REVISTA
BRASILEIRA
DE
ANESTESIOLOGIA
OfficialPublicationoftheBrazilianSocietyofAnesthesiologywww.sba.com.br
SCIENTIFIC
ARTICLE
Effect
of
low
dose
dexmedetomidine
premedication
on
propofol
consumption
in
geriatric
end
stage
renal
disease
patients
Pinar
Ergenoglu
∗,
Sule
Akin,
Cagla
Bali,
Hatice
Evren
Eker,
Oya
Yalcin
Cok,
Anis
Aribogan
BaskentUniversitySchoolofMedicine,AnesthesiologyandReanimationDepartment,Adana,TurkeyReceived17September2014;accepted11November2014 Availableonline2May2015
KEYWORDS
Geriatricpatient; Endstagerenal disease;
Dexmedetomidine; Propofol
Abstract
Backgroundandobjective: Sedation in dialysis dependent end-stage renal disease patients requirescautionasaresultofperforminghighdosesofsedativesanditscomplications. Mul-tidrugsedationregimensmightbesuperiorandadvantageonlesserdrugconsumptionandby thewayadverseeventswhichoccureasilyinend-stagerenaldiseasepatients.Weevaluated theeffectsofdexmedetomidinepremedicationonpropofolconsumption,sedationlevelswith Observer’sAssessmentofAlertnessandSedationscoresandthebispectralindexandthe hemo-dynamicchanges,potentialsideeffectsingeriatricpatientswithend-stagerenaldiseasewho underwenthipfracturesurgeryunderspinalanesthesia.
Method: Inthisrandomized,controlled,double-blindstudy60elderlypatients(age≥65years) withend-stagerenaldiseaseandhipfracturescheduledforanterogradefemoralintramedullary nailing were assigned to groups that received either intravenous saline infusion (Group C) ordexmedetomidine0.5g/kg/10mininfusionforpremedication(GroupD).Allthepatients receivedpropofolinfusionaftertheinductionofthespinalanesthesia.
Results:Total propofol consumption, propofol dose required for targeted sedation levels accordingtoObserver’sAssessmentofAlertnessandSedationscoresandbispectralindexlevels, recoverytimesweresignificantlylowerinGroupD(p<0.001).ThetimetoreachtoObserver’s AssessmentofAlertnessandSedationscore4andtoachievebispectralindex≤80was signi-ficantlylowerinGroupCcomparedwithGroupD(p<0.001).Adverseeventsweresimilarin bothgroups.
Conclusion:Dexmedetomidinepremedication lowersintraoperative propofolconsumptionto maintaintargetedlevelofsedation.Thereforelowdosedexmedetomidinepremedicationin additiontopropofolinfusionmightbeanalternativeingeriatricpatientswithend-stagerenal diseaseforsedation.
©2015SociedadeBrasileiradeAnestesiologia.PublishedbyElsevier EditoraLtda.Allrights reserved.
∗Correspondingauthor.
E-mail:pergenoglu@yahoo.com(P.Ergenoglu).
http://dx.doi.org/10.1016/j.bjane.2014.11.002
PALAVRAS-CHAVE
Pacientegeriátrico; Doenc¸arenalem estágioterminal; Dexmedetomidina; Propofol
Efeitodapré-medicac¸ãocomdosebaixadedexmedetomidinasobreoconsumode propofolempacientesgeriátricoscomdoenc¸arenalemestágioterminal
Resumo
Justificativaeobjetivo: Asedac¸ãoempacientedependentedediálisecomdoenc¸arenalem estágioterminal(DRET)requercautelacomoresultadodaadministrac¸ãodealtasdosesde seda-tivosesuascomplicac¸ões.Osregimesdesedac¸ãocommúltiplasdrogaspodemsersuperiorese vantajososemrelac¸ãoaoconsumomenordedrogaseaoseventosadversosqueocorrem facil-menteempacientescomDEET.Avaliamososefeitosdapré-medicac¸ãocomdexmedetomidina sobreoconsumodepropofol,osníveisdesedac¸ãocomosescoresdaObserver’sAsssessment ofAlertnessandSedation(OAA/S)edoíndicebispectral(BIS),asalterac¸õeshemodinâmicase ospotenciaisefeitoscolateraisempacientesgeriátricoscomDRETsubmetidosàcirurgiapara fraturadequadrilsobraquianestesia.
Método: Neste estudorandômico, controlado eduplo-cego, 60 pacientesidosos(idade≥65 anos),comDRETefraturadequadril,agendadosparafixac¸ãointramedulardehastefemoral anterógradaforamdesignadosparagruposparareceberaminfusãointravenosadesoluc¸ãosalina (GrupoC)oupré-medicac¸ãocominfusãode0,5mgkg/10mindedexmedetomidina(DEX)(Grupo D).Todosospacientesreceberaminfusãodepropofolapósainduc¸ãodaraquianestesia.
Resultados: Oconsumototaldepropofol,adosedepropofolnecessáriaparaosníveis-alvode sedac¸ãodeacordocomosescoresdaOAA/S,osvaloresdoBISeostemposderecuperac¸ão foramsignificativamentemenoresnoGrupoD(p<0,001).Otempoparaatingiroescore4na OAA/SevaloresBIS≤80foisignificativamenteinferiornoGrupoCemcomparac¸ãocomoGrupo D(p<0,001).Oseventosadversosforamsemelhantesemambososgrupos.
Conclusão:Apré-medicac¸ãocomdexmedetomidinareduzoconsumodepropofolno intraoper-atórioparamanteronível-alvodesedac¸ão.Portanto,apré-medicac¸ãocomDEXemdosebaixa emcombinac¸ãocominfusãodepropofolpodeserumaalternativaparasedac¸ãoempacientes geriátricoscomDRET.
©2015SociedadeBrasileira deAnestesiologia.PublicadoporElsevierEditoraLtda.Todosos direitosreservados.
Introduction
Theincidenceofendstagerenaldiseaseanddialysis pop-ulation inthe elderly continuestoincrease universally.1---3 Hip fractures are also major problem and the anesthesia techniqueshouldbeplannedindetailduetopotential alter-ations in volume distribution, protein binding, and drug metabolismandexcretion.4---6Inanidealanesthesiaregime, themostimportantparametersareprovidinghemodynamic stability withoptimalfluid andelectrolyte balance, using drugs withalowermetabolism, shorter half-lifeand non-renal clearance, targeting early recovery and return of cognitiveandpsychomotorfunctions.7
Neuraxial techniques such as single spinal injection is frequently performed for the intraoperative anesthesia managementofpatientswithchronicrenalfailure.8 Coad-ministration of spinal anesthesia and sedation became a standard protocol for providing patients’ anxiolysis and amnesiaat theintraoperativeperiod.9 Propofolisthe fre-quently used agent and combination regimens such as propofol vs alfentanil or midazolam vs fentanyl for seda-tion are commonly used in patients with chronic renal failure.10,11Thesedoanalgesiadrugdosesshouldbetitrated and to reduce dose consumption combination regimens shouldbeperformedinhemodialysispatients.12
Dexmedetomidine (DEX)is aselective␣2receptor ago-nistagent,mightbeanalternativeofchoiceforcombination regimen with propofol due to its sedative and analgesic
propertieswithminimaleffectsonventilation.13Thereare limitednumber of studies investigating the effectof DEX in patients withend stage renal disease (ESRD),however thesestudies are not specific to geriatric patients at the sametime.14,15
In this study we evaluate the effects of dexmedeto-midine premedication on propofol consumption, sedation levels,hemodynamicchanges,potentialsideeffectsin geri-atricpatientswithESRDwhounderwenthipfracturesurgery underspinalanesthesia.
Materials
and
methods
This study was approved by the Baskent University Insti-tutional Review Board and EthicsCommittee (Project no: KA12/166).Afterobtainingwritteninformedconsentfrom thepatients,60elderlypatients(age≥65years)withend stage renal failure on dialysis treatment (glomerular fil-tration rate<15, Stage 5) and hip fracture scheduled for anterogradefemoralintramedullarynailingwereincludedin thisdouble-blind,randomized, controlledstudy.Exclusion criteriaweredecompensated respiratoryor heartfailure, liverfailure,obesity (bodymassindex>30), mental disor-ders,cognitivedisorders,languageproblems,patientswith a contraindication for regional anesthesia (coagulopathy, historyofanticoagulantuse,spinalcorddiseaseandpatients
whorejectedspinalanesthesia)andhistoryofallergytoany medicationsusedinthisstudy.
The randomization scheme was developed by a com-puter and covered in sealed envelopes. These envelopes werepreparedbyanindependentanesthesiologistwhowas notassociatedwiththestudy.Theenvelopeswereopened bytheanesthesiatechnician,whoalsopreparedthestudy drugs.
Patientswererandomlydividedintotwogroups: Group control (Group C): Saline infusion for premedi-cation, midazolam 0.02mg/kg; spinal block (hyperbaric bupivacaine0.5%,12.5mg,n=30).
GroupDEX(GroupD):0.5g/kg/10mindexmedetomidine infusionforpremedication,midazolam0.02mg/kg;spinal block(hyperbaricbupivacaine0.5%,12.5mg,n=30).
The study drugs were brought to the operation the-aterbytheanesthesiatechnician.Theanesthesiologistwho performed premedications, spinal anesthesia, intraopera-tivepostoperativefollow-upsanddatarecordingswasalso blindedtothestudydrugsandgroupallocation.
Aperipheralintravenouslinewasplacedusingan18---20 gauge catheter in patients. Patients arrived in the oper-ation theater without premedication. Routine anesthesia monitoringwasperformedwithpulse-oxymeter,5-leadECG, noninvasiveblood pressure measurement,pulse oxymetry andBIS.BISscoresweremeasuredusinganAspectBISVista Monitor(AspectMedicalSystems,Inc).Electroencefalogram (EEG)wasrecordedusingBISQUATROTMsensorstucktothe
preparedforeheadskinasexplainedintheinstructions.All thepatientsreceived0.02mg/kgmidazolam.0.5g/kgDEX in20mLwasadministeredin10minwithaninfusionpump. An equivalent volumeof saline solution was given tothe controlgroupbyusingthesamemethod.Baseline,1-,5-, 10-minuteOAA/Sscores,BIS,peripheraloxygensaturation (SpO2),heartrate(HR),systolicbloodpressure(SBP),
dias-tolic blood pressure (DBP) values were recorded. At this period 250mL of 0.9% NaCl was infused. Basal SBP, DBP, HR, SpO2, BIS values were recorded before induction of
thespinalblock.Lumbarpuncturewasperformedinlateral decubitis position with a Quincke® 27 gauge spinal
nee-dleat theL3---L4 interspaces using the midline approach. Patients were promptly rotated to supine position after
blockinduction.Inductionofthespinalblockwasaccepted astimeof0forallintraoperativedatarecordings.All param-eterswere recordedat 1-,5-min andevery 5min for the firsthour and followingthe firsthour every 15min during surgery.
Hypotension was described as ≥25% decrease in SBP fromthebaselineor incaseswhensystolicbloodpressure decreases below 90mmHg. Ephedrine 5mg was adminis-teredintravenouslyandtherateofcrystalloidinfusionwas increased.
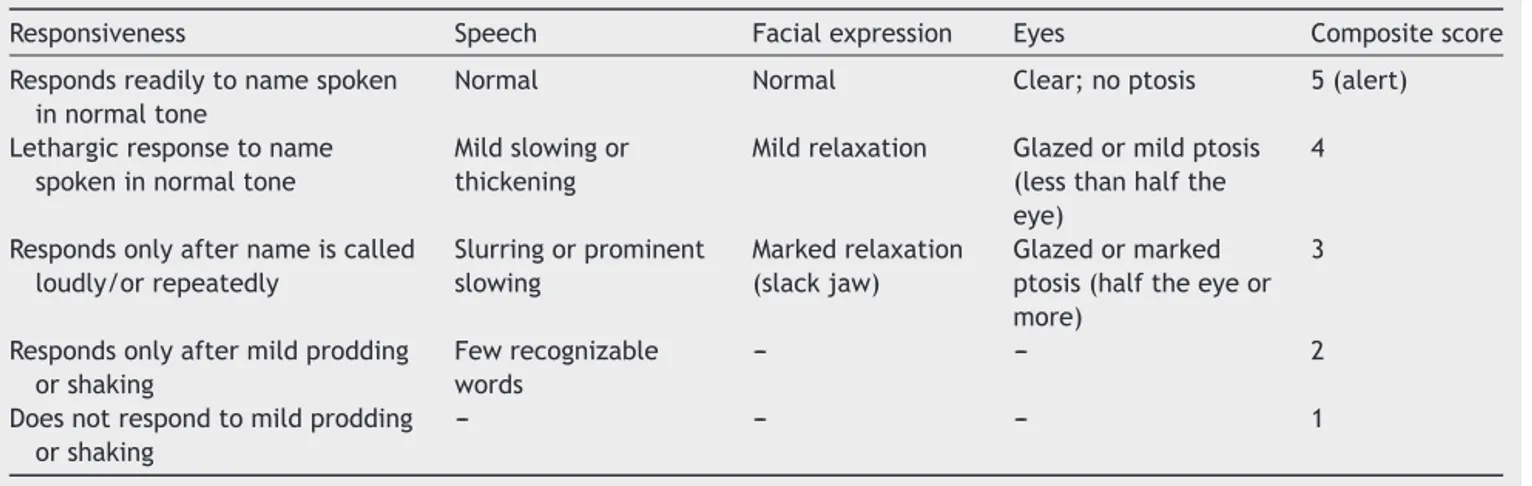
Thesensorialblocklevelandthemotorblocklevelwere assessedbypinpricktestandmodifiedBromagescale(0=no motor block, 1=hip flexion with extended leg blocked, 2=kneeflexionblocked,3=completemotorblock), respec-tively.TimetoreachthelevelofT10andtoBromage3was alsonoted.Propofolinfusionwasstartedinallthepatients atadose of50mcg/kg/minafterthelevelofblockarised toT10dermatome level.OAA/S scalewasusedfor evalu-atingthelevelofsedation16 (Table1).Intermittent0.5mL bolus doses of propofolwere givenfor reaching totarget OAA/S scores andBISlevelsat thebeginning ofthe seda-tionifnecessary.Sedativeagent(DEXvspropofol)infusion startingtimewasaccepted as0pointfor therecordingof thetimetoreachtoOAA/Sscore4andthetimetoreachto BIS≤80.TargetBISvalueswerebetween70and80.Infusion rate wastitrated according tothe targetedOAA/S scores andBISlevels.IncaseOAA/Sscore<4andBIS<70,propofol infusionratewasreduced.Propofolinfusionwasstoppedat thebeginningofskinsuturing.
Patientsweremonitoredatthepostoperativecareunit and all monitoring parameters were registered at every 5min for 1h. Criteria for transferring the ward were OAA/S=5,BIS>90,Bromage=0---1.
Totalpropofolconsumption,timenecessarytoreachthe targeted level of sedation (OAA/S score 4 and BIS≤80), propofol dose required for targeted OAA/S score and BIS levels,recoverytime(BIS>90),durationofsurgery,amount of bleeding, vasoactive drug need were recorded. Pos-sible side effects and possible complications during the preoperative, intraoperativeperiodand thepostoperative follow-upsuchashypotension(SBP<90mmHg),bradycardia (HR<60min),respiratorydepression(SpO2≤90%),nausea,
vomiting,anddeepsedationwerecarefullymonitoredand recorded.
Table1 Theobserver’sassessmentofalertness/sedationscore.
Responsiveness Speech Facialexpression Eyes Compositescore
Respondsreadilytonamespoken innormaltone
Normal Normal Clear;noptosis 5(alert)
Lethargicresponsetoname spokeninnormaltone
Mildslowingor thickening
Mildrelaxation Glazedormildptosis (lessthanhalfthe eye)
4
Respondsonlyafternameiscalled loudly/orrepeatedly Slurringorprominent slowing Markedrelaxation (slackjaw) Glazedormarked ptosis(halftheeyeor more)
3
Respondsonlyaftermildprodding orshaking
Fewrecognizable words
--- --- 2
Doesnotrespondtomildprodding orshaking
Statistical
analysis
Statisticalanalysiswasperformedusingthestatistical pack-age SPSS (Version 17.0, SPSS Inc., Chicago, IL, USA). The primary outcome of this study was total propofol con-sumptionduringthehipfracturesurgery.Apoweranalysis indicatedthat26patientspergroupwererequiredtodetect atruedifferenceof40mgbetweengroupswherethe antici-patedstandarddeviationwas43.16.Thestandarddeviation wasbasedonapilotgroupofpatientsundergoinghip frac-ture surgery. The type 1 error was set at 0.05 and type II error at 0.10. We allowed for 4 more patients in each groupstocompensatefordropoutsduringthestudyperiod. For each continuous variable, normality was checked by Kolmogorov---Smirnov and Shapiro---Wilk tests and by his-tograms.Independentsamplest-testandtheMann---Whitney
U-test were performed for between-groups comparisons where appropriate. Pre-post measures were analyzed by RepeatedMeasureAnalyses.Valuesofp<0.05were consid-eredtobestatisticallysignificant.
Results
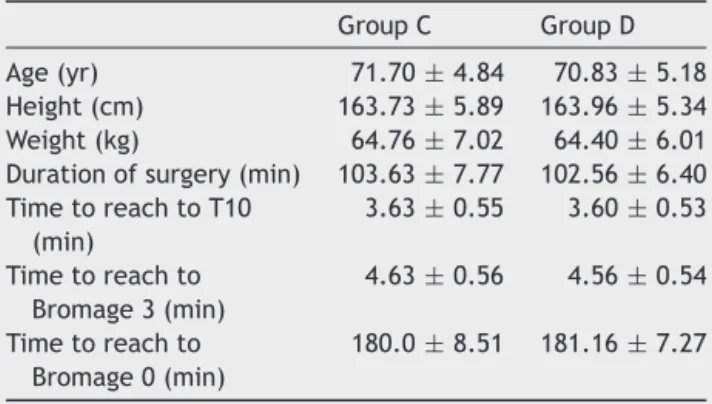
Sixty-hemodialysisdependentchronicrenalfailurepatient scheduledforhipfracturerepairwereenrolledinthestudy. Fig. 1 presents the allocation of patients in groups. The groupswerecomparablewithrespecttodemographicdata, durationofsurgery,timetoreachtoT10,toBromage3and toBromage0(Table2).
Total propofol consumption, propofol dose required for targeted sedation levels and recovery time were
Table2 Demographicdataandblockcharacteristics. GroupC GroupD
Age(yr) 71.70±4.84 70.83±5.18
Height(cm) 163.73±5.89 163.96±5.34 Weight(kg) 64.76±7.02 64.40±6.01 Durationofsurgery(min) 103.63±7.77 102.56±6.40 TimetoreachtoT10 (min) 3.63±0.55 3.60±0.53 Timetoreachto Bromage3(min) 4.63±0.56 4.56±0.54 Timetoreachto Bromage0(min) 180.0±8.51 181.16±7.27 Dataexpressedasmean±SD.
significantlylowerinGroup D whencomparedwithGroup C(p<0.001).Thetimetoachievetotargetedsedation lev-elsaccordingtoOAA/SscoreandBISlevelswassignificantly lowerin Group C comparedwith Group D (p<0.001). All thepatientsin GroupD achievedtargetedsedation levels withonly DEX infusion without propofol infusion require-ment(Table3).
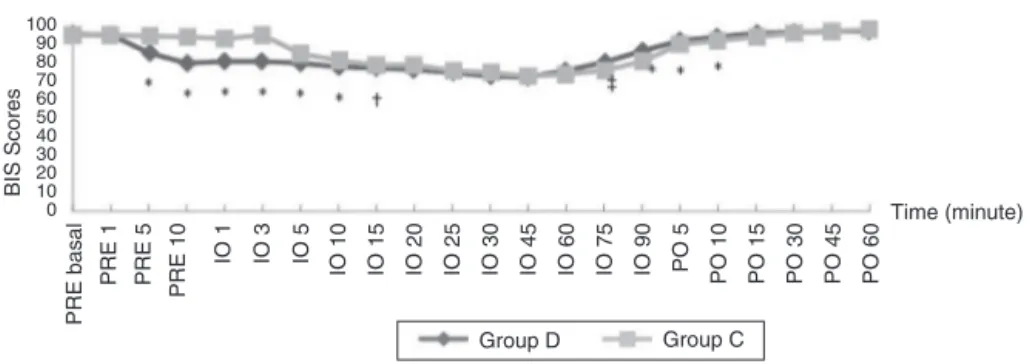
ComparisonofpreoperativeOAA/SandBISscoresshowed that the scores were significantly lower in Group D com-paredwithGroup Cat preoperative5thand10thminutes (p<0.001).Intraoperative OAA/Sscoresat 1-,3-,5-,10th minutesandintraoperativeBISscoresat1-,3-,5-,10-,15th minutesweresignificantlylowerinGroupDcomparedwith GroupC(p<0.05).The scoresweresimilarinboth groups till75thminutesandweresignificantlylowerat75th,90th minutesingroupC(p<0.05)(Figs.2and3).Postoperative
Enrollment
Randomized (n=60)
Allocation
Follow-Up
Analysis
Assessed for eligibility (n=60)
Excluded (n=0)
Allocated to control group (n=30)
♦ Not meeting inclusion criteria (n=0) ♦ Declined to participate (n=0) ♦ Other reasons (n=0)
♦ Received allocated intervention (n=30) ♦ Did not receive allocated intervention (n=0)
Allocated to Dexmedetomidine group (n=30)
♦ Received allocated intervention (n=30) ♦ Did not receive allocated intervention (n=0)
♦ Excluded from analysis (n=0)
Lost to follow-up (n=0) Discontinued intervention (n=0) Lost to follow-up (n=0)
Discontinued intervention (n=0)
Analysed (n=30)
♦ Excluded from analysis (n=0)
Analysed (n=30)
100 90 80 70 60 50 40 30 20 10 0 BIS Scores Time (minute) Group D Group C PRE basal PRE 1 PRE 5 PRE 10 IO 1 IO 3 IO 5 IO 10 IO 15 IO 20 IO 25 IO 30 IO 45 IO 60 IO 75 IO 90 PO 5 PO 10 PO 15 PO 30 PO 45 PO 60
Figure2 BISvaluesofthepatients.Valuesgivenaremedian(*p<0.001;†p=0.001;‡p=0.002).
Table3 Sedationdata.
GroupC GroupD p Timetoachieve BIS≤80(min) 5.08±0.51 7.65±1.49 <0.001 Timetoreachto OAA/Sscore4 (min) 4.03±0.45 5.28±0.85 <0.001
Propofoldosefor BIS≤80(mg) 37.17±5.83 0.00±0.00 <0.001 Totalpropofol consumption(mg) 197.0±50.08 82.0±23.03 <0.001 Recoverytime (BIS≥90)(min) 16.73±1.84 7.30±1.52 <0.001 Dataexpressedasmean±SD.
OAA/S scores were similarbetween groups (Fig. 3). Post-operative BIS scores were significantly lower at 5-, 10th minutes in Group C (p<0.001); but was similar between groupsafterthe10thminutes(Fig.2).
Theheartrate,SBP,DBP,SpO2showeddecreaseatGroup
D but there were no significant differences among two groups.Hypotensionwasobservedat8patientsinGroupD and9patientsinGroupC;bradycardiaobservedat6patients inGroupDand5patientsinGroupCduringthe intraopera-tiveperiod.Howeverthedifferencebetweenthegroupswas notstatisticallysignificant.None ofthepatientsexhibited respiratorydepression,nauseaandvomiting.
Discussion
In this study we showed that in geriatric patients with chronicrenalfailuresedationregimenwithDEX premedica-tionreducestotalpropofolconsumptionwithrapidrecovery time(GroupC:16.73±1.84min;GroupD:7.30±1.52min). Ontheotherhand,accordingtothepharmacokinetic prop-ertiesthetimerequiredtoattaintheaimedlevelofsedation wassignificantlyshorterwithpropofolinthecontrolgroup (5.08±0.51min)incomparisonwiththeDEXpremedication (7.65±1.49min).
Propofolisanultrafastagentwithapeakeffectwithin 5minofadministrationandisusedforsedationoranesthesia maintenance.17,18Ithasbeenreportedthatthe pharmacoki-neticsofbolusorinfusiondosesarenotaffectedmarkedly andcanbeusedsafelyinESRDpatients.19,20DEXisahighly selective␣2adrenoceptoragonistdrugwithsedative, sym-patholytic,andanalgesicactions.Itismetabolizedintoits inactivemetabolitesinliveranditseliminationisunaffected byrenaldisease.Byvirtueoftheseproperties,itmayoffer analternativeoptionforsedationinESRDpatients.15,21Ithas also been reportedthat it does not exert any respiratory depressant effectevenin highdoses,anditcanbesafely usedforsedationinveryelderlypeople.22
Dose determination studies for DEX in patients with chronic renal failure have demonstrated that the drug providedsufficientsedationwithanysignificantsideeffect at a dose of 0.6g/kg/10min in volunteer patients aged 18to65yearswithcreatinineclearanceof<30.15 Wealso
5 4 3 2 1 0 O AA/S Scores Time (minute) Group D Group C PRE basal PRE 1 PRE 5 PRE 10 IO 1 IO 3 IO 5 IO 10 IO 15 IO 20 IO 25 IO 30 IO 45 IO 60 IO 75 IO 90 PO 5 PO 10 PO 15 PO 30 PO 45 PO 60
Figure3 OAA/Sscoresofthepatients.Valuesgivenaremedian(*p<0.001;†p=0.001).PRE,preoperative;Io,intraoperative; PO,postoperative.
attainedthedesiredsedationlevelwithoutanysignificant hemodynamicresponseorsideeffectwithsimilar premed-icationdosesofDEX(0.5gr/kg/10min).Alsoweobserved thatallthepatientsinGroupDreachedtargetedsedation levels following preoperative DEX infusion without any propofolrequirement.
IthasbeenreportedthatDEXusedasanadditiveagent decreasespropofolconsumption.23Alsoinourstudya propo-foldosetitrationwasperformedafterDEXpremedicationfor sedationwiththeguidanceofOAA/SandBISmonitoring.It wasdemonstratedthatpropofolconsumptionwas2.4-fold greaterthanthestudygroup(197.0mgvs82.0mg)andthus the recovery period was2.29 times longerin the control group(16.73minvs7.30min).Accordingtotheseresults,it maybesuggested thatthelowerOAA/S andBIS scoresat 75and90minattheintraoperativeperiodaswellaslower BISscoresandasignificantlylongerrecoverytimeat5and 10minatthepostoperativeperiodobservedinthecontrol groupwereassociatedwithahigherpropofolconsumption, andthusdexmedetomidinehadanimportanteffecton post-operativeearlyrecovery.
One other parameter that should be taken into con-sideration is the hemodynamic response. In addition to sympatholyticeffectsofspinalanesthesia,anadditive inter-actionwithcardiovasculareffectsofDEXandpropofolmay be possible. DEX is known to have some cardiovascular effectsincludinghypotensionandbradycardia owingtoits sympatholyticeffects.However,ithasbeen reportedthat itoffersagoodcardiovascularstabilityandthusitisagood sedativeagent.24,25
In a study comparing sedation application with dexmedetomidine or midazolam in ESRD patients it was reportedthatnoneof thepatientsexperienced prolonged hypotensionor bradycardia,allrespondedsatisfactorilyto thetreatment,andnoneof themwereexcludedfromthe study even with large loading doses of 1g/kg/10min of dex.14 Wealsodidnotdemonstrateasignificantlydifferent hemodynamicresponsetoDEXloadedatadoseof0.5g/kg compared to the control group. However, both groups developedintraoperativehypotension(GroupC,30%;Group D, 26.7%) and bradycardia (Group C, 16.7%; Group D, 20%) after propofolinfusion, which quickly resolvedupon administrationofsympathomimetics.Thisresponsemaybe an additiveresultofthe venodilatativeeffectof propofol and the sympatholytic effect of spinal anesthesia rather thantheeffectofDEX.
In thepresentstudy wefound thatpremedicationwith DEX at a dose of 0.5g/kg for 10min attained sufficient and aimed sedation levels without propofol requirement during the preoperative period. DEX premedication also reducedintraoperativepropofolconsumption, significantly promoted earlyrecovery andwasnotthe causeofsevere side effects.In conclusion, we believethat low dose DEX premedicationinadditiontopropofolinfusionmightbean alternativeregimeningeriatricpatientswithESRDfor seda-tion.
Conflicts
of
interest
Theauthorsdeclarenoconflictsofinterest.
Acknowledgement
This study was supported by Baskent University Research Fund(BaskentUniversityInstutionalReviewBoardandEthics Committee,ProjectnumberKA12/166).
Trial registration: Clinicaltrials.gov identifier NCT01837290.
References
1.IsmailN,HakimRM,OreopoulosDG,etal.Renalreplacement therapiesintheelderly:Part1.Hemodialysisandchronic peri-tonealdialysis.AmJKidneyDis.1993;22:759---82.
2.KeithDS. Transplantationintheelderly patient.ClinGeriatr Med.2013;29:707---19.
3.SasakiY,MarioniR,KasaiM,etal.Chronickidneydisease:a riskfactorfordementiaonset:apopulation-based studyThe Osaki-TajiriProject.JAmGeriatrSoc.2011;59:1175---81. 4.Le-WendlingL,BihoracA,BaslantiTO,etal.Regional
anesthe-siaascomparedwithgeneralanesthesiaforsurgeryingeriatric patientswithhipfracture:doesitdecreasemorbidity, mortal-ity,andhealthcarecosts?Resultsofasingle-centeredstudy. PainMed.2012;13:948---56.
5.Jørgensen TSH, Hansen AH, Sahlberg M, et al. Falls and comorbidity:thepathwaytofractures.ScandJPublicHealth. 2014;42:287---94.
6.TrainorD,BorthwickE,FergusonA.Perioperativemanagement ofthehemodialysispatient.SeminDial.2011;24:314---26. 7.ByrickRJ.Anesthesiaand endstagerenal failure:isTIVAan
advance?CanJAnaesth.1999;46:621---2.
8.Hadimioglu N, Ulugol H, Akbas H, et al. Combination of epidural anesthesia andgeneral anesthesia attenuatesstress response to renal transplantation surgery. Transplant Proc. 2012;44:2949---54.
9.BrownDL.Spinal,epidural,andcaudal anesthesia.In:Miller RD,editor.Miller’sanesthesia.ElsevierHealthSciences;2010. p.1612---27.
10.EddlestonJM,PollardBJ,BladesJF,etal.Theuseofpropofolfor sedationofcriticallyillpatientsundergoinghaemodiafiltration. IntensiveCareMed.1995;21:342---7.
11.LeeSM,KimGH,LeeJJ,etal.Doespropofoland alfentanil-inducedsedationcauseperiodicapnoeainchronicrenalfailure patients?IntJClinPract.2010;64:1---5.
12.Beathard GA, Urbanes A, Litchfield T, et al. The risk of sedation/analgesiainhemodialysispatientsundergoing inter-ventionalprocedures.SeminDial.2011;24:97---103.
13.OkHG,BaekSH,BaikSW,etal.Optimaldoseof dexmedetomi-dineforsedationduringspinalanesthesia.KoreanJAnesthesiol. 2013;64:426---31.
14.RutkowskaK,KnapikP,MisiolekH.Theeffectof dexmedeto-midine sedation on brachial plexus block in patients with end-stagerenaldisease.EurJAnaesthesiol.2009;26:851---5. 15.DeWolfAM,FragenRJ,AvramMJ,etal.Thepharmacokinetics
of dexmedetomidinein volunteers withsevererenal impair-ment.AnesthAnalg.2001;93:1205---9.
16.BagchiD,MandalMC,DasS,etal.Bispectralindexscoreand observer’sassessmentofawareness/sedationscoremay mani-festdivergenceduringonsetofsedation:studywithmidazolam andpropofol.IndianJAnaesth.2013;57:351---7.
17.Lundström S, TwycrossR, MihalyoM, et al. Propofol.J Pain SymptomManage.2010;40:466---70.
18.Fechner J, Ihmsen H, Hatterscheid D, et al. Comparative pharmacokinetics and pharmacodynamics ofthe new propo-folprodrugGPI15715andpropofolemulsion.Anesthesiology. 2004;101:626---39.
19.IckxB,CockshottID,BarvaisL,etal.Propofolinfusionfor induc-tionandmaintenanceofanaesthesiainpatientswithend-stage renaldisease.BrJAnaesth.1998;81:854---60.
20.Kakinohana M, Tokumine J, Kawashima S, et al. Patient-controlled sedation using propofol in eight patients with endstagerenalfailure.JAnesth.2004;18:39---42.
21.Gertler R, BrownHC, Mitchell DH,et al. Dexmedetomidine: anovelsedative-analgesic agent.Proc(BaylUnivMedCent). 2001;14:13---21.
22.Kunisawa T, HanadaS, Kurosawa A, etal. Dexmedetomidine wassafelyusedforsedationduringspinalanesthesiainavery elderlypatient.JAnesth.2010;24:938---41.
23.SenS,ChakrabortyJ,SantraS,etal.Theeffectof dexmedeto-midine infusionon propofolrequirementfor maintenance of optimumdepthof anaesthesiaduringelectivespine surgery. IndianJAnaesth.2013;57:358---63.
24.HallJE,UhrichTD,BarneyJA,etal.Sedative,amnestic,and analgesicpropertiesofsmall-dosedexmedetomidineinfusions. AnesthAnalg.2000;90:699---705.
25.BajwaS,KulshresthaA.Dexmedetomidine:anadjuvantmaking largeinroadsinto clinicalpractice. AnnMedHealth Sci Res. 2013;3:475---83.