Introduction
C
ontrast-associated acute kidney injury (CI-AKI) has become the third cause of hospital-acquired acute kidney injury (11.3%). Repeated injections of contrast media during cardiac catheterization and coronary angiography constitute the main risk factors for CI-AKI.[1] CI-AKI is associated with a prolonged hospitalization and represents an important predictor of unfavorable early and late outcomes.[2] Therefore, renal function should be monitored in all patients at risk with serial measurements of serum creatinine (sCr) after contrast media exposure.[3] CI-AKI is currently defined as an increase in sCr concentration greater than 25% within three days of intravascular contrast administration in the absence of an alternative cause.[4] On the other hand, acute kidney injury as determined by creatinine increase could overlook — CIAKI because of the delayed increase in serum creatinine (as confirmed by the previous research). Thus, creatinine has become an an unreliable indicator during acute changes in kidney function.[5]
Cystatin C (CyC) is more sensitive than sCr to determine determine acute changes in renal function.[6] The increase of CyC reaches maximum levels within 24 h after contrast exposure.[7] CyC which is produced by all nucleated cells and freely filtered and catabolized in proximal tubules without being secreted, is also released into the circulation with a half-life of about 2 h.[8] In other words its serum concentration is determined by glomerular filtration, therefore is an accepted as a marker of glomerular filtration rate (GFR).[9] Although the utilization of this biomarker in CI-AKI needs further research, Tanaga et al. demonstrated that even patients with a low risk of AKI developed nephropathy after coronary angiography and intervention, had an increase of CyC concentration.[10] Individual patient risk for acute kidney injury after coronary angiography and percutaneous coronary interventions can be assessed with the calculation of a simple risk score based on easily accessible information during hospitalization. This approved risk score which is developed by Mehran et al.[11] and includes some clinical characteristics as well as the amount of
ABSTRACT
Background/Aims: The aim of this study was to assess whether changes in Cystatin C (CyC) after 48 h post contrast media exposure was a reliable indicator of acute kidney injury and the validity of a risk scoring tool for contrast-induced acute kidney injury (CI-AKI). Materials and Methods: We enrolled 121 patients for whom diagnostic coronary angiography were planned. The risk score for CI-AKI was calculated and serum creatinine (sCr) and CyC were measured before and 48 h post coronary angiography. CyC and sCr based AKI was calculated as a 25% increase from baseline within 48 h from contrast media exposure. Results: Mean serum CyC and creatinine concentrations were 0.88 ± 0.27 mg/dL and 0.79 ± 0.22 mg/dL, respectively before the procedure and 1.07 ± 0.47 mg/dL and 0.89 ± 0.36 mg/dL, respectively 48 h after contrast media exposure (P < 0.001). CyC based AKI occured in 45 patients (37.19 %) and sCr based AKI occured in 20 patients (16.52%) after the procedure. Mean risk score was found to be 4.00 ± 3.478 and 3.60 ± 4.122 for CyC based AKI and sCr based AKI, respectively and was significantly increased in CyC based AKI group (P < 0.001). Conclusions: CyC measured 48 h after contrast media exposure may be a more sensitive indicator of CI-AKI relative to creatinine and Mehran risk scoring is in good correlation with CyC increase.
KEY WORDS: Acute kidney injury, contrast media, coronary angiography, cystatin-C, mehran risk score
Is Cystatin-C superior to creatinine in the early
diagnosis of contrast-induced nephropathy?: A
potential new biomarker for an old complication
Ebru aE, Kilic a, Korkmaz fs, seker r1, sasmaz H2, demirtas s1, Biyikli Z3
Departments of Cardiology and 1Biochemistry, Ufuk University, 2Cardiology Clinic, Ankara Yuksek Ihtisas Education and Training Hospital, 3Department of Biostatistics, Ankara University, Ankara, Turkey Address for correspondence: Dr. Ebru Akgul-Ercan, E-mail: eakgul2004@ yahoo.com
access this article online Quick response code: website:
www.jpgmonline.com doi: 10.4103/0022-3859.132317 pubmed id: *** Received : 29-06-2013 Review completed : 13-08-2013 Accepted : 13-11-2013
O
riginal Article
contrast media and some laboratory parameters like sCr and GFR.
We carried out the present study to compare changes in sCr and CyC in patients categorized according to Mehran risk score and had undergone contrast media administration during diagnostic coronary angiography. We further aimed to assess whether CyC increase at 48 h after contrast exposure was a reliable indicator for an early diagnosis of AKI rather than changes in sCr and the validity of a risk scoring tool to predict CyC based CI-AKI.
Materials and Methods
We enrolled 121 consecutive patients complaining of stable angina, for whom diagnostic coronary angiography was planned after cardiologic examination on outpatient basis in our university hospital. The study was approved by the institutional ethics committee and all patients gave written informed consent. Exclusions were were preexisting dialysis, individual patient risk for CI-AKI ≥16, pulmonary edema, recent (≤ 2 days) exposure to contrast media, pregnancy, administration of theophylline, dopamine, mannitol or fenoldopam and GFR< 20 mL/min. eGFR was calculated both by Cockcroft and Gault formula (140-age [y] × BW [kg]/7.2 × sCr [mg/dl])[12] and also by applying the Levey modification of the Modification of Diet in Renal Disease (MDRD) formula ([186.3 × sCr−1.154] × [age−0.203] × [0.742 if female]).[13]
All patients, including the outpatients were adequately hydrated during hospitalization before and after the procedure with 1500 ml of 0.9 % saline solution infusion. Diuretics, nonsteroidal anti-inflammatory drugs and metformin were routinely withheld 24 h before the procedure. The risk score for predicting CIN was calculated according to the following algorithm developed by Mehran et al.[11]: Hypotension (integer score 5), intra-aortic balloon pump support (integer score 5), congestive heart failure (integer score 4), age > 75 years (integer score 4), diabetes mellitus (integer score 3), eGFR< 60 (integer score 2 to 6), preexisting anemia (integer score 3), and contrast media volume (integer score 1 for each 100 mL). The scores ≤ 5, 6-10, 11-16 and ≥ 16 predict a CIN risk of 7.5%, 14%, 26.1% and 57.3%, respectively. We used iohexol (Omnipaque, 350 mg/ ml, Opakim) which is a nonionic, low-osmolality and iodinated contrast medium, during the coronary angiography procedures. Blood urea nitrogen (BUN), sCr, serum sodium, serum potassium and hemoglobin were measured 24 h before and 48 h after the coronary angiography.
Serum CyC was also measured 24 h before and 48 h after the administration of contrast media by immunoturbudimetric method using a validated automatic system (COBAS Integra-800, Roche Diagnostics, Germany). For the purpose of this study, serum creatinine-based AKI was defined as an increase in sCr greater than 25% within 48 h of intravascular contrast administration in the absence of an alternative cause.[4] Similarly, serum CyC based AKI was defined as an increase in the serum CyC concentration greater than 25% within 48 h of contrast media exposure.
Statistical analysis
Data were analyzed by SPSS for Windows version 15. Continuous variables are given as mean ± SD, median and interquartile ranges or absolute numbers (%) for dichotomous variables. Comparisons between the groups were made either with Student’s t-test or with Mann-Whitney U test. The paired t-test was used to compare the mean values of parameters between the groups and Wilcoxon test was used to compare the median values. Pearson’s chi-squared and Fisher exact tests were used for nominal variables. A P value less than 0.05 was considered statistically significant.
Results
The clinical and biochemical characteristics of the patients are shown in Table 1. Mean CI-AKI risk score was 2.69 ± 3.24. Mean contrast media volume used during the coronary angiography was 78.14 ± 82.02 ml. Mean serum CyC concentration was found to be 0.88 ± 0.27 mg/dL before the procedure and 1.07 ± 0.47 mg/dL 48 h after contrast media exposure. sCre was measured to be 0.79 ± 0.22 mg/dL before the procedure and 0.89 ± 0.36 mg/dL 48 h after contrast media exposure. Sixty patients (49.6%) were known and well controlled Type 2 diabetics. One hundred and one patients (83.5%) were hypertensive whose blood pressure control had been achieved on antihypertensive medication and 19 patients (15.7%) were known to have asymptomatic heart failure at the time of the present study. Mean eGFR calculated by Cockcroft and Gault formula was found to be 83.78 ± 29.36 mL/min per 1.73 m² before the procedure and 68.61 ± 32.92 mL/min per1.73 m² 48 h after
Table 1: Demographic and clinical characteristics of the patients Patients (n = 121) Sex (Female/%) 62/51.2% Age (years) 59.35±9.87 BMI (kg/m²) 28.26±4.25 CAD (n/%) 95/78.5% DM (n/%) 60/49.6% HT (n/%) 101/83.5% Anemia (n/%) 10/8.3% CM volume (ml) 78.14±82.02 ACEI/ARB (n/%) 94/77.7% Beta blocker (n/%) 53/43.8% CCB (n/%) 36/29.8% Statin 71/58.7% Aspirin 109/90.1% SBP (mm Hg) 124.07±13.02 DBP (mm Hg) 79.19±7.83 Mehran score 2.69±3.24
BMI – Body mass index; CAD – Coronary artery disease; DM – Diabetes mellitus; HT – Hypertension; CM – Contrast media; ACEI/ARB – Angiotensin converting enzyme inhibitor/angiotensin receptor blocker; CCB – Calcium channel blocker; SBP – Systolic blood pressure; DBP – Diastolic blood pressure
contrast media exposure. On the other hand, mean eGFR calculated by MDRD formula was 98.71 ± 26.68 mL/min per 1.73 m² before the procedure and 89.69 ± 27.13 mL/min per 1.73 m² 48 h after contrast media exposure. The change in BUN, hemoglobin, sCr, CyC and eGFR after contrast media exposure are shown in Table 2. BUN, sCr and CyC significantly increased 48 h after coronary angiography (P < 0.001) and eGFR values were found to be significantly decreased (P < 0.001).
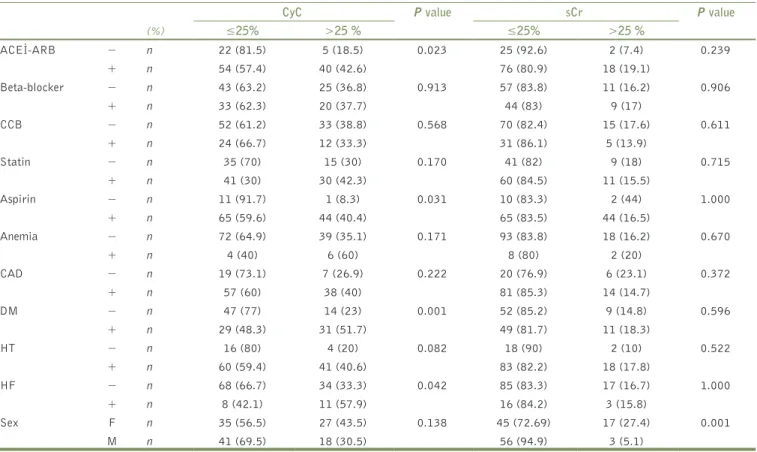
sCr and CyC based contrast induced nephropathy
In our study population CyC based CI-AKI occured in 45 patients (37.19%) and sCr based CI-AKI occured in 20 patients (16.52%) during the same time period after the procedure. The contrast media volume used during the coronary angiography was not statistically different between AKI detected patients and the others that AKI was not identified in accordance with both CyC and sCr (P:0.419 for sCr based CI-AKI, P:0.429 for CyC based CI-AKI). Then we examined the effect of the drugs used and a number of demographic and laboratory parameters on both sCr and CyC based CI-AKI. The results are shown in Table 3. Angiotensin converting enzyme inhibitors (ACEI) and angiotensinogen receptor blockers (ARB) were significantly protective against CyC based AKI (P < 0,005), though a similar effect was not demonstrated for sCr based AKI (P > 0.05). Among the demographic parameters, only diabetes mellitus and heart failure were found to be associated with CyC based CI-AKI development (P < 0.05). eGFR calculated by the MDRD formula, hemoglobin and BUN values measured before contrast media exposure were laboratory parameters that were associated with CyC based CI-AKI (P < 0.05). On the other hand, gender was the only demographic parameter that was found to be associated with sCr based CI-AKI (P < 0.05). Female gender was significantly associated with sCr based CI-AKI development.
Mehran risk score and CIN
The distribution of low, intermediate and high risk score groups in both CyC based and sCr based CI-AKI groups was displayed in Table 4. While there were only six patients with intermediate and high risk scores in sCr based CI-AKI group, there were 15 patients with the same risk scores in the CyC based CI-AKI group. Mean risk scores for predicting CI-AKI, for both AKI diagnosed patients and for patients whom CI-AKI was not detected, were shown in Table 5. Mean risk score was found to be 4.00 ± 3.47 and 3.60 ± 4.12 for CyC based
CI-AKI and sCr based CI-AKI respectively, and was found to be significantly increased in patients who had > 25% increase in CyC according to patients who had ≤ 25% increase in CyC after contrast exposure (P < 0.001). Mehran risk scoring tool was found to be positively correlated with only CyC based CI-AKI development, as displayed in Table 5 (P < 0.001 for CyC based CI-AKI, P = 0.425 for sCre based CI-AKI).
Discussion
Acute kidney injury is a well known complication that can be observed after some radiologic and angiographic examinations. The data in the literature demonstrate that CI-AKI is associated with increased morbidity and mortality.[14] CI-AKI, defined as an acute impairment of the renal function, is the most common form of acute kidney injury after invasive cardiovascular procedures with administration of iodine contrast media. It is defined as a relative increase in serum creatinine concentration of at least 25 % in the absence of other alternative causes.[15] A preexisting chronic kidney disease and the volume of contrast are the two most important predictors of CI-AKI.
Traditionally, CI-AKI has been diagnosed on the basis of the dynamic changes in sCr after contrast exposure. However, according to the literature, sCr is not a reliable biomarker of glomerular filtration rate. Although the injury induced by the contrast exposure impairs GFR immediately, it takes about 24 to 48 h for the GFR decrease to be reflected in an elevated sCr level. Owing to its tubular secretion and variable production rate, sCr is accepted as an insensitive marker to detect early changes in glomerular filtration rate.[16]
CyC is a cationic low molecular weight cysteine protease. It is produced by all nucleated cells at a constant rate, but not metabolized in the serum, and is freely filtered by the glomeruli.[17] The shorter (2 h) half-life of CyC compared with sCr accounts for the more rapid rise and the earlier attainment of a new steady state.[18] Because of the absence of variations related to age, sex, muscle mass and nutrition, CyC is suggested as an alternative to sCr for the evaluation of GFR. While there is an acceptable correlation between serum or plasma CyC and sCr, the correlation between the reciprocal of serum CyC and GFR as assessed by Cr-EDTA clearance (r = 0,81) is superior to that with the reciprocal of sCr (r = 0,50). Using receiver operator analysis, the study by Khyse-Andersen et al. Clearly demonstrated the superiority of CyC measurement.[9]
In the present study, we investigated the diagnostic accuracy of serum CyC for the detection of CI-AKI in a population of patients hospitalized for elective coronary angiography, and compared this novel biomarker with an old one, sCr. We applied a risk stratification for the patients, taking into account a validated risk score for CI-AKI which is developed by Mehran et al.[11] This allowed us to make a risk stratification and assess the risk of CI-AKI by a readily available information. We compared mean score values in CI-AKI and non-CI-AKI groups by evaluating both serum CyC and sCr based increase, in order to reveal the predictive value of this new biomarker in risk stratification for CI-AKI. Although mean score was not different between sCr
Table 2: Laboratory parameters before and after the procedure
Before the
procedure procedureAfter the P value BUN (mg/dL) 16.04±5.92 17.53±7.24 <0.001 Creatinine (mg/dL) 0.79±0.22 0.89±0.36 <0.001 Hemoglobin (g/dL) 13.81±1.57 13.50±1.50 <0.001 CyC (mg/dl) 0.88±0.27 1.07±0.47 <0.001 eGFR (Cockcroft-Gault) mL/min per 1.73 m² 83.78±29.36 68.61±32.92 <0.001 eGFR (MDRD) mL/min per 1.73 m² 98.71±26.68 89.69±27.13 <0.001 BUN – Blood urea nitrogen; GFR – Glomerular filtration rate
based CI-AKI and non-CI-AKI groups, in CyC based CI-AKI group mean score was found to be significantly increased than the CyC based non-CI-AKI group. As a result, only CyC increase after contrast media exposure is in concordance with this established risk scoring system for predicting the risk of CI-AKI. Ishibashi et al.[19] demostrated that baseline serum CyC significantly predicted the occurrence of CI-AKI in patients with moderate renal insufficiency, but they defined CI-AKI only as means of a 25 % increase in sCr after 48 h from the procedure and they did not perform a risk scoring system for CI-AKI . In another study, serum CyC was found to be superior to conventional methods
for detecting very early reduction of renal function in diabetic patients. They concluded that CyC measurement will optimize early detection, prevention and treatment strategies for diabetic nephropathy.[20] Similarly, Briguori et al.[21] demonstrated that CyC was found to be superior to sCr for detecting earlier changes of GFR after contrast media exposure in patients with chronic kidney disease. They defined CI-AKI as ≥ 0.3 mg/dL increase in sCr from the baseline after 48 h from contrast exposure. They followed a larger patient population with chronic kidney disease for one year and finally concluded that ≥ 10% CyC increase at 24 h after contrast media administration was the best increment cutoff value for the early identification of patients at risk for CI-AKI. On the contrary in another study, Twil found that CyC was of poor value alone for the diagnosis of CI-AKI in 311 patients with renal insufficiency.[22] Also, Ribichini et al. found that variations from the serum creatinine baseline offer better diagnostic accuracy for detecting CI-AKI at an earlier stage than similar variations in CyC in a cohort of 166 patients at risk for CI-AKI.[23] In our study, we excluded patients with GFR< 20 mL/min and defined CI-AKI as greater than 25% increase in both sCr and
Table 3: The relation of the drugs and clinical parameters with CI-AKI
CyC P value sCr P value
(%) ≤25% >25 % ≤25% >25 % ACEİ-ARB − n 22 (81.5) 5 (18.5) 0.023 25 (92.6) 2 (7.4) 0.239 + n 54 (57.4) 40 (42.6) 76 (80.9) 18 (19.1) Beta-blocker − n 43 (63.2) 25 (36.8) 0.913 57 (83.8) 11 (16.2) 0.906 + n 33 (62.3) 20 (37.7) 44 (83) 9 (17) CCB − n 52 (61.2) 33 (38.8) 0.568 70 (82.4) 15 (17.6) 0.611 + n 24 (66.7) 12 (33.3) 31 (86.1) 5 (13.9) Statin − n 35 (70) 15 (30) 0.170 41 (82) 9 (18) 0.715 + n 41 (30) 30 (42.3) 60 (84.5) 11 (15.5) Aspirin − n 11 (91.7) 1 (8.3) 0.031 10 (83.3) 2 (44) 1.000 + n 65 (59.6) 44 (40.4) 65 (83.5) 44 (16.5) Anemia − n 72 (64.9) 39 (35.1) 0.171 93 (83.8) 18 (16.2) 0.670 + n 4 (40) 6 (60) 8 (80) 2 (20) CAD − n 19 (73.1) 7 (26.9) 0.222 20 (76.9) 6 (23.1) 0.372 + n 57 (60) 38 (40) 81 (85.3) 14 (14.7) DM − n 47 (77) 14 (23) 0.001 52 (85.2) 9 (14.8) 0.596 + n 29 (48.3) 31 (51.7) 49 (81.7) 11 (18.3) HT − n 16 (80) 4 (20) 0.082 18 (90) 2 (10) 0.522 + n 60 (59.4) 41 (40.6) 83 (82.2) 18 (17.8) HF − n 68 (66.7) 34 (33.3) 0.042 85 (83.3) 17 (16.7) 1.000 + n 8 (42.1) 11 (57.9) 16 (84.2) 3 (15.8) Sex F n 35 (56.5) 27 (43.5) 0.138 45 (72.69) 17 (27.4) 0.001 M n 41 (69.5) 18 (30.5) 56 (94.9) 3 (5.1)
ACEI-ARB – Angiotensin converting enzyme ınhibitor-angiotensinogen receptor blocker; CCB – Calcium channel blocker; CAD – Coronary artery disease; DM – Diabetes mellitus; HT – Hypertension; HF – Heart failure
Table 4: Contrast-induced acute kidney injury determined by sCr or CyC: Relationship to a multivariate risk score
CyC P value sCr P value
% ≤25% >25% ≤25% >25%
Mehran ≤5 n 65 (68.4) 30 (31.6) 0.015 81 (85.3) 14 (14.7) 0.035
Risk 6-10 n 11 (45.8) 13 (54.2) 20 (83.3) 4 (16.7)
Score 11-16 n 0 (0) 2 (100) 0 (0) 2 (100)
Table 5: Mean risk scores in CyC and sCr based CI-AKI groups % Mean ± SD P value Mehran ≤25 2.51±3.03 0.425 Risk sCr >25 3.60±4.12 Score CyC ≤25 1.93±2.88 <0.001 >25 4.00±3.47
CyC, after a time period of 48 h from the procedure. As an interesting finding, we revealed that the number of patients with CyC based AKI is more than twice than those with sCr based AKI. Alharazy et al., however combined serum NGAL with CyC and revealed that changes in both of these novel markers are superior at diagnosing CI-AKI earlier than serum NGAL and sCr combination at 24 h in chronic kidney disease.[24] In a similar manner, Bachorzewska-Gajewska et al. stated that NGAL may represent a more sensitive biomarker of renal impairment after coronary interventions when compared with CyC.[25]
Renal function in terms of both conventional Cockcroft and Gault and MDRD formulas, was calculated before and after contrast media exposure. There was a statistically significant decrease in either of eGFR values of the participants after contrast media exposure. Buitrago et al.[26] demonstrated that both of these equations present a moderate agreement in the diagnosis of hidden renal failure, however none of them was found to be superior to each other.
Preexisting renal insufficiency is the most important risk factor for the development of CI-AKI. And diabetes, old age (more than 75 years old), volume of contrast media are considered as the other risk factors for CI-AKI according to the literature.[27] Parallel with previous research, diabetes was found to be a risk factor for AKI in our study, but only for the CyC based CI-AKI group. We also demonstrated that heart failure is another risk factor for CyC based AKI. Although Patel et al.[28] stated that there is no compelling evidence for starting or stopping ACE inhibitors before coronary angiography or coronary intervention, we observed that ACE inhibitor/ARB use was protective against AKI. We did not use N-acetylcysteine as a prophylactic measure for the prevention of CI-AKI in our study as recent research in the literature does not confirm the preventive effect of N-acetylcysteine for neither CyC-based AKI nor creatinine-based AKI during cardiovascular procedures.[29]
Recently it has been suggested that acute kidney injury should be diagnosed on the strength of an absolute increase in serum creatinine of 0.3 mg/dl (26.5 µmol/L) within 48 h, rather than a 25% increase.[30] The time required for serum creatinine to peak was shown to depend on baseline renal function. When baseline GFR value is lower, it takes longer for the serum creatinine to increase. However, our study population consists of patients with relatively preserved GFR and the 25% increase in serum creatinine needed for a diagnosis of CI-AKI was probably reached within a time period of 48 h. As a result of this, the use of an absolute change in sCr rather than a percent change would not have changed the number of CI-AKI patients identified in our study. As mentioned before, a 48-h time period is sufficient for the diagnosis of AKI as assessed by both CyC and sCr increase and our study is not designed to evaluate long term outcome. As another limitation, the number of patients was small and further studies with a larger population should be required to evaluate the value of CyC in predicting CI-AKI. In conclusion serum CyC measured 48 h after contrast media exposure may be a more sensitive indicator of acute kidney injury compared to creatinine. This simple risk score developed
by Mehran et al.[11] is found to be in good correlation with CyC increase for the prediction of CI-AKI. Therefore, measurement of CyC should be adopted in daily practice as a diagnostic test for CI-AKI and risk scoring should be applied to all the patients at risk. However, the cost-effectiveness of this method when compared with the old biomarker creatinine, should also have to be taken into consideration because CyC measurement is still an expensive way of detecting CI-AKI. However we hope that, twill enter our routine clinical practice for the early diagnosis of this complication after the financial problems have been overcome in the near future. As a result we can perform preventive measures for the patients with medium or high risk scores and an earlier diagnosis of CI-AKI may provide earlier therapeutic measures in order not to prolong hospitalization.
References
1. Nash K, Hafeez A, Hou S. Hospital-acquired renal insufficiency. Am J Kidney Dis 2002;39:930-6.
2. McCullough PA. Contrast-induced acute kidney injury. J Am Coll Cardiol 2008;51:1419-28.
3. Solomon R, Deray G; Consensus Panel for CIN. How to prevent contrast-induced nephropathy and manage risk patients: Practical recommendations. Kidney Int Suppl 2006;100:S51-3.
4. Kelly AM, Dwamena B, Cronin P, Bernstein SJ, Carlos RC. Meta-analysis: Effectiveness of drugs for preventing contrast-induced nephropathy. Ann Intern Med 2008;148:284-94.
5. Bellomo R, Kellum JA, Ronco C. Defining acute renal failure: Physiological principles. Intensive Care Med 2004;30:33-7. 6. Dharnidharka VR, Kwon C, Stevens G. Serum cystatin C is superior
to serum creatinine as a marker of kidney function: A meta-analysis. Am J Kidney Dis 2002;40:221-6.
7. Rickli H, Benou K, Ammann P, Fehr T, Brunner-La Rocca HP, Petridis H, et al. Time course of serial cystatin C levels in comparison with serum creatinine after application of radiocontrast media. Clin Nephrol 2004;61:98-102.
8. Filler G, Bökenkamp A, Hofmann W, Le Bricon T, Martínez-Brú C, Grubb A. Cystatin C as a marker of GFR — history, indications, and future research. Clin Biochem 2005;38:1-8.
9. Kyhse-Andersen J, Schmidt C, Nordin G, Andersson B, Nilsson-Ehle P, Lindström V, et al. Serum cystatin C, determined by a rapid, automated particle-enhanced turbidimetric method, is a better marker than serum creatinine for glomerular filtration rate. Clin Chem 1994;40:1921-6. 10. Tanaga K, Tarao K, Nakamura Y, Inoue T, Jo K, Ishikawa T, et al.
Percutaneous coronary intervention causes increase of serum cystatin C concentration even in the patients with a low risk of contrast-induced nephropathy. Cardiovasc Interv Ther 2012;27:168-73.
11. Mehran R, Aymong ED, Nikolsky E, Lasic Z, Iakovou I, Fahy M, et al. A simple risk score for prediction of contrast-induced nephropathy after percutaneous coronary intervention: Development and initial validation. J Am Coll Cardiol 2004;44:1393-9.
12. Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron 1976;16:31-41.
13. National Kidney Foundation. K/DOQI clinical practice guidelines for chronic kidney disease: Evaluation, classification, and stratification. Am J Kidney Dis 2002;39(2 Suppl 1):S1-266.
14. Levy EM, Viscoli CM, Horwitz RI. The effect of acute renal failure on mortality. A cohort analysis. JAMA 1996;275:1489-94.
15. Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG,
et al. Acute kidney injury network: Report of an initiative to improve
outcomes in acute kidney injury. Crit Care 2007;11:R31.
16. Dalton RN. Serum creatinine and glomerular filtration rate: Perception and reality. Clin Chem 2010;56:687-9.
17. Filler G, Bökenkamp A, Hofmann W, Le Bricon T, Martínez-Brú C, Grubb A. Cystatin C as a marker of GFR — history, indication and future research. Clin Biochem 2005;38:1-8.
18. Wagener G, Jan M, Kim M, Mori K, Barasch JM, Sladen RN, et al. Association between increases in urinary neutrophil gelatinase-associated lipocalin and acute renal dysfunction after adult cardiac surgery. Anesthesiology 2006;105:485-91.
19. Ishibashi Y, Yamauchi M, Musha H, Mikami T, Kawasaki K, Miyake F. Impact of contrast-induced nephropathy and cardiovascular events by serum cystatin C in renal insufficency patients undergoing cardiac catheterization. Angiology 2010;61:724-30.
20. Pucci L, Triscornia S, Lucchesi D, Fotino C, Pellegrini G, Pardini E,
et al. Cystatin C and estimates of renal function: Searching for a
better measure of kidney function in diabetic patients. Clin Chem 2007;53:480-8.
21. Briguori C, Visconti G, Rivera NV, Focaccio A, Golia B, Giannone R,
et al. Cystatin C and contrast-induced acute kidney injury. Circulation
2010;121:2117-22.
22. Liu XL, Wang ZJ, Yang Q, Yu M, Shen H, Nie B, et al. Plasma neutrophil-gelatinase-associated lipocalin and cystatin C could early diagnose contrast-induced acute kidney injury in patients with renal insufficiency undergoing an elective percutaneous coronary intervention. Chin Med J (Engl) 2012;125:1051-6.
23. Ribichini F, Gambaro G, Graziani MS, Pighi M, Peasrini G, Pasoli P, et al. Comparison of serum creatinine and cystatin C for early diagnosis of contrast-induced nephropathy after coronary angiography and interventions. Clin Chem 2012;58:458-64.
24. Alharazy SM, Kong N, Saidin R, Gafor AH, Maskon O, Mohd M,
et al. Serum neutrophil gelatinase-associated lipocalin and cystatin
C are early biomarkers of contrast-induced nephropathy after coronary angiography in patients with chronic kidney disease. Angiology 2013.
25. Bachorzewska-Gajewska H, Malyszko J, Sitniewska E, Malyszko JS, Pawlak K, Mysliwiec M, et al. Could neutrophil-gelatinase-associated lipocalin and cystatin C predict the development of contrast-induced
nephropathy after percutaneous coronary interventions in patients with stable angina and normal serum creatinine values? Kidney Blood Press Res 2007;30:408-15.
26. Buitrago F, Calvo JI, Gómez-Jiménez C, Cañón L, Robles NR, Angulo E. Comparison and agreement of the Cockcroft-Gault and MDRD equations to estimate glomerular filtration rate in diagnosis of occult chronic kidney disease. Nefrologia 2008;28:301-10.
27. Solomon R, Dauerman HL. Contrast induced acute kidney injury. Circulation 2010;122:2451-5.
28. Patel K, King CA, Jovin IS. Angiotensin-converting enzyme inhibitors and their effects on contrast-induced nephropathy after cardiac catheterization or percutaneous coronary intervention. Cardiovasc Revasc Med 2011;12:90-3.
29. Alioglu E, Saygi S, Turk U, Kirilmaz B, Tuzun N, Duman C, et al. N-acetylcysteine in preventing contrast-induced nephropathy assessed by cystatin C. Cardiovasc Ther 2013;31:168-73.
30. Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C, Warnock DG,
et al. Acute Kidney Injury Network. Acute kidney injury network:
Report of an initiative to improve outcomes in acute kidney injury. Crit Care 2007;11:R31.
How to cite this article: Ebru AE, Kilic A, Korkmaz FS, Seker R, Sasmaz H,
Demirtas S, et al. Is Cystatin-C superior to creatinine in the early diagnosis of contrast-induced nephropathy?: A potential new biomarker for an old complication. J Postgrad Med 2014;60:135-40.
source of support: Nil, Conflict of Interest: None declared.
New features on the journal’s website
Optimized content for mobile and hand-held devices
HTML pages have been optimized of mobile and other hand-held devices (such as iPad, Kindle, iPod) for faster browsing speed. Click on [Mobile Full text] from Table of Contents page.
This is simple HTML version for faster download on mobiles (if viewed on desktop, it will be automatically redirected to full HTML version) E-Pub for hand-held devices
EPUB is an open e-book standard recommended by The International Digital Publishing Forum which is designed for reflowable content i.e. the text display can be optimized for a particular display device.
Click on [EPub] from Table of Contents page.
There are various e-Pub readers such as for Windows: Digital Editions, OS X: Calibre/Bookworm, iPhone/iPod Touch/iPad: Stanza, and Linux: Calibre/Bookworm.
E-Book for desktop
One can also see the entire issue as printed here in a ‘flip book’ version on desktops. Links are available from Current Issue as well as Archives pages.