2007. The worldwide prevalence of ADHD:
a systematic review and metaregression analysis. Am J Psychiatry. 164:942–948.
Ponzi D, Wilson MC, Maestripieri D.2014. Eveningness is
associated with higher risk-taking, independent of sex and personality. Psychol Rep. 115:932–947.
Ruiz-Lozano T, Vidal J, De Hollanda A, Canteras M,
Garaulet M, Izquierdo-Pulido M. 2016. Evening
chrono-type associates with obesity in severely obese subjects: interaction with CLOCK 3111T/C. Int J Obes. 40:1550. Rybak YE, McNeely HE, Mackenzie BE, Jain UR, Levitan RD.
2007. Seasonality and circadian preference in adult
attention-deficit/hyperactivity disorder: clinical and neu-ropsychological correlates. Compr Psychiatry. 48:562–571.
Schaal S, Peter M, Randler C. 2010.
Morningness-evening-ness and physical activity in adolescents. Int J Sport Exercise Psychol. 8:147–159.
Schmidt S, Randler C.2010. Morningness-eveningness and
eating disorders in a sample of adolescent girls. J Individ Differ. 31:38–45.
Schwartz BS, Bailey-Davis L, Bandeen-Roche K, Pollak J,
Hirsch AG, Nau C, Liu AY, Glass TA. 2014. Attention
deficit disorder, stimulant use, and childhood body mass
index trajectory. Pediatrics.Peds.133(4):668–676. doi:
10.1542/peds.2013-3427.
Selvi Y, Gulec M, Agargun MY, Besiroglu L. 2007. Mood
changes after sleep deprivation in morningness–evening-ness chronotypes in healthy individuals. J Sleep Res. 16:241–244.
Selvi Y, Kandeger A, Boysan M, Akbaba N, Sayin AA, Tekinarslan E, Koc BO, Uygur OF, Sar V.2017. The effects of individual biological rhythm differences on sleep qual-ity, daytime sleepiness, and dissociative experiences. Psychiatry Res. 256:243–248.
Van der Heijden KB, Smits MG, Someren EJV, Boudewijn Gunning W.2005. Idiopathic chronic sleep onset insomnia in attention-deficit/hyperactivity disorder: a circadian rhythm sleep disorder. Chronobiol Int. 22:559–570. Vgontzas AN, Bixler EO, Chrousos GP.2006. Obesity-related
sleepiness and fatigue: the role of the stress system and cytokines. Ann N Y Acad Sci. 1083:329–344.
Vogel SW, Bijlenga D, Tanke M, Bron TI, van der
Heijden KB, Swaab H, Beekman AT, Kooij JS. 2015.
Circadian rhythm disruption as a link between
Attention-Deficit/Hyperactivity Disorder and obesity? J Psychosom Res. 79:443–450.
Weinberg WA, Brumback RA. 1990. Primary disorder of
vigilance: a novel explanation of inattentiveness,
day-dreaming, boredom, restlessness, and sleepiness.
J Pediatr. 116:720–725.
Wennman H, Kronholm E, Partonen T, Peltonen M,
Vasankari T, Borodulin K. 2015. Evening typology and
morning tiredness associates with low leisure time physical activity and high sitting. Chronobiol Int. 32:1090–1100.
Wirz-Justice A. 2003. Chronobiology and mood disorders.
Dialogues Clin Neurosci. 5:315.
Xu X, Breen G, Chen C-K, Huang Y-S, Wu -Y-Y, Asherson P. 2010. Association study between a polymorphism at the 3ʹ-untranslated region of CLOCK gene and attention deficit hyperactivity disorder. Behav Brain Funct. 6:48.
Yu JH, Yun C-H, Ahn JH, Suh S, Cho HJ, Lee SK, Yoo HJ,
Seo JA, Kim SG, Choi KM. 2015. Evening chronotype is
associated with metabolic disorders and body composition
in middle-aged adults. J Clin Endocrinol Metab.
100:1494–1502.
Zhang R, Lahens NF, Ballance HI, Hughes ME, Hogenesch JB
(2014). A circadian gene expression atlas in mammals:
implications for biology and medicine. Proceedings of the
National Academy of Sciences (PNAS). 111