Full Terms & Conditions of access and use can be found at
https://www.tandfonline.com/action/journalInformation?journalCode=icbi20
Chronobiology International
The Journal of Biological and Medical Rhythm Research
ISSN: 0742-0528 (Print) 1525-6073 (Online) Journal homepage: https://www.tandfonline.com/loi/icbi20
The relationship between chronotype, sleep
disturbance, severity of fibromyalgia, and quality
of life in patients with fibromyalgia
Gözde Türkoğlu & Yavuz Selvi
To cite this article: Gözde Türkoğlu & Yavuz Selvi (2020) The relationship between chronotype,
sleep disturbance, severity of fibromyalgia, and quality of life in patients with fibromyalgia, Chronobiology International, 37:1, 68-81, DOI: 10.1080/07420528.2019.1684314
To link to this article: https://doi.org/10.1080/07420528.2019.1684314
Published online: 05 Nov 2019.
Submit your article to this journal
Article views: 327
View related articles
View Crossmark data
The relationship between chronotype, sleep disturbance, severity of
fibromyalgia, and quality of life in patients with fibromyalgia
Gözde Türkoğluaand Yavuz Selvib
aDepartment of Physical Medicine and Rehabilitation, Konya Training and Research Hospital, Konya, Turkey;bDepartment of Psychiatry,
Selcuk University Faculty of Medicine, Konya, Turkey
ABSTRACT
Patients with fibromyalgia (FM) report high levels of sleep disturbance and chronic diffuse muscu-loskeletal pain. These patients experience diminished quality of life (QoL) due to pain and other comorbidities. Chronotype preferences have been suggested as a potential factor connecting increased severity of FM, sleep disturbances, and poor overall QoL. The present study is the first study examining the possible association between chronotype preferences, sleep disturbance, sever-ity of FM, and QoL in patients with FM.
One hundred drug-free patients diagnosed with FM participated in this cross-sectional study. Of them, 79 (79%) were females and 21 (21%) were males. The mean age was 41.65 ± 9.17 years (range: 21–62 years). The severity of FM symptoms, chronotype preferences, and QoL was evaluated using the Fibromyalgia Impact Questionnaire (FIQ), Morningness-Eveningness Questionnaire (MEQ), and World Health Organization Questionnaire on Quality of Life: Short Form (WHOQOL-BREF). The participants’ anxiety/depressive symptoms and sleep problems were assessed using the Hospital Anxiety and Depression Scale (HADS) and Pittsburgh Sleep Quality Index (PSQI).
The participants were classified according to their MEQ scores as evening type (score: 16–41), neither type (score: 42–58), and morning type (score: 59–86). It was found that there were significant differences in the FIQ score between the three groups (p < .001). It was determined that the total PSQI score was significantly higher in the evening type than the other two types (p < .05). It was found that there were significant differences in the general health, physical health, psychological, and environmental domain scores of the WHOQOL-BREF between the three groups (p < .05). It was detected that there were significant correlations between MEQ scores, WHOQOL-BREF subscale scores, FIQ scores, HADS-A and HADS-D scores, and PSQI scores. According to hierarchical regression analysis, eveningness preference explained an additional 21.9% of the variation in FM severity, thereby causing a statistically significant change in R-squared.
Our results indicated that eveningness preference was directly related to increased FM symp-tom severity and poorer QoL. Based on these findings, neglecting to take chronotype preference into account may not result in optimal response to standard treatment for some patients with FM.
ARTICLE HISTORY Received 22 July 2019 Revised 14 October 2019 Accepted 21 October 2019 KEYWORDS Fibromyalgia; chronotype; evening type; sleep disturbance; quality of life
Introduction
Fibromyalgia (FM) syndrome is a chronic musculos-keletal pain condition characterized by decreased pressure pain thresholds with hyperalgesia and allo-dynia (Andrade et al. 2019). Besides chronic wide-spread pain, other commonly reported symptoms include prominent fatigue, sleep problems, functional impairment, cognitive dysfunction, mood distur-bances, stiffness, interstitial cystitis/painful bladder syndrome, endometriosis, and gastrointestinal symp-toms (such as diarrhea and constipation) (Choy2015; Aaron and Buchwald2001). FM is seen in 3–6% of the
general population and often affects women (90%), with a female:male ratio of 6–10:1 (Gonzalez et al.
2015). Genetic predisposition, central sensitization, environmental factors, psychosocial variables, physi-cal stress, neuroendocrine functions, and immune factors are emphasized in the etiology of FM. Various factors including accidents (such as traffic or workplace injuries, fractures, polytraumatisms), med-ical interventions and complications (such as surgeries or infections, emotional trauma, stressful life events), and increased body mass index due to inactive life-styles seem to play a role in susceptibility to FM (Albrecht and Rice 2016; Low and Schweinhardt
CONTACTGözde Türkoğlu drgozdet@gmail.com Department of Physical Medicine and Rehabilitation, Konya Training and Research Hospital, Konya 42040, Turkey
Color versions of one or more of the figures in the article can be found online atwww.tandfonline.com/icbi.
https://doi.org/10.1080/07420528.2019.1684314
2012; Mork et al. 2010; Raphael et al. 2006). Psychological disorders (such as obsessive-compulsive personality disorder), histrionic personal-ity disorder (Uguz et al. 2010), avoidant personality disorder (Fu et al. 2015), borderline personality dis-order (Alciati et al.2012a), personality traits (such as neuroticism, psychoticism, perfectionism) (Montoro and Del Paso2015), alexithymia (Castelli et al.2012), and type-D personality (van Middendorp et al.2016) have also been implicated. The most recent models of the pathophysiology of FM are based on the concept of central sensitization to pain and the presumption that mechanisms suppressing endogenous pain are some-how impaired. The term“central” here refers to the central nervous system origins of hyperalgesia and allodynia (de la Coba et al.2018,2017). In FM, affec-tive dysregulation, which is a conceptualization repre-senting the mechanism of central sensitization, disrupts the perception of pain intensity (Ablin et al.
2008). It is a complex and multifactorial syndrome that is difficult to diagnose due to its indeterminate etiopathogenesis (Bellato et al.2012; Fitzcharles and Yunus2012). Currently, FM has no cure, but is treated with medication, cognitive behavioral therapy, and physical activity for symptom management (Nüesch et al.2013).
The most widely reported psychiatric disorders associated with FM are anxiety disorders, depres-sion, and sleep disorders, with lifetime prevalence rates of 11.6–32.2%, 29–70%, and >90%, respec-tively (Thieme et al. 2004; Bigatti et al. 2008; Alciati et al. 2012b; Diaz-Piedra et al. 2015). Some studies have indicated that mental disor-ders and sleep disturbances correlate with wor-sening symptoms such as pain severity, the number of tender points, and QoL (Hamilton et al. 2008; Lentz et al.1999; Plazier et al. 2015). Typical alterations in sleep patterns suggest that pain is affected by dysregulations of the auto-nomic and neuroendocrine systems (Jahan et al.
2012). Yunus et al. (1991) found that sleep dis-turbances correlated with increased pain sensitiv-ity, decreased physical functioning, and consequent affective disorders. Some studies have demonstrated that increased pain sensitivity and lower pain thresholds are associated with sleep deprivation or disruption (Onen et al.
2001; Roehrs et al. 2006; Smith et al. 2007). Other studies have shown that sleep quantity
and quality are related to the fact that how pain affects fatigue and depression (Hamilton et al.
2008; Nicassio et al. 2002). The relationship between the risk of developing FM and poor sleep quality has been investigated in two epide-miological studies. Mork and Nilsen (2012) found a dose-dependent association between the devel-opment of FM and poor sleep quality in 12,350 women. However, this study had a notable limita-tion, such as the fact that risk factors other than sleep could not be evaluated. In another study, all of age, baseline pain status, anxiety, physical health-related quality of life, cognitive impair-ment, and nonrestorative sleep correlated with the development of widespread pain in FM patients, but the results of multivariate analyses indicated that nonrestorative sleep was the stron-gest predictor of the subsequent development of widespread pain (Wolfe 2012). For these reasons, chronotype preferences, which have a significant impact on sleep quality, should also be evaluated (de Coo et al. 2019; Sun et al. 2019).
There is a cyclic rhythm in a number of hormonal, physiological, psychological, and behavioral pro-cesses of living organisms. In humans, all of sleep– wake cycles, hormone levels, body temperature, cog-nition, and affect vary based on the circadian rhythm. Factors affecting the sleep-wake cycle may be endogenous (e.g., circadian pacemaker) and/or exogenous (e.g., working hours, social activities). Individual differences in chronotype (such as morn-ing type or evenmorn-ing type) are related to numerous psychological, behavioral, and biological variables (including meal time, performance, mood, alertness, appetite, body temperature, and cortisol/melatonin secretion). For example, evening types report later bedtimes and waking times than morning types (Mongrain et al. 2006). Morning types also exhibit less variability in their bedtimes and wake times than evening types (Kudielka et al. 2006). In addition, evening types feel sleepy more often during the day-time (Ong et al.2007) and have more irregular sleep-wake habits (Barclay et al. 2010) when compared with morning types. Evening types also awaken more frequently than morning types due to night-mares, resulting in shorter total sleep time (Korczak et al.2008). These findings thus indicate that even-ingness preference is associated with sleep distur-bances and other sleep-related problems.
To date, there has been scarcely any focus on the relationship between chronotype preferences, sleep disturbance, severity of FM, and QoL in the litera-ture. Therefore, the present study aimed to examine the direct effects of chronotype on sleep, FM severity, and QoL.
Materials and methods
Subjects and study design
One hundred individuals with FM between the ages of 18–65 participated in this cross-sectional study. This study was conducted in the Physical Medicine and Rehabilitation Clinic of Konya Training and Research Hospital in Turkey and was approved by the Local Ethics Committee of Selcuk University. Patients who consented to par-ticipate in the study were newly diagnosed with FM and untreated. According to the new diag-nostic criteria developed by the American College of Rheumatology in 2010, individuals with FM participating in research studies must be 18 years or older and diagnosed. Those with medical conditions known to contribute to FM sympto-molgy (e.g., thyroid disease, inflammatory arthri-tis, systemic lupus erythematosus, rheumatoid arthritis, myositis, vasculitis, or Sjogren’s syn-drome) were excluded from the study. In addi-tion, those with comorbid psychiatric disorders (e.g., neurodevelopmental disorders, psychosis, depression, generalized anxiety disorder, or sub-stance abuse) were excluded from the study. The Sociodemographic Data Collection Form, Morningness-Eveningness Questionnaire (MEQ), Fibromyalgia Impact Questionnaire (FIQ), Pittsburgh Sleep Quality Index (PSQI), Hospital Anxiety and Depression Scale (HADS), and World Health Organization Questionnaire on Quality of Life: Short Form (WHOQOL-BREF) were used to assess the study participants.
Morningness-eveningness questionnaire (MEQ)
It is the most widely used scale for evaluating chron-otype preference (Horne and Östberg 1976) and consists of 19 self-report items. The total score ranges from 16 to 86, with higher scores indicating stronger morning preference. Scores can also be
divided into five categories of chronotypes: definite evening type, 16–30; moderate evening type, 31–41; neither type, 42–58; moderate morning type, 59–69; and definite morning type, 70–86. The validity and reliability study of the Turkish version of the scale was performed by Agargun et al. (2007). The Cronbach’s alpha coefficient was 0.81 for overall items. The test–retest reliability of composite scores was high (r = 0.95).
Fibromyalgia Impact Questionnaire (FIQ)
It was developed by Burckhardt et al. (1991) and is the most commonly used scale for assessing functional status in patients with FM. It includes 10 different characteristics: physical functioning, well-being, missed days of work, work difficulty, pain, fatigue, morning tiredness, stiffness, anxiety, and depression. The total score ranges from 0 to 100. While an average individual with FM scores 50 points, an individual who is more severely affected usually scores 70 and above (Sarmer et al. 2000). The Cronbach’s alpha
coefficient was 0.73 for overall items.
Pittsburgh Sleep Quality Index (PSQI)
It is the most widely used scale for evaluating subjec-tive sleep quality over the previous month. It consists of 19 self-report items that are grouped into seven components. These seven components are subjective sleep quality, habitual sleep efficiency, sleep latency, sleep duration, sleep disturbances, use of sleep medi-cation, and daytime dysfunction. Each item is weighted equally on a 0–3 scale: 0 = not during the past month, 1 = less than once a week, 2 = once or twice a week, and 3 = three or more times a week. Sleep quality is rated on a 0–3 scale: 0 = very good, 1 = fairly good, 2 = fairly bad, and 3 = very bad. The total score ranges from 0 to 21, with higher scores indicat-ing poor sleep quality. While a total PSQI score≤5 is considered indicative of good sleep quality, a total PSQI score >5 is considered indicative of poor sleep quality. The diagnostic specificity and sensitivity of the scale are, respectively, 0.86 and 0.89 (Buysse et al.
1989). Agargun et al. (1996) conducted the validity and reliability study of the Turkish version of the scale. In this study, the Cronbach’s alpha coefficient was calculated as 0.79.
Hospital anxiety and depression scale (HADS)
The participants’ anxiety and depression levels were assessed using the HADS (Zigmond and Snaith1983). It has two subscales: HADS-A (for anxiety) and HADS-D (for depression). Both subscales contain seven items rated on a 4-point scale (0–3). Total scores for each subscale range from 0 to 21. Higher scores indicate higher levels of anxiety/depression. The valid-ity and reliabilvalid-ity study of the Turkish version of the scale found that the cutoff point was 10 for the anxiety subscale and 7 for the depression subscale. Accordingly, those scoring above these cutoff points are considered as risk groups. The Turkish version was assessed for validation and reliability by Aydemir et al. (1997). In this study, the Cronbach’s alpha coefficient
was calculated as 0.85 for the anxiety subscale and 0.77 for the depression subscale.
World Health Organization Questionnaire on Quality of Life: Short Form (WHOQOL-BREF)
It was developed as a short version of the WHOQOL-100 to minimize the burden of partici-pants for some clinical trials. It includes 27 self-report items. The validity and reliability study of the Turkish version of the scale was conducted by Eser et al. (1999). It addresses five dimensions of QoL: general health, social relationships, physical health, psychological well-being, and environment. Each item is rated on a 5-point Likert scale. All five dimensions (general health, social relationships, physical health, psychological well-being, and envir-onment) are transformed to lie between 0 and 100. There is no cutoff value. Higher scores indicate bet-ter QoL. In this study, the Cronbach’s alpha coeffi-cient was calculated as 0.83 for the physical domain, as 0.66 for the psychological domain, as 0.53 for the social domain, as 0.73 for the environmental domain and as 0.73 for the national environmental domain, respectively.
Statistical analysis
Statistical analysis was performed with IBM SPSS Statistics for Windows Version 22.0 (SPSS Inc; Chicago, IL, USA). All variables were normally dis-tributed. The participants’ demographic and clinical characteristics were reported using the One-Way
Analysis of Variance (ANOVA) for numerical vari-ables and the Chi-square test for categorical varivari-ables. The ANOVA and Tukey’s post hoc test were used to evaluate differences (MEQ, FIQ, WHOQOL-BREF, PSQI, HADS) between groups in terms of chronotype preference. The relationships between psychological test scores and clinical variables were analyzed using the Pearson and partial correlation coefficients. In order to assess the contribution of eveningness pre-ference to FM symptoms, the hierarchical regression model was applied after controlling for some variables (age, HADS-A, HADS-D, and PSQI). Statistical sig-nificance was set atp-value less than 0.05.
Results
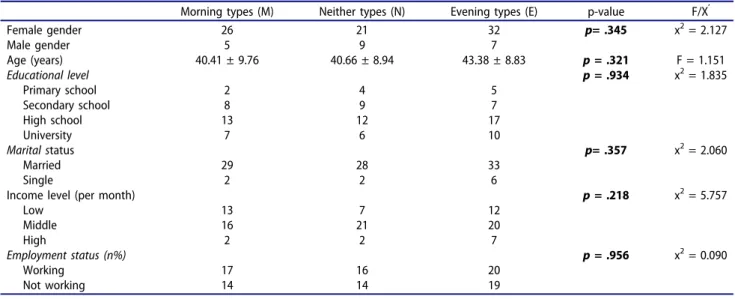
One hundred drug-free patients diagnosed with FM participated in this cross-sectional study. Of them, 79 (79%) were females and 21 (21%) were males. The mean age was 41.65 ± 9.17 years (range: 21–62 years) (Table 1). For the analysis of differences between chronotypes, moderate evening type and definite evening type were grouped together under evening type, while moderate morning type and definite morning type were grouped together under morning type. Then, the participants were divided into three groups based on MEQ scores: evening type (scores ranging from 16 to 41), neither type (scores ranging from 42 to 58), and morning type (scores ranging from 59 to 86). No significant differences were found between the three groups in terms of age, gender, educational level, or socioeconomic level (p> .05). There were 39 (39%) evening types, 30 (30%) neither types, and 31 (31%) morning types in this study.
It was found that there were significant differences in the FIQ score between the three groups (F(2, 97) = 51.13, p < .001). The mean FIQ score was 79.12 ± 9.17 in evening types, 62.30 ± 10.96 in neither types, and 48.13 ± 17.55 in morning types, respectively (Figure 1). Post hoc analyses revealed that there were significant differences in the FIQ score between evening types/morning types (p < .001), between evening types/neither types (p < .001), and between morning types/neither types (p < .001).
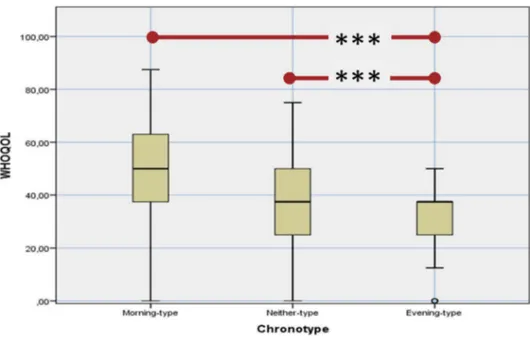
The general health (F(2, 97) = 11.93, p < .001), physical health (F(2, 97) = 20.17,p < .001), psycho-logical (F(2, 97) = 17.64,p < .001) and environmental (F(2, 97) = 7.37, p = .001) domain scores of the WHOQOL-BREF showed significant differences
between the three groups. The social relationship domain score of the WHOQOL-BREF did not exhi-bit significant differences between the three groups (F(2, 97) = 2.76,p = .067). Post hoc analyses revealed that there were significant differences in the WHOQOL-BREF subdomain scores between eve-ning types/moreve-ning types and between eveeve-ning types/neither types (p < .001), but not between neither types/morning types (p > .05) (Figure 2).
It was found that there were significant differ-ences in the HADS-A (F(2, 97) = 9.37, p < .001) and HADS-D (F(2, 97) = 11.60, p < .001) scores
between the three groups. However, post hoc ana-lyses revealed that there were significant differ-ences in the HADS-A and HADS-D scores between evening types/morning types and between evening types/neither types (p < .05), but not between neither types/morning types (p > .05) (Table 2).
The total PSQI score showed significant differ-ences between the three groups (F(2, 97) = 6.21, p < .01). However, post hoc analyses revealed that there were significant differences in the total PSQI score between evening types/morning types and
Table 1.Comparison of descriptive statistics between chronotype preferences (analysis of variance and chi-square test).
Morning types (M) Neither types (N) Evening types (E) p-value F/X’ Female gender Male gender 26 5 21 9 32 7 p= .345 x2= 2.127 Age (years) 40.41 ± 9.76 40.66 ± 8.94 43.38 ± 8.83 p= .321 F = 1.151 Educational level Primary school Secondary school High school University 2 8 13 7 4 9 12 6 5 7 17 10 p= .934 x2= 1.835 Marital status Married Single 29 2 28 2 33 6 p= .357 x2= 2.060 Income level (per month)
Low Middle High 13 16 2 7 21 2 12 20 7 p= .218 x2= 5.757 Employment status (n%) Working Not working 17 14 16 14 20 19 p= .956 x2= 0.090
between evening types/neither types (p < .05), but not between neither types/morning types (p > .05).
While a total PSQI score ≤5 is considered indica-tive of good sleep quality, a total PSQI score >5 is considered indicative of poor sleep quality. It was found that there were significant differences between the three groups in terms of sleep quality (p < .05). The rate of those with poor sleep quality according to the total PSQI score was 61.2% in morning types, 93.3% in neither types, and 97.4% in evening types, respectively. However, post hoc analyses revealed that there were significant differences between evening
types/morning types and between neither types/ morning types (p < .05), but not between evening types/neither types (p > .05) (Table 3). The subjective sleep quality (F(2, 97) = 35.77,p < .001), habitual sleep efficiency (F(2, 97) = 5.43,p < .01), sleep duration (F (2, 97) = 5.27,p < .01) and daytime dysfunction (F(2, 97) = 19.45, p < .001) domain scores of the PSQI showed significant differences between the three groups. Post hoc analyses revealed that there remained significant differences in the subjective sleep quality and daytime dysfunction domain scores of the PSQI between the three groups (p < .05). It was
Figure 2.Comparison of WHOQOL-BREF/General Health scores according to chronotype preferences.
Table 2.Comparison of FIQ, WHOQOL and HADS scores between chronotype preferences (analysis of variance).
Morning- types (M) Neither- types (N) Evening- types (E) p-value F-value
Post-hoc analysis FIQ 48.13 ± 17.55 62.30 ± 10.96 79.12 ± 9.17 p< .001 F = 51.13 E > N > M WHOQOL-BREEF WHOQOL-GH WHOQOL-P WHOQOL-PH WHOQOL-E WHOQOL-SR 52.09 ± 23.16 61.40 ± 14.82 56.27 ± 18.28 66.84 ± 12.48 56.79 ± 17.13 49.05 ± 20.48 62.09 ± 16.03 60.06 ± 19.39 66.27 ± 15.09 60.45 ± 16.65 32.01 ± 16.06 44.41 ± 15.46 37.02 ± 16.28 55.79 ± 15.31 51.32 ± 22.21 p< .001 p< .001 p< .001 p= .001 p= .067 F = 11.93 F = 17.64 F = 20.17 F = 7.37 F = 2.76 E < N = M E < N = M E < N = M E < N = M E = N = M HADS HADS-A HADS-D 9.02 ± 3.91 6.47 ± 3.71 7.88 ± 4.34 5.92 ± 3.31 11.73 ± 4.59 9.36 ± 3.78 p< .001 p< .001 F = 9.37 F = 11.60 E > N = M E > N = M WHOQOL-GH: World Health Organization Questionnaire on Quality of Life-General Health, WHOQOL-P: World Health Organization Questionnaire on
Quality of Life-Psychological, WHOQOL-PH: World Health Organization Questionnaire on Quality of Life-Physical Health, WHOQOL-E: World Health Organization Questionnaire on Quality of Life-Environment WHOQOL-SR: World Health Organization Questionnaire on Quality of Life-Social Relationships, HADS-A: Hospital Anxiety and Depression Scale-Anxiety, HADS-D: Hospital Anxiety and Depression Scale-Depression, FIQ: Fibromyalgia Impact Questionnaire, MEQ: Morningness-Eveningness Questionnaire.
Table 3. Comparison of PSQI total and subdomain scores between chronotype preferences (analysis of variance and chi-square test). Morning-types (M) Neither-types (N) Evening-types (E) p-value F/X 2 Post-hoc anaalysis PSQI Total Score 7.91 ± 4.33 7.50 ± 3.60 10.21 ± 3.73 p < 0.01 F = 6.21 E>N=M PSQI p < 0.001 x 2 = 20.03 E=N< M Good Sleep Qual ıty (Score ≤ 5) 12 2 1 Poor Sleep Qual ıty (score > 5) 19 28 38 PSQI Subjective Sleep Quality 0.80 ± 0.90 1.30 ± 0.70 2.23 ± 0.53 p < 0.001 F = 35.76 E>N>M Habitual Sleep Efficiency Sleep Latency 1.29 ± 0.97 1.53 ± 0.57 1.94 ± 0.91 p < 0.01 F = 5.43 E>M, E=N, M=N Latency 1.61 ± 1.02 1.46 ± 0.81 1.20 ± 0.86 p = 0.16 F = 1.84 E=N=M Sleep Duration 1.67 ± 1.01 1.56 ± 0.56 1.07 ± 0.83 p < 0.01 F = 5.27 E< N=M Sleep Disturbances 1.12 ± 0.84 1.33 ± 0.75 1.35 ± 0.81 p = 0.45 F = 0.79 E=N=M Use Of Sleep Medications 0.77 ± 0.88 0.76 ± 0.81 0.64 ± 0.74 p = 0.73 F = 0.30 E=N=M Daytime Dysfunction 0.90 ± 0.83 1.40 ± 0.77 2.05 ± 0.72 p < 0.001 F = 19.45 E>N>M
found that there were significant differences in the sleep duration domain score of the PSQI between evening types/morning types (p < .01) and between evening types/neither types (p < .05), but not between morning types/neither types (p > .05). It was found that there were significant differences in the habitual sleep efficiency domain score of the PSQI between only evening types/morning types (p < .05).
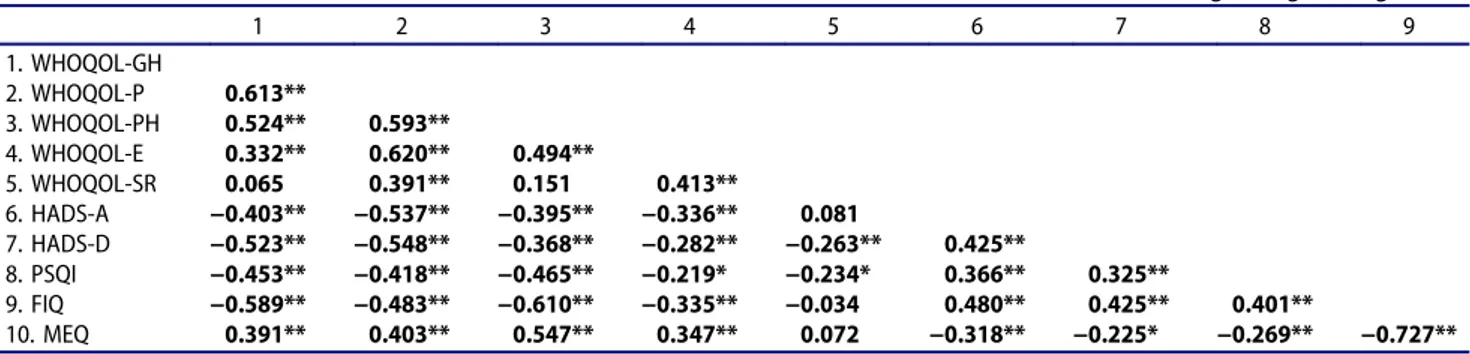
The relationships between the MEQ score and the FIQ, PSQI, HADS-A, HADS-D, and WHOQOL-BREF subscale scores were analyzed using the Pearson correlation coefficient. A negative correlation was found between the MEQ score and all other scale scores (except for the social relationship domain score of the WHOQOL-BREF).Table 4shows the results of the Pearson correlation analysis. Similarly, partial cor-relation analyses (controlling for age and gender) demonstrated a significant relationship (Table 5).
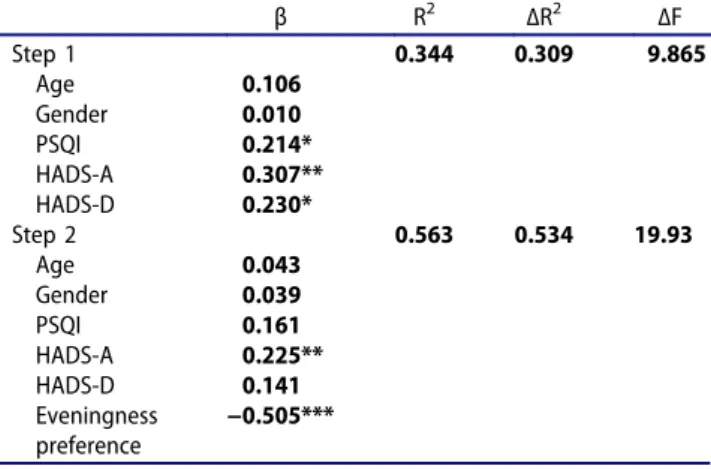
Hierarchical multiple regression analysis was performed in order to test our hypothesis regarding the FIQ score and chronotype preference. The vari-able ‘FIQ’, which indicates the severity of FM, was selected as a dependent variable. The independent variables (age, gender, HADS-A, HADS-D, and PSQI) were entered in the first step of regression analysis, while eveningness preference was added in the second step of regression analysis. The results of the regression analysis are presented in Table 6.
The first step of regression analysis revealed statistical significance (F = 9.86, p < .001). The control variables accounted for 34.4% (R-squared) of the variation in the FIQ. The HADS-A, HADS-D, and PSQI scores were statis-tically significant and positively associated with the FIQ score in the first step of regression analysis. Eveningness preference, which was added in
Table 4.Pearson’s correlation coefficients between age, WHOQOL, HADS, PSQI, FIQ, and MEQ scores.
1 2 3 4 5 6 7 8 9 10 1. Age 2. WHOQOL-GH −0.156 3. WHOQOL-P −0.129 0.621** 4. WHOQOL-PH 0.011 0.516** 0.632** 5. WHOQOL-E 0.009 0.403** 0.627** 0.507** 6. WHOQOL-SR −0.145 0.081 0.384** 0.169 0.386** 7. HADS-A −0.126 −0.354** −0.511** −0.372** −0.328** −0.098 8. HADS-D 0.198* −0.471** −.0569** −.0346** −0.353** −.0301** 0.379** 9. PSQI 0.038 −0.456** −0.391** −0.433** −0.240* −0.169 0.301** 0.325** 10. FIQ 0.173 −0.595** −0.534** −0.601** −0.324** −0.067 0.435** 0.403** 0.416** 11. MEQ −0.226* 0.416** 0.414** 0.526** 0.295** 0.073 −0.284** −0.247* −0.288** −0.718** * p < 0.05; ** p < 0.01
WHOQOL-GH: World Health Organization Questionnaire on Quality of Life-General Health, WHOQOL-P: World Health Organization Questionnaire on Quality of Life-Psychological, WHOQOL-PH: World Health Organization Questionnaire on Quality of Life-Physical Health, WHOQOL-E: World Health Organization Questionnaire on Quality of Life-Environment WHOQOL-SR: World Health Organization Questionnaire on Quality of Life-Social Relationships, HADS-A: Hospital Anxiety and Depression Scale-Anxiety, HADS-D: Hospital Anxiety and Depression Scale-Depression, PSQI: Pittsburgh Sleep Quality Index, FIQ: Fibromyalgia Impact Questionnaire, MEQ: Morningness-Eveningness Questionnaire.
Table 5.Partial correlation coefficients between WHOQOL, HADS, PSQI, FIQ and MEQ scores after controlling for age and gender.
1 2 3 4 5 6 7 8 9 1. WHOQOL-GH 2. WHOQOL-P 0.613** 3. WHOQOL-PH 0.524** 0.593** 4. WHOQOL-E 0.332** 0.620** 0.494** 5. WHOQOL-SR 0.065 0.391** 0.151 0.413** 6. HADS-A −0.403** −0.537** −0.395** −0.336** 0.081 7. HADS-D −0.523** −0.548** −0.368** −0.282** −0.263** 0.425** 8. PSQI −0.453** −0.418** −0.465** −0.219* −0.234* 0.366** 0.325** 9. FIQ −0.589** −0.483** −0.610** −0.335** −0.034 0.480** 0.425** 0.401** 10. MEQ 0.391** 0.403** 0.547** 0.347** 0.072 −0.318** −0.225* −0.269** −0.727** * p < 0.05; ** p < 0.01
WHOQOL-GH: World Health Organization Questionnaire on Quality of Life-General Health, WHOQOL-P: World Health Organization Questionnaire on Quality of Life-Psychological, WHOQOL-PH: World Health Organization Questionnaire on Quality of Life-Physical Health, WHOQOL-E: World Health Organization Questionnaire on Quality of Life-Environment WHOQOL-SR: World Health Organization Questionnaire on Quality of Life-Social Relationships, HADS-A: Hospital Anxiety and Depression Scale-Anxiety, HADS-D: Hospital Anxiety and Depression Scale-Depression, PSQI: Pittsburgh Sleep Quality Index, FIQ: Fibromyalgia Impact Questionnaire, MEQ: Morningness-Eveningness Questionnaire.
the second step of regression analysis, explained an additional 21.9% of the variation in FM severity, thereby causing a statistically significant change in R-squared (F = 19.93,p < .001). Thus, our hypoth-esis is supported by the results of regression ana-lysis, which showed that eveningness preference predicted the severity of FM. The second step of regression analysis revealed statistical significance. The control variables accounted for 56.3% of the variation in the FIQ.
Discussion
In this study, individuals with FM were grouped according to their chronotype preferences and assessed with regard to FM severity and chronotype. The relationships between factors affecting FM severity and QoL in the participating patients were then investigated. The present study is the first study examining the possible association between chrono-type preferences, sleep disturbance, severity of FM, and QoL in patients with FM. Our results showed a strong association between eveningness preference and increased severity of FM and poor QoL.
FM may impair physical, psychological, and social functioning and adversely affect social rela-tionships, personal and professional life, daily life activities, and mental health. These negative effects are not only caused by the pain associated with FM but also by fatigue, cognitive deficits, and other symptoms of FM (Karper 2016; RPdA et al. 2017). Chronotype and related
psychological, behavioral, and social problems may influence the severity of FM and complicate its treatment. Studies conducted on chronotype preferences have found that morning types are more conscientious, exhibit a stronger internal locus of control, have healthier lifestyles, and report higher self-esteem compared with evening types (Jackson and Gerard 1996; Taillard et al.
2001). Other studies have demonstrated that morningness is associated with higher-order per-sonality factors, emotional stability, happiness, and positive affect (including constructs like ‘pride’), as well as social (agreeableness) and motivational (conscientiousness) traits (DeYoung et al. 2007; Drezno et al. 2019; Murray et al. 2009). Drezno et al. (2019) have suggested that conscientiousness and emotional stability traits would mediate the relationship between morningness and life satisfaction. Furthermore, they have indicated that extraver-sion would moderate the association between chronotype and satisfaction (Drezno et al. 2019). They have also reported that morningness-eveningness and standard personality traits are associated with well-being but few studies have directly compared the two types of construct as correlates of life satisfaction, and that all these differences in personality traits between these types will of course change the effect of FM on perceived symptom severity and QoL in indivi-duals with FM. In addition, morning types per-form daily life activities more regularly and exhibit greater uniformity in their routines, social rhythms, and eating behaviors compared with evening types (Monk et al. 2004). Another factor associated with chronotype preference is exercise. This is important because sports activity/exercise is one of the most powerful factors that can reduce the symptoms of FM including better pain modulation (Andrade et al. 2019; Ellingson et al. 2012), better sleep quality, better QoL (Andrade et al. 2019), better mood/life satisfac-tion (Andrade et al. 2017), and better overall health (Larsson et al. 2014). Some studies have shown that morning types exercise more fre-quently and regularly than evening types (Hisler et al. 2017). Sławińska et al. (2019) brought a different perspective to this issue. This study demonstrated that intense physical exercise may
Table 6.The results of regression analysis.
β R2 ΔR2 ΔF Step 1 0.344 0.309 9.865 Age 0.106 Gender 0.010 PSQI 0.214* HADS-A 0.307** HADS-D 0.230* Step 2 0.563 0.534 19.93 Age 0.043 Gender 0.039 PSQI 0.161 HADS-A 0.225** HADS-D 0.141 Eveningness preference −0.505*** *p< 0.05; **p< 0.01; ***p< 0.001.
HADS-A: Hospital Anxiety and Depression Scale-Anxiety, HADS-D: Hospital Anxiety and Depression Scale-Depression, PSQI: Pittsburgh Sleep Quality Index, FIQ: Fibromyalgia Impact Questionnaire.
allow compensation for the negative effects of non-optimal time of day on experienced moods, particularly in the case of neither/evening-types (Sławińska et al. 2019). In this way, it has been shown that the time disadvantages of chronotype preferences can be eliminated by the exercise program. Other studies found that eveningness was correlated with poorer emotional adjustment (i.e., higher levels of depressive and anxiety symptoms), substance abuse, and irregular sleep-wake habits (Giannotti et al. 2002; Selvi et al.
2010). Urbán et al. (2011) demonstrated that eveningness preference was positively associated with health-impairing behaviors such as alcohol consumption, smoking, and watching television or playing computer games. Furthermore, the role of eveningness preference has been high-lighted in various health conditions, including hypertension (Bursztyn et al. 1994), obesity (Maukonen et al. 2016), dyslipidemia, and dia-betes mellitus (Ritonja et al. 2019). Accordingly, eveningness preference may be considered a risk factor for physical and psychological disorders. A number of factors associated with eveningness preference are correlated with the etiology and severity of FM. Our findings clearly showed that evening types exhibited significantly more severe FM symptoms and worse QoL than morning types and neither types. Especially, the second step of the hierarchical regression model in our study demonstrated that this effect was statisti-cally significant.
Similarly, Kantermann et al. (2012) showed that evening types were more affected by FM. In this study, evening types were more affected than morning types according to the sum scores of perceived stress, FM severity, fatigue, and depres-sion (Kantermann et al. 2012). For common pro-blems such as FM in which biopsychosocial factors are determinative, the evaluation of chronotype preferences is critical for the etiology and proper treatment of the disease.
Pain is the most important symptom in FM and is affected by many factors. The circadian rhythm is one of these factors. Diurnal and circadian var-iations in pain have been observed in pathological conditions such as FM (Junker and Wirz 2010). Morning types demonstrated a higher pain thresh-old during the day than evening types (Jankowski
2013). The present study showed that the mean FIQ score was significantly higher in the evening type than the other two types. Being more sensitive to pain may be one of the factors causing this condition. It is not true that pain hypersensitivity is evaluated separately from affective functioning. Emotional processing has a key role in pain per-ception (Shackman et al. 2011). Negative affective states are considered as a disadvantage in pain perception (Haukkal et al. 2011). In this respect, it can be again said that being an evening type is disadvantageous (DeYoung et al. 2007).
Sleep disturbances (especially nocturnal restless-ness, shorter sleep duration, frequent awakening, and nonrefreshing sleep) are common in patients with FM, affecting >90% of patients (Bigatti et al.
2008; Hauri and Hawkins 1973; Wu et al. 2017). The PSQI contains seven domains; however, only the total PSQI score can be used to distinguish poor sleepers from good sleepers, with a total PSQI score of >5 being a sensitive and specific measure of lower sleep quality (Buysse et al.
1989). Our study found that the mean total PSQI score was 10.21 in evening types, 7.50 in neither types, and 7.91 in morning types, respectively. Accordingly, our study showed that the rate of those with poor sleep quality according to the total PSQI score was lower in the morning type than the other two types. In both total and partial correlations, PSQI scores were also found to be negatively correlated with QoL scores and posi-tively correlated with FIQ scores. These results are very important because low sleep quality is a risk factor for FM (Choy 2015; Mork and Nilsen 2012), sleep quality is associated with many aspects of QoL (Milrad et al. 2017) and is strongly and dose dependently associated with symptom severity in FM patients, and there is a possibility that pain severity can be reduced by improving sleep quality (Clauw2014; Spaeth et al.
2011). Therefore, primary care providers should be informed about the findings of this study, should proactively assess the risk of sleep disturbance in patients with chronic diffuse pain, and should consider the diagnosis of FM in these patients. Clinicians should also actively treat sleep disorders when poor sleep is detected in FM patients.
FM, pain sensitivity, and circadian rhythm distur-bances may be linked to a shared genetic etiology.
Certain gene polymorphisms (particularly those that affect the serotoninergic, dopaminergic, and cate-cholaminergic systems) have been shown to possibly be implicated in the development and severity of FM (Park and Lee 2017). Individual variations in the aforementioned neurotransmitter systems are con-nected to the modulation of circadian rhythm (Murray 2019; Randler 2008). Another common etiology is central sensitization, which may also result in conditions other than FM (such as circadian rhythm disturbances, memory problems, and mood disorders), as pain and sensory sensitivity are likely to be controlled by the same neurotransmitters that also influence sleep, affect, and memory (Phillips and Clauw2013). Due to their common polygenic etiol-ogy, the treatment of circadian rhythm disturbances may also ameliorate FM symptoms; the converse is also true.
This study has several limitations that should be taken into consideration. First of all, chronotype preferences were evaluated by only self-report ques-tionnaires, not objective measures (such as actigra-phy and objective temperature measurements). The participants were recruited from outpatient clinics and therefore might not accurately represent the general population due to biases related to treat-ment-seeking samples. Another limitation is that this study has a cross-sectional design as opposed to longitudinal studies which would be able to more clearly show the relationship between chronotype preferences, QoL, and FM.
In conclusion, our results indicated that even-ingness preference was directly related to increased FM symptom severity and poorer QoL. We also found that eveningness preference was associated with poorer sleep quality and increased severity of anxiety/depressive symptoms. Thus, certain patients with FM might not respond optimally to standard treatment if their sleep-wake cycles are not taken into consideration. Future properly designed prospective studies should be able to deepen our understanding of the relationship between FM, chronotype preferences, and QoL.
Conflict of interest
The authors report no conflicts of interest. The authors alone are responsible for the content and writing of this article.
References
Aaron L A, Buchwald D.2001. A review of the evidence for
overlap among unexplained clinical conditions. Ann
Intern Med. 134:868–881. doi:
10.7326/0003-4819-134-9_part_2-200105011-00011. PMID: 11346323.
Ablin J, Neumann L, Buskila D.2008. Pathogenesis of
fibro-myalgia–a review. Joint Bone Spine. 75:273–279.
doi:10.1016/j.jbspin.2007.09.010. PMID: 18375167.
Agargun M, Kara H, Anlar Ö.1996. Validity and reliability of the Pittsburgh Sleep Quality Index in Turkish sample. Tur Psychiat. 7:107–155.
Agargun MY, Cilli AS, Boysan M, Selvi Y, Gulec M, Kara H.
2007. Turkish version of morningness-eveningness
ques-tionnaire (MEQ). Sleep Hypn. 9:16–23.
Albrecht PJ, Rice FL.2016. Fibromyalgia syndrome pathology and environmental influences on afflictions with medically
unexplained symptoms. Rev Environ Health. 31:281–294.
doi:10.1515/reveh-2015-0040. PMID: 27105483.
Alciati A, Sarzi-Puttini P, Batticciotto A, Torta R, Gesuele F, Atzeni F, Angst J.2012a. Overactive lifestyle in patients with fibromyalgia as a core feature of bipolar spectrum disorder.
Clin Exp Rheumatol. 30:122–128. PMID: 23261011.
Alciati A, Sgiarovello P, Atzeni F, Sarzi-Puttini P. 2012b. Psychiatric problems in fibromyalgia: clinical and neuro-biological links between mood disorders and fibromyalgia.
Reumatismo. 64:268–274. doi:
10.4081/reuma-tismo.2012.268. PMID: 23024971.
Andrade A, Sieczkowska SM, Vilarino GT. 2019. Resistance
training improves quality of life and associated factors in patients with fibromyalgia syndrome. PM&R. 11:703–709.
doi:10.1016/j.pmrj.2018.09.032. PMID: 30266345.
Andrade A, Steffens R, Vilarino GT, Sieczkowska SM,
Coimbra DR. 2017. Does volume of physical exercise
have an effect on depression in patients with
fibromyalgia? J Affect Disord. 208:214–217. doi:10.1016/j.
jad.2016.10.003. PMID: 27792965.
Aydemir Ö, Guvenir T, Kuey L, Kultur S.1997. Validity and reliability of Turkish version of hospital anxiety and depression scale. Turk Psikiyatri Derg. 8:280–287. Barclay NL, Eley TC, Buysse DJ, Archer SN, Gregory AM.
2010. Diurnal preference and sleep quality: same genes? A study of young adult twins. Chronobiol Int. 27:278–296.
doi:10.3109/07420521003663801. PMID: 20370470.
Bellato E, Marini E, Castoldi F, Barbasetti N, Mattei L,
Bonasia DE, Blonna D. 2012. Fibromyalgia syndrome:
etiology, pathogenesis, diagnosis, and treatment. Pain Res Treat:1–17. PMID: 23213512. doi:10.1155/2012/426130.
Bigatti SM, Hernandez AM, Cronan TA, Rand KL. 2008.
Sleep disturbances in fibromyalgia syndrome: relationship
to pain and depression. Arthritis Rheum. 59:961–967.
doi:10.1002/art.23828. PMID: 18576297.
Burckhardt CS, Clark SR, Bennett RM.1991. The
fibromyal-gia impact questionnaire: development and validation.
J Rheumatol. 18:728–733. PMID: 1865419.
Bursztyn M, Mekler J, Wachtel N, Ben-Ishay D.1994. Siesta and ambulatory blood pressure monitoring comparability
of the afternoon nap and night sleep. Am J of Hypertens. 7:217–221. doi:10.1093/ajh/7.3.217. PMID: 8003271. Buysse DJ, Reynolds III CF, Monk TH, Berman SR,
Kupfer DJ. 1989. The pittsburgh sleep quality index:
A new instrument for psychiatric practice and research.
Psychiatry Res. 28:193–213. doi:10.1016/0165-1781(89)
90047-4. PMID: 2748771.
Castelli L, Tesio V, Colonna F, Molinaro S, Leombruni P,
Bruzzone M, Fusaro E, Sarzi-Puttini P, Torta R. 2012.
Alexithymia and psychological distress in fibromyalgia: prevalence and relation with quality of life. Clin Exp Rheumatol. 30:70–77. PMID: 23110722.
Choy EH.2015. The role of sleep in pain and fibromyalgia. Nat Rev Rheumatol. 11:513–520. doi:10.1038/nrrheum.2015.56. PMID: 25907704.
Clauw DJ. 2014. Fibromyalgia: a clinical review. JAMA.
311:1547–1555. doi:10.1001/jama.2014.3266. PMID:
24737367.
de Coo IF, van Oosterhout WPJ, Wilbrink LA, van Zwet EW, Ferrari MD, Fronczek R.2019. Chronobiology and sleep in
cluster headache. Headache. 59:1032–1041. doi:10.1111/
head.13567. PMID: 31148161.
de la Coba P, Bruehl S, Galvez-Sánchez CM, Del Paso GAR. 2018. Slowly repeated evoked pain as a marker of central sensitization in fibromyalgia: diagnostic accuracy and reliability in comparison with temporal summation of
pain. Psychosom Med. 80:573–580. doi:10.1097/
PSY.0000000000000599. PMID: 29742751.
de la Coba P, Bruehl S, Moreno-Padilla M, Reyes Del Paso GA.2017. Responses to slowly repeated evoked pain stimuli in fibromyalgia patients: evidence of enhanced pain sensitization. Pain Med. 18:1778–1786. PMID: 28371909.
doi:10.1093/pm/pnw361.
DeYoung CG, Hasher L, Djikic M, Criger B, Peterson JB. 2007. Morning people are stable people: circadian rhythm and the higher-order factors of the big five. Pers Individ Dif. 43:267–276.
Diaz-Piedra C, Di Stasi LL, Baldwin CM, Buela-Casal G, Catena A.2015. Sleep disturbances of adult women suffer-ing from fibromyalgia: a systematic review of observational
studies. Sleep Med Rev. 21:86–99. doi:10.1016/j.
smrv.2014.09.001. PMID: 25456469.
Drezno M, Stolarski M, Matthews G.2019. An in-depth look
into the association between morningness-eveningness and well-being: evidence for mediating and moderating effects of personality. Chronobiol Int. 36:96–109. doi:10.1080/
07420528.2018.1523184. PMID: 30303401.
Ellingson LD, Shields MR, Stegner AJ, Cook DB. 2012.
Physical activity, sustained sedentary behavior, and pain
modulation in women with fibromyalgia. J Pain.
13:195–206. doi:10.1016/j.jpain.2011.11.001. PMID:
22245361.
Eser SY, Fidaner H, Fidaner C, Elbi H, Eser E, Göker E.1999. Psychometric properties of the WHOQOL-100 and WHOQOL-BREF. J Psychiatry Psychol Psychopharmacol. 7:23–40.
Fitzcharles M-A, Yunus MB. 2012. The clinical concept of
fibromyalgia as a changing paradigm in the past 20 years. Pain Res Treat. doi:10.1155/2012/184835. PMID: 22135738.
Fu T, Gamble H, Siddiqui U, Schwartz T.2015. Psychiatric
and personality disorder survey of patients with
fibromyalgia. Ann Dep Anxiety. 2:1064.
Giannotti F, Cortesi F, Sebastiani T, Ottaviano S. 2002.
Circadian preference, sleep and daytime behaviour in adolescence. J Sleep Res. 11:191–199. doi:
10.1046/j.1365-2869.2002.00302.x. PMID: 12220314.
Gonzalez JG, Del Teso Rubio M, Paniagua CNW, Criado-Alvarez JJ, Holgado JS.2015. Symptomatic pain and fibro-myalgia treatment through multidisciplinary approach for
primary care. Reumatol Clín. 11:22–26. doi:10.1016/j.
reuma.2014.03.005. PMID: 24837647.
Hamilton NA, Affleck G, Tennen H, Karlson C, Luxton D, Preacher KJ, Templin JL. 2008. Fibromyalgia: the role of sleep in affect and in negative event reactivity and recovery. Health Psychol. 27:490–497. doi:
10.1037/0278-6133.27.4.490. PMID: 18643007.
Haukkal E, Leino Arjasl P, Ojajärvil A, Takalal EP, Viikari Juntural E, Riihimäkil H.2011. Mental stress and psycho-social factors at work in relation to multiple site muscu-loskeletal pain: A longitudinal study of kitchen workers. Euro J Pain. 15:432–438. doi:10.1016/j.ejpain.2010.09.005. PMID: 20932789.
Hauri P, Hawkins DR. 1973. Alpha-delta sleep.
Electroencephalogr Clin Neurophysiol. 34:233–237.
doi:10.1016/0013-4694(73)90250-2. PMID: 4129610.
Hisler GC, Phillips AL, Krizan Z.2017. Individual differences in diurnal preference and time-of-exercise interact to pre-dict exercise frequency. Ann Behav Med. 51:391–401.
doi:10.1007/s12160-016-9862-0. PMID: 27909945.
Horne JA, Östberg O.1976. A self-assessment questionnaire to determine morningness-eveningness in human circa-dian rhythms. Int J of Chronobiol. 4:97–110. PMID: 1027738.
Jackson LA, Gerard DA. 1996. Diurnal types, the“Big Five” personality factors, and other personal characteristics. J Soc Behav and Pers. 11:273–283.
Jahan F, Nanji K, Qidwai W, Qasim R. 2012. Fibromyalgia
syndrome: an overview of pathophysiology, diagnosis and
management. Oman Med J. 27:192–195. doi:10.5001/
omj.2012.44. PMID: 22811766.
Jankowski K. 2013. Morning types are less sensitive to pain than evening types all day long. Eur J Pain. 17:1068–1073.
doi:10.1002/j.1532-2149.2012.00274.x. PMID: 23322641.
Junker U, Wirz S.2010. Chronobiology: influence of circadian rhythms on the therapy of severe pain. J Oncol Pharm Prac. 16:81–87. doi:10.1177/1078155209337665. PMID: 19541762.
Kantermann T, Theadom A, Roenneberg T, Cropley M.2012.
Fibromyalgia syndrome and chronotype: late chronotypes
are more affected. J Biol Rhythms. 27:176–179.
doi:10.1177/0748730411435999. PMID: 22476779.
Karper WB.2016. Effects of exercise, patient education, and resource support on women with fibromyalgia: an
extended long-term study. J Women Aging. 28:555–562.
doi:10.1080/08952841.2016.1223954. PMID: 27749200.
Korczak A, Martynhak B, Pedrazzoli M, Brito A, Louzada F.
2008. Influence of chronotype and social zeitgebers on
sleep/wake patterns. Braz J Med and Biol Res.
41:914–919. doi:10.1590/s0100-879x2008005000047.
PMID: 18982197.
Kudielka BM, Federenko IS, Hellhammer DH, Wüst S.2006.
Morningness and eveningness: the free cortisol rise after
awa-kening in “early birds” and “night owls”. Biol Psychol.
72:141–146. doi:10.1016/j.biopsycho.2005.08.003. PMID: 16236420.
Larsson A, Palstam A, Löfgren M, Ernberg M, Bjersing J, Bileviciute-Ljungar I, Gerdle B, Kosek E, Mannerkorpi K. 2014. FRI0563-HPR does resistance exercise improve phy-sical function, health status and pain in fibromyalgia? Ann Rheum Dis. 73:1199. doi:10.1136/annrheumdis-2014-eular.
4245. PMID: 22777332.
Lentz MJ, Landis CA, Rothermel J, Shaver JL.1999. Effects of selective slow wave sleep disruption on musculoskeletal pain and fatigue in middle aged women. J Rheumatol. 26:1586–1592. PMID: 10405949.
Low LA, Schweinhardt P.2012. Early life adversity as a risk factor for fibromyalgia in later life. Pain Res Treat:1–15. PMID: 22110940. doi:10.1155/2012/140832.
Maukonen M, Kanerva N, Partonen T, Kronholm E,
Konttinen H, Wennman H, Männistö S.2016. The
asso-ciations between chronotype, a healthy diet and obesity.
Chronobiol Int. 33:972–981. doi:10.1080/
07420528.2016.1183022. PMID: 27246115.
Milrad SF, Hall DL, Jutagir DR, Lattie EG, Ironson GH, Wohlgemuth W, Nunez MV, Garcia L, Czaja SJ, Perdomo DM.2017. Poor sleep quality is associated with greater circulating pro-inflammatory cytokines and sever-ity and frequency of chronic fatigue syndrome/myalgic
encephalomyelitis (CFS/ME) symptoms in women.
J Neuroimmunol. 303:43–50. PMID: 28038892.
doi:10.1016/j.jneuroim.2016.12.008.
Mongrain V, Carrier J, Dumont M.2006. Difference in sleep regulation between morning and evening circadian types as indexed by antero-posterior analyses of the sleep EEG.
Eur J Neurosci. 23:497–504. doi:
10.1111/j.1460-9568.2005.04561.x. PMID: 16420456.
Monk TH, Buysse DJ, Potts JM, DeGrazia JM, Kupfer DJ. 2004. Morningness-eveningness and lifestyle regularity. Chronobiol Int. 21:435–443. doi:10.1081/CBI-120038614. PMID: 15332448.
Montoro CI, Del Paso GAR.2015. Personality and fibromyal-gia: Relationships with clinical, emotional, and functional variables. Pers Individ Dif. 85:236–244.
Mork PJ, Nilsen TI.2012. Sleep problems and risk of fibro-myalgia: longitudinal data on an adult female population
in Norway. Arthritis Rheum. 64:281–284. doi:10.1002/
art.33346. PMID: 22081440.
Mork PJ, Vasseljen O, Nilsen TI.2010. Association between physical exercise, body mass index, and risk of fibromyal-gia: longitudinal data from the Norwegian Nord Trøndelag
Health Study. Arthritis Care Res. 62:611–617. doi:10.1002/
acr.20118. PMID: 20191480.
Murray G.2019. Circadian science and psychiatry: of planets,
proteins and persons. London (England): SAGE
Publications Sage UK.
Murray G, Nicholas CL, Kleiman J, Dwyer R, Carrington MJ, Allen NB, Trinder J.2009. Nature’s clocks and human mood: the circadian system modulates reward motivation. Emotion. 9:705–716. doi:10.1037/a0017080. PMID: 19803592.
Nicassio PM, Moxham EG, Schuman CE, Gevirtz RN.2002.
The contribution of pain, reported sleep quality, and depressive symptoms to fatigue in fibromyalgia. Pain.
100:271–279. doi:10.1016/s0304-3959(02)00300-7. PMID:
12467998.
Nüesch E, Häuser W, Bernardy K, Barth J, Jüni P. 2013.
Comparative efficacy of pharmacological and
non-pharmacological interventions in fibromyalgia
syn-drome: network meta-analysis. Ann Rheum Dis.
72:955–962. doi:10.1136/annrheumdis-2011-201249.
PMID: 22739992.
Onen SH, Alloui A, Gross A, Eschallier A, Dubray C.2001.
The effects of total sleep deprivation, selective sleep inter-ruption and sleep recovery on pain tolerance thresholds in healthy subjects. J Sleep Res. 10:35–42. doi:
10.1046/j.1365-2869.2001.00240.x. PMID: 11285053.
Ong JC, Huang JS, Kuo TF, Manber R.2007. Characteristics
of insomniacs with self-reported morning and evening chronotypes. J Clin Sleep Med. 3:289–294. PMID: 17561599.
Park D-J, Lee -S-S. 2017. New insights into the genetics of
fibromyalgia. Korean J Intern Med. 32:984–995.
doi:10.3904/kjim.2016.207. PMID: 29056037.
Phillips K, Clauw DJ.2013. Central pain mechanisms in the rheumatic diseases: future directions. Arthritis Rheum. 65:291–302. doi:10.1002/art.37739. PMID: 23045168. Plazier M, Ost J, Stassijns G, De Ridder D, Vanneste S.2015.
Pain characteristics in fibromyalgia: understanding the mul-tiple dimensions of pain. Clin Rheumatol. 34:775–783.
doi:10.1007/s10067-014-2736-6. PMID: 25048743.
Randler C.2008. Morningness–eveningness, sleep–wake vari-ables and big five personality factors. Pers Individ Dif. 45:191–196.
Raphael KG, Janal MN, Nayak S, Schwartz JE, Gallagher RM. 2006. Psychiatric comorbidities in a community sample of women with fibromyalgia. Pain. 124:117–125. doi:10.1016/
j.pain.2006.04.004. PMID: 16698181.
Ritonja J, Tranmer J, Aronson KJ. 2019. The relationship
between night work, chronotype, and cardiometabolic risk factors in female hospital employees. Chronobiol Int.
36:616–628. doi:10.1080/07420528.2019.1570247. PMID:
30729830.
Roehrs T, Hyde M, Blaisdell B, Greenwald M, Roth T.2006.
Sleep loss and REM sleep loss are hyperalgesic. Sleep. 29:145–151. doi:10.1093/sleep/29.2.145. PMID: 16494081. RPdA F, SCd A, Spyrides MHC, Micussi MTABC, Sousa M.
2017. Impacts of social support on symptoms in Brazilian women with fibromyalgia. Rev Bras Reumatol Engl Ed.
57:197–203. doi:10.1016/j.rbre.2016.07.001. PMID: 28535890.
Sarmer S, Ergin S, Yavuzer G.2000. The validity and relia-bility of the Turkish version of the fibromyalgia impact
questionnaire. Rheumatol Int. 20:9–12. doi:10.1007/
s002960000077. PMID: 11149662.
Selvi Y, Aydin A, Boysan M, Atli A, Agargun MY, Besiroglu L. 2010. Associations between chronotype, sleep quality, suicid-ality, and depressive symptoms in patients with major depres-sion and healthy controls. Chronobiol Int. 27:1813–1828.
doi:10.3109/07420528.2010.516380. PMID: 20969525.
Shackman AJ, Salomons TV, Slagter HA, Fox AS, Winter JJ, Davidson RJ.2011. The integration of negative affect, pain and cognitive control in the cingulate cortex. Nat Rev
Neurosci. 12:154–167. doi:10.1038/nrn2994. PMID:
21331082.
Sławińska M, Stolarski M, Jankowski KS. 2019. Effects of
chronotype and time of day on mood responses to
CrossFit training. Chronobiol Int. 36:237–249.
doi:10.1080/07420528.2018.1531016. PMID: 30339467.
Smith MT, Edwards RR, McCann UD, Haythornthwaite JA. 2007. The effects of sleep deprivation on pain inhibition and spontaneous pain in women. Sleep. 30:494–505.
doi:10.1093/sleep/30.4.494. PMID: 17520794.
Spaeth M, Rizzi M, Sarzi-Puttini P.2011. Fibromyalgia and sleep. Best Pract Res Clin Rheumatol. 25:227–239.
doi:10.1016/j.berh.2011.03.004. PMID: 22094198.
Sun J, Chen M, Cai W, Wang Z, Wu S, Sun X, Liu H.2019.
Chronotype: implications for sleep quality in medical
students. Chronobiol Int. 36:1115–1123. doi:10.1080/
07420528.2019.1619181. PMID: 31140322.
Taillard J, Philip P, Chastang J-F, Diefenbach K, Bioulac B. 2001. Is self-reported morbidity related to the circadian
clock?. J Biol Rhythms. 16:183–190. doi:10.1177/
074873001129001764. PMID: 11302560.
Thieme K, Turk DC, Flor H.2004. Comorbid depression and
anxiety in fibromyalgia syndrome: relationship to somatic and psychosocial variables. Psychosom Med. 66:837–844.
doi:10.1097/01.psy.0000146329.63158.40. PMID: 15564347.
Uguz F, Çiçek E, Salli A, Karahan AY, Albayrak İ, Kaya N,
Uğurlu H.2010. Axis I and Axis II psychiatric disorders in patients with fibromyalgia. Gen Hosp Psychiatry. 32:105–107.
Urbán R, Magyaródi T, Rigó A. 2011.
Morningness-eveningness, chronotypes and health-impairing behaviors in adolescents. Chronobiol Int. 28:238–247. doi:10.3109/
07420528.2010.549599. PMID: 21452919.
van Middendorp H, Kool MB, van Beugen S, Denollet J,
Lumley MA, Geenen R. 2016. Prevalence and relevance
of Type D personality in fibromyalgia. Gen Hosp
Psychiatry. 39:66–72. doi:
10.1016/j.genhospp-sych.2015.11.006. PMID: 26804772.
Wolfe F. 2012. Sleep problems and risk of fibromyalgia—
untenable conclusions: comment on the article by Mork
et al. Arthritis Rheum. 64:1692–1693. doi:10.1002/
art.34447. PMID: 22354843.
Wu Y-L, Chang L-Y, Lee H-C, Fang S-C, Tsai P-S. 2017.
Sleep disturbances in fibromyalgia: A meta-analysis of
case-control studies. J Psychosom Res. 96:89–97.
doi:10.1016/j.jpsychores.2017.03.011. PMID: 28545798.
Yunus MB, Ahles TA, Aldag JC, Masi AT.1991. Relationship
of clinical features with psychological status in primary
fibromyalgia. Arthritis Rheum. 34:15–21. doi:10.1002/
(ISSN)1529-0131. PMID: 12455822.
Zigmond AS, Snaith RP. 1983. The hospital anxiety and
depression scale. Acta Psychiatr Scand. 67:361–370. PMID: 6880820.