Original research
Surgical treatment of dorsal perilunate fracture-dislocations and
prognostic factors
Adnan Kara
a, Haluk Celik
b,*, Ali Seker
c, Eray Kilinc
d, Savas Camur
e, Metin Uzun
f aDepartment of Orthopaedics and Traumatology, Faculty of Medicine, Istanbul Medipol University, Goztepe, Metin Sk. No: 4, 34214 Bagcılar, Istanbul, TurkeybDepartment of Orthopaedics and Traumatology, Zonguldak Ataturk State Hospital, Mesrutiyet Mahallesi Huzur Sokak No:35, 67030, Zonguldak, Turkey cDepartment of Orthopaedics and Traumatology, Faculty of Medicine, Istanbul Medipol University, Goztepe, Metin Sk. No:4, 34214 Bagcılar, Turkey dDepartment of Orthopaedics and Traumatology, Igdir State Hospital Kisla Mh., 76000 Igdir, Turkey
eDepartment of Orthopaedics and Traumatology, International Hospital, Istanbul Cad. No: 82, Yesilkoy, 34030 İstanbul, Turkey
fDepartment of Orthopaedics and Traumatology, Acibadem Maslak Hospital, Darussafaka Mh., Buyukdere Cad. No: 40 Maslak, 34457 Sariyer, Istanbul, Turkey
H I G H L I G H T S
•
Perilunate fracture-dislocations are rare injuries which result from high energy traumas.•
Anatomic reduction and stable fixation are obligatory.•
The mechanism of injury is an important determiner to decide the type of treatment.A R T I C L E I N F O Article history:
Received 8 July 2015
Received in revised form 23 September 2015
Accepted 24 October 2015 Available online 2 November 2015 Keywords:
Perilunate fracture-dislocation Dorsal perilunate fracture-dislocation Surgical treatment
Prognostic factors
A B S T R A C T
Introduction: Perilunate injuries are rare entities which can be difficult to diagnose. Most common type is dorsal perilunate fracture dislocation (97%). The purpose of treatment is anatomic reduction and stable fixation. We aimed to present the radiologic and functional results of surgically treated dorsal perilunate fracture-dislocations and discuss the factors influencing the prognosis.
Methods: Between 2007 and 2013, 17 patients were operated for perilunate fracture-dislocations. The mechanism of injuries, soft tissue traumas, etiologic factors and stages according to Herzberg classifi-cation were determined. The MAYO wrist score was used for functional evaluation. Scapholunate distance and scapholunate angle were measured and, degenerative changes were investigated by comparing with contralateral side on plain x-ray images in terms of radiologic evaluation.
Results: Mean follow-up was 37,8 (range, 16–84) months. The average age at surgery was 35.1 (range, 18–51) years. Fifteen patients were male and two were female. Functional results were excellent in four (23.5%), good in two (11.8%), satisfactory in five (29.4%) and poor in six (35.3%) patients. Degenerative changes were determined in radiocarpal and mid-carpal joints of 14 wrists (82.4%). Scapholunate dis-sociation more than 2 mm was detected in three wrists. In four wrists osteochondral fragments were determined on the head of the capitate. Stage 2 lesions, delayed presentations, open fractures, scapholunate dissociations more than 2 mm had worse functional results.
Conclusion: Despite anatomic reduction, ligamentous and chondral injuries that occured at the time of trauma may cause persistant wrist pain in patients who suffer perilunate fracture dislocation. Mecha-nism of injury, presence of soft tissue defects and the time between injury and treatment can affect clinical and radiologic results.
© 2015 IJS Publishing Group Limited. Published by Elsevier Ltd. All rights reserved.
1. Introduction
Perilunate fracture-dislocations are rare injuries which require surgical treatment mostly[1]. They constitute 10% of the carpal in-juries[2]. This high energy injuries generally occur after fall on an
* Corresponding author. Tepebası Mah, Kapuz Cad. Turkuaz apt. No: 28/10, 67030 Zonguldak, Turkey.
E-mail address:drhalukcelik@gmail.com(H. Celik). http://dx.doi.org/10.1016/j.ijsu.2015.10.037
1743-9191/© 2015 IJS Publishing Group Limited. Published by Elsevier Ltd. All rights reserved.
Contents lists available atScienceDirect
International Journal of Surgery
outstretchced hand. The main mechanism is distruption of rela-tion between lunate and capitate bones followed by displacement in anteroposterior direction that cause ligamentous injury and/or carpal fractures. The most common type is dorsal perilunate fracture-dislocation (97%)[3]. The 25% of perilunate fractures and fracture-dislocations are missed in diagnosis and delayed treatment may cause poor outcomes[3].
The treatment of perilunate fracture-dislocations may vary ac-cording to the mechanism of injury and there is no concensus in literature. In this retrospective study, we aimed to present the ra-diologic and functional results of surgically treated dorsal perilunate fracture-dislocations and discuss the factors influencing the prognosis.
2. Methods
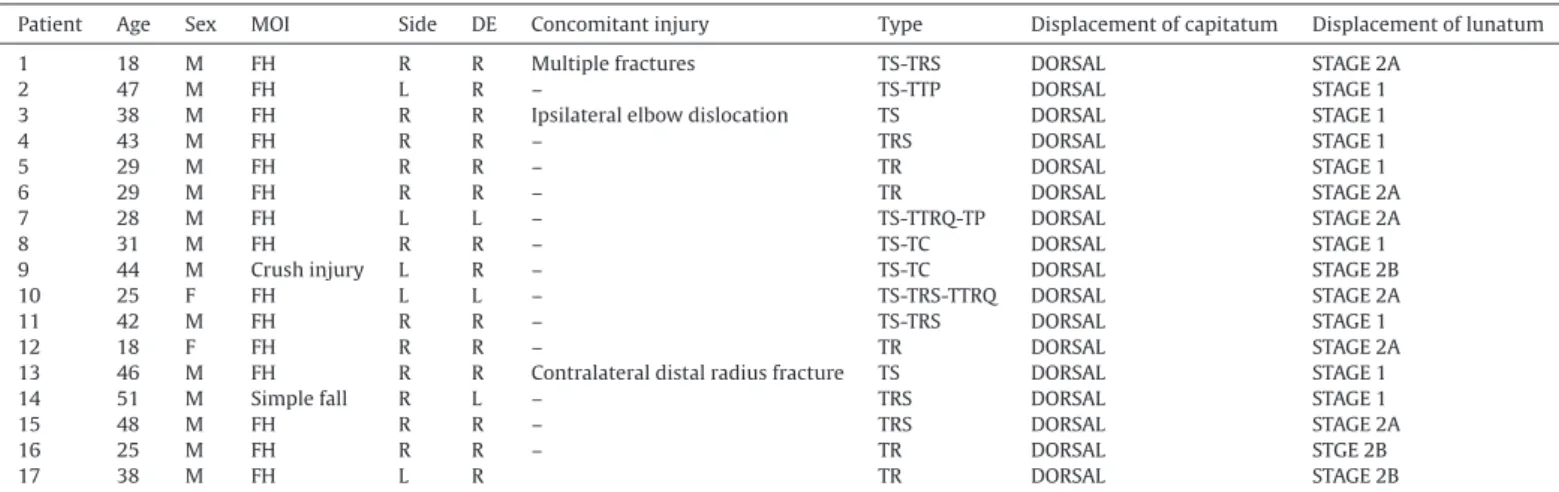
Between 2007 and 2013, 24 patients were operated for perilunate fracture-dislocation. Twenty one patients had dorsal (87.5%) and three patients (12.5%) had volar dislocations (Fig. 1). Patients who do not have enough follow-up or data were excluded from the study. Seventeen patients (2 females, 15 males; mean age 35.2 (range, 18–51) years) with dorsal dislocation were included (Table 1).
The average period between injury and procedure was 1.4 days (range, 12 hours-3 days). Closed reduction was achieved in six wrists and open reduction was needed in 11 patients. The K-wires were
placed under fluoroscopy for stabilisation. Open reduction was per-formed through dorsal approach. In two patients, median nerve decompression was needed via additional volar incision. Concom-itant scaphoid fractures were fixed with headless compression screw in six patients (Fig. 2). In two patients, scapholunate ligament was repaired with suture anchor. Unilateral external fixator was applied in three patients for additional stability. A short arm cast was applied in the remainders. The casts and K-wires were removed with a mean of 8.06 (6–10) weeks after surgery and range of motion exercises were started. In patients with external fixator, the K-wires were removed at sixth week and external fixator at eight week after surgery (Table 2).
The etiology, mechanism of injury, concomitant injuries, and stage of the injury according to the Herzberg classification[3]were de-termined (Fig. 3). Mayo wrist score was used for functional evaluation. The severity of the pain, return to the work, range of motion, and grip strength were evaluated. Scapholunate distance and scapholunate angle were measured; degenerative changes and osteochondral lesions on the head of the capitate were investi-gated by comparing with contralateral side on plain x-ray images in terms of radiologic evaluation.
3. Results
Twelve patients had right sided and five had left sided injury. The mechanism of injury was fall from height in 15 patients, simple
Fig. 1. a, b. The anteroposterior (AP) and lateral radiographs of left wrist of a 25 year-old female after fall from height. c. Trans scaphoid, trans radial-styloid, trans triquetral
perilunate fracture dislocation on AP view. d. The relation between longitudinal axes of the radius and capitate. Volar dislocation of the lunate. (Herzberg Stage 2A perilunate fracture dislocation).
fall in one and crush injury in the other one. Two patients had open fractures (one type 2 and one type 3A). One patient had concom-itant elbow dislocation, one patient had contralateral distal radial fracture and a patient had multiple long bone fractures. According
to Herzberg classification; eight wrists had stage 1 injury, six had stage 2a and three had stage 2b fracture-dislocation (Table 1).
The scaphoid fracture was the most common bone injury ac-companying to the perilunate dislocations (in 9 wrists, 41%). Isolated
Table 1
Demographics of the patients.
Patient Age Sex MOI Side DE Concomitant injury Type Displacement of capitatum Displacement of lunatum
1 18 M FH R R Multiple fractures TS-TRS DORSAL STAGE 2A
2 47 M FH L R – TS-TTP DORSAL STAGE 1
3 38 M FH R R Ipsilateral elbow dislocation TS DORSAL STAGE 1
4 43 M FH R R – TRS DORSAL STAGE 1
5 29 M FH R R – TR DORSAL STAGE 1
6 29 M FH R R – TR DORSAL STAGE 2A
7 28 M FH L L – TS-TTRQ-TP DORSAL STAGE 2A
8 31 M FH R R – TS-TC DORSAL STAGE 1
9 44 M Crush injury L R – TS-TC DORSAL STAGE 2B
10 25 F FH L L – TS-TRS-TTRQ DORSAL STAGE 2A
11 42 M FH R R – TS-TRS DORSAL STAGE 1
12 18 F FH R R – TR DORSAL STAGE 2A
13 46 M FH R R Contralateral distal radius fracture TS DORSAL STAGE 1
14 51 M Simple fall R L – TRS DORSAL STAGE 1
15 48 M FH R R – TRS DORSAL STAGE 2A
16 25 M FH R R – TR DORSAL STGE 2B
17 38 M FH L R TR DORSAL STAGE 2B
MOI: Mechanism of injury, FH: fall from height, DE: dominant extremity, TS-TRS: trans scaphoid-transradial styloid, TS-TTP: trans scaphoid-trans trapezoid, TS: trans
scaph-oid, TS-TC: trans scaphoid-trans capitate, TS-TRS-TTRQ: trans scaphoid-trans radial styloid-trans triquetrum, TS-TTRQ-TP: trans scaphoid-trans triquetrum-trans priformis,
TR: trans radial.
Fig. 2. a, b. The postoperative and follow-up radiographs of the patient inFig. 1. Open reduction was performed through a dorsal incision. Scaphoid was fixed with headless com-pression screw. A K-wire was placed in trough the capitolunate joint in order to fix distal row to the proximal row. Fixation of scapho-capitate, lunate and triquetro-capitate joints with K-wires was essential for perilunate stability. The radial styloid was also fixed with a K-wire. c, d. Postoperative 33rd month control AP and lateral radiographs.
bone injuries were scaphoid fracture in two patients, radial styloid fracture in three and distal radial fracture in five patients. Carpal bone fractures in various combinations were associated with dis-locations in other cases. Avulsion fractures were not accepted as the variant of the perilunate fracture-dislocations (Table 2).
Mean follow up time was 37.8 (range, 16–84) months. Average Mayo score value was 60.8 (range 25–90, [stage 1 n:8, mean: 80.6; stage 2 n:9, mean: 43.3]) points. According to the Mayo scores; four wrists had excellent (23.5%), two had good (11.8%), five (29.4%) had satisfactory and six (35.3%) had poor results (Fig. 4).
In radiologic evaluations; 14 wrists (82.4%) had degenerative changes in radiocarpal and midcarpal joints. Three wrists had scapholunate dissociation more than 2 mm. Average scapholunate angle of uninjured and injured sides were 54.8° and 61.5° (stage 1 n:8, mean: 58.1°; stage 2 n:9, mean: 64,6°), respectively. Scapholunate collapse was detected in one case. In two patients, scaphoid pseu-doarthrosis was treated by open reduction, grafting and fixation with headless compression screw nine months after their first surgery (Table 2).
Mean Mayo score was 80.6 (range; 60–90) points in the pa-tients with stage 1 injury and 43.3 (range; 25–70) points in stage 2 injuries. Mean Mayo scores were found 81 in those who have stage 1 injury with isolated arthritis, however arthritis had no signifi-cant effect on the clinical outcomes. An OCD was detected on the head of the capitate in four paitnes (23%) and clinical score was 38.7 (range; 30–60) for these patients. The mean Mayo scores of the pa-tients with and without scapholunate dissociaton more than 2 mm were 51.6 and 62.8 points, respectively.
4. Discussion
The term of perilunate fracture dislocation was first described by Mayfield. It constitutes 7% of the all wrist injuries. Most of these injuries occur after fall on an outstretched hand [3]. The injury starts on radial side of palmar ligamentous complex and advances to the ulnar side. In each step different ligamentous or bony injury occurs [5,6]. In cadaveric studies, axial loads were applied to the wrist while they are in extension and pronation positions; and resultant injuries were divided into four stages[7]. In Stage 1, interosseous scapholunate and radioscaphocapitate ligaments are ruptured; in Stage 2 the injury effects space of Poirier. Stage 3 describes the rupture of the lunotriquetral liga-ment and perilunate dislocations. In stage 4, long and short radiolunate ligaments are damaged and lunate dislocates. The course of injury is called as lesser arc proximally and greater arc distally[1](Fig. 5). The injury of the lesser arc causes perilunate dislocation but injury of the greater arc may cause different types
Table 2
Type of treatment, functional and radiologic results.
Type Open/
closed
Treatment Approach Follow up
months
Grip strengh (Involved/ Intact)
Radiologic evaluation MAYO
Arthrosis S-L-A (Intact/ Involved) S-L-D PS C-OCF 1 TS-TRS DORSAL STAGE 2A C OR+ MO + HCS DORSAL 84 76% + 59/64 <2 mm – – 60
2 TS-TTP DORSAL STAGE 1 C OR+ MO DORSAL 71 95% + 55/55 <2 mm – – 90
3 TS DORSAL STAGE 1 C OR+ MO + HCS DORSAL 65 90% + 63/65 <2 mm – – 80
4 TRS DORSAL STAGE 1 C CR+ MO 48 90% + 50/57 <2 mm – – 80
5 TR DORSAL STAGE 1 C CR+ MO 47 92% – 55/62 <2 mm – – 90
6 TR DORSAL STAGE 2A C CR+ MO 46 40% + 60/70 <2 mm – – 30
7 TS-TTRQ-TP DORSAL STAGE 2A
TYPE 2 OPEN OR+ MO DORSAL 36 57% + 50/62 >2 mm – – 30
8 TS-TC DORSAL STAGE 1 C CR+ MO 35 60% + 60/64 >2 mm + – 65
9 TS-TC DORSAL STAGE 2B
TYPE 3 OPEN OR+ MO + EF Combined 35 25% + 50/60 <2 mm – + 25
10 TS-TRS-TTRQ STAGE 2A C OR+ MO + HCS DORSAL 33 83% – 60/60 <2 mm – – 70
11 TS-TRS DORSAL STAGE 1 C OR+ MO + HCS DORSAL 26 43% + 50/50 <2 mm + + 60
12 TR DORSAL STAGE 2A C OR+ MO + HCS + EF + LR DORSAL 24 15% + 60/70 <2 mm – + 30
13 TS DORSAL STAGE 1 C OR+ MO + HCS DORSAL 22 82% – 51/58 <2 mm – – 90
14 TRS DORSAL STAGE 1 C OR+ MO + EF + LR DORSAL 22 84% + 50/54 <2 mm – – 90
15 TRS DORSAL STAGE 2A C CR+ MO 17 75% + 50/60 >2 mm – – 60
16 TR DORSAL STAGE 2B C OR+ MO + HCS Combined 16 30% + 60/70 <2 mm – + 40
17 TR STAGE 2B C CR+ MO 16 40% + 50/66 <2 mm – – 45
TS-TRS: transsacaphoid-trans radial styloid, TS-TTP: trans trans trapezoid, TS: trans scaphoid, TS-TC: trans trans capitate, TS-TRS-TTRQ: trans
scaphoid-trans radial styloid-scaphoid-trans triquetrum, TS-TTRQ-TP: scaphoid-trans scaphoid-scaphoid-trans triquetrum-scaphoid-trans priformis, TR: scaphoid-trans radial, C: closed, OR: open reduction, CR: closed reduction,
MO: minimal osteosynthesis, HCS: headless compression screw, EF: external fixator, LR: ligament reconstruction S-L-A: Scapholunate angle S-L-D: Scapholunate dissociation. SP: Scaphoid pseudoarthrosis C-OCF: Capitate osteochondral fragment.
Fig. 3. Herzberg classified perilunate fracture dislocations according to the
rela-tion of the capitate with the radius. The posirela-tion of the capitate (dorsal or volar) determines the type of dislocation. The relation of lunate and radius is normal in Stage 1 injury but lunate is displaced to the palmar side in Stage 2. In stage 2a ro-tation of the lunate is less than 90° and more in Stage 2b[3].
of perilunate fracture-dislocations depending on the directions and magnitude of the acting forces. Greater arc injuries have worse prognosis [1]. In our study, all patients had greater arc injuries and different types of carpal fractures.
There is no concensus on the treatment of perilunate fracture-dislocations. According to Green, fixation of scaphoid through palmar incision is enough in the treatment of dorsal trans-scaphoid fracture-dislocations and an additional dorsal incision can be used in the case of inadequate reduction of capitolunate joint [8]. Ada et al. pointed the importance of the anatomic reduction and stabilisation of the scapholunate and lunotriquetral ligaments if the scaphoid is intact[1]. Hildebrand et al. perfomed open reduction via combined incisions and repaired scapholunate and lunotriquetral ligaments with suture anchor [9]. Herzberg emphasized the importance of the dorsal proximal raw ligaments and after scaphoid fixation, he recommended perilunate fixation with K-wires which stabilize the radiolunate and triquetrolunate joints. If there is scapholunate ligament injury, he advices to stabilize the scapholunate and lunocapitate joints with K-wires. By this way the author aims to strengthen the relation between proximal and distal raws [10]. Laporte et al. performed open reduction through dorsal incision and stabilize scapholunate, triquetrolunate and scaphocapitate joints with K-wires in their series of 13 dorsal perilunate fracture dislocations[11]. In another study, Chou et al. reported good results with percutaneous screws and K-wires in the treatment of 24 trans-scaphoid perilunate fracture dislocations[12]. In our study we preferred dorsal ap-proach for open reduction in 11 wrists. In two patients median nerve decompression was performed via additional volar incision. In order to preserve continuity of the radioscaphocapitate ligament, radial styloid fixation was performed in 6 patients. We performed scapholunate ligament repair in two patients using suture anchor. The scaphoid is intact and, the scapholunate and lunotriquetral ligaments were torned in 8 cases. The stability of these joints were gained with K-wires in these patients. Concomitant scaphoid fractures were fixed with headless
compres-sion screws (7 wrists) and K-wires (2 wrists). If the injury extended to the distal raw, scaphocapitate fixation was performed. Unilater-al externUnilater-al fixator was applied in two patients for additionUnilater-al stability.
According to Herzberg classification eight patients had stage 1, nine patients (six stage 2a, three stage 2b) had stage 2 injuries in our series. Mean Mayo wrist score was 80.6 (range, 60–90) points in stage 1 patients and 43.3 (range, 25–70) points in stage 2 pa-tients. Although similar treatment protocols were applied to all patients, results in Stage 2 injuries were worse and this maybe cor-related with more extended ligamentous injury[1].
The time between injury and treatment is another prognostic factor. In the study of Herzberg et al., the results of patients who were treated in first week of trauma had better results compared to patients operated later than first week[3]. In another study, pa-tients who were operated in first week of injury had better functional and radiologic results compared to the patients operated after second week[1]. Komurcu et al. reported better results in patient who were operated earlier[13]. Mean time between injury and operation was 1,4 (range:1–3 days) days in our study.
The open fractures are estimated to acoount for 10% of perilunate fracture dislocations and accepted as an important prognostic factor [10]. Herzberg reported significant difference between open and closed injuries (open fractures 11 cases, mean score:57 points; closed fracture 51 cases, mean score: 80 points)[3]. In our study two wrists had open injury (one type 2 and one type 3a) and functional out-comes of these patients were poor. Our findings were compatible with literature.
Although we detected radiocarpal and intercarpal arthrosis in most of the patients radiologically, these findings had no effect on patients’ satisfaction and functional results (Table 2). This was also claimed in the study of Forli and colleagues which consists 18 pa-tients with at least 10 years follow-up[4]. In another study which evaluated 14 patients with trans-scaphoid dorsal perilunate frac-ture dislocations, it was reported that radiologically evident arthrosis may not cause functional disabilities[14]. In our study, 14 out of
17 patients had radiologically obvious posttraumatic arthritis. Mean Mayo scores were found 81 in those who have stage 1 injury with isolated arthritis, however arthritis had no significant effect on the clinical outcomes.
The osteochondral lesions on the head of the capitate can be ac-cepted as an indicator of poor prognosis. It was seen in the 8% of the patients[10,14,15]. Four patients (23%) in our series had os-teochondral lesions on capitate and mean MAYO wrist score of these patients was 38.7 (range, 30–60) points.
It was shown that repair of scapholunate injury may have a key role in terms of good results in long term follow-up[16]. In our study, the patients who had more than and less than 2 mm of scapholunate distance had mean MAYO scores as 51.6 and 62.8 points, respec-tively. We accepted scapholunate dissociation as a factor of poor prognosis.
5. Conclusion
Perilunate fracture dislocations are rare injuries. The mecha-nism of injury should be clarified, staging should be done and treatment should be decided carefully. The anatomic relation between capitatum, lunatum and radius has to be preserved; subluxations in intercarpal joints and fractures of the carpal bones have to be fixed. Despite anatomic reduction, persistent pain can be observed in some patients due to ligamentous and chondral in-juries. The mechanism of injury, concomitant soft tissue damage, and time between the trauma and treatment are prognostic factors for clinical and radiologic results. Stage 1 injuries has good prog-nosis but it should be known that stage 2 injuries may have poor outcomes.
Conflicts of interest
All named authors hereby declare that they have no conflicts of interest to disclose.
Funding
This research received no specific grant from any funding agency in the public commercial, or not-for-profit sectors.
Ethical approval
None.
Author contribution
Adnan Kara-study design, data collections, writing, Final corrections.
Haluk Celik - study design, data analysis, writing, Final corrections. Ali Seker-data analysis, writing.
Bekir Eray Kilinc-data collections, data analysis. Savas Camur-data collections, data analysis. Metin Uzun-data analysis, writing, Final corrections. All authors approve final version of paper for submission.
Guarantor
Adnan Kara, Haluk Celik.
References
[1] S. Ada, F. Ozerkan, A. Bora, Y. Ademoglu, I. Kaplan, The results of surgical treatment of perilunate fracture-dislocations, Acta Orthop. Traumatol. Turc. 29 (1995) 263–267.
[2] M.S. Moneim, Management of greater arc carpal fractures, Hand Clin. 4 (1988) 457–467.
[3] G. Herzberg, J.J. Comtet, R.L. Linscheid, P.C. Amadio, W.P. Cooney, J. Stalder, Perilunate dislocations and fracture-dislocations: a multicenter study, J. Hand Surg. Am. 18 (1993) 768–779.
[4] A. Forli, A. Courvoisier, S. Wimsey, D. Corcella, F. Moutet, Perilunate dislocations and transscaphoid perilunate fracture-dislocations: a retrospective study with minimum ten-year follow-up, J. Hand Surg. Am. 35 (2010) 62–68.
[5] J.K. Mayfield, Mechanism of carpal injuries, Clin. Orthop. Relat. Res. 149 (1980) 45–54.
[6] O. Soejima, H. Iida, M. Naito, Transscaphoid-transtriquetral perilunate fracture dislocation: report of a case and review of the literature, Arch. Orthop. Trauma Surg. 123 (2003) 305–307.
[7] P.M. Murray, Dislocations of the wrist: carpal instability complex, J.Hand Surg. Am. 3 (2003) 88–99.
[8] D.P. Green, Carpal dislocations and instabilities, in: D.P. Green (Ed.), Operative Hand Surgery, second ed., Churchill Livingstone, New York, 1988, pp. 875–938. [9] K.A. Hildebrand, D.C. Ross, S.D. Patterson, J.H. Roth, J.C. MacDermid, G.J. King, Dorsal perilunate dislocations and fracture-dislocations: questionnaire, clinical, and radiographic evaluation, J. Hand Surg. Am. 25 (2000) 1069–1079. [10] G. Herzberg, Acute dorsal trans-scaphoid perilunate dislocations: open reduction
and internal fixation, Tech. Hand Up. Extrem Surg. 4 (2000) 2–13.
[11] M. Laporte, A. Michot, H. Choughri, M.L. Abi-Chahla, P. Pelissier, Perilunate dislocations and fracture-dislocations of the wrist, a review of 17 cases, Chir. Main. 31 (2012) 62–70.
Fig. 5. The progression of injury from radial to the ulnar sides according to the Mayfield classification. In each step a new ligamentous injury or bone fracture occurs. a)
[12]Y.C. Chou, Y.H. Hsu, C.Y. Cheng, C.C. Wu, Percutaneous screw and axial Kirschner wire fixation for acute transscaphoid perilunate fracture dislocation, J. Hand Surg. Am. 37 (2012) 715–720.
[13]M. Komurcu, M. Kurklu, K.E. Ozturan, M. Mahirogullari, M. Basbozkurt, Early and delayed treatment of dorsal transscaphoid perilunate fracture-dislocations, J. Orthop. Trauma 22 (2008) 535–540.
[14]G. Herzberg, D. Forissier, Acute dorsal trans-scaphoid perilunate fracture-dislocations: medium-term results, J. Hand Surg. Br. 27 (2002) 498–502. [15]C.P. Melone Jr., M.S. Murphy, K.B. Raskin, Perilunate injuries. Repair by dual
dorsal and volar approaches, Hand Clin. 16 (2000) 439–448.
[16]W.M. Weil, J.F. Slade 3rd, T.E. Trumble, Open and arthroscopic treatment of perilunate injuries, Clin. Orthop. Relat. Res. 445 (2006) 120–132.