The aim of this study was to compare the clinical and radiological results of InterTan nail and proximal femoral nail antirotation (PFNA) in the treatment of reverse intertrochanteric fractures (AO/OTA 31-A3). The study included a total of consecutive patients who presented at trauma centre with a reverse intertrochanteric fracture between in the last 7 years. Treatment was applied with PFNA in 33 patients and with InterTan nail in 36. Evaluation was made from the radiographs taken on postoperative day 1 and at the final follow-up examination of changes in the femoral neck and shaft angulation, measurement of telescoping of blade and lag screws and reduction quality. The mean telescoping was measured as 7.21±7.13mm in the PFNA group and 4.18±4.32 mm in the InterTan group (p = 0.039). Mechanical failure was seen in 8 (24.2%) cases in the PFNA group and in one case of the InterTan group. Cut-out was observed in 4 cases of the PFNA group and in none of the InterTan group. No statistically significant difference was determined between the groups in respect of time to union and functional scores (p = 0.573 and p = 0.294). The use of InterTan nailing in the fixation of reverse intertrochanteric fractures provided better clinical and radiological results compared to PFNA in terms of less telescoping, less change in the neck shaft angle and lower complication rates.
Keywords : reverse trochanteric fracture ; intramedullary nail ; complication ; proximal femoral nail antirotation.
INTRODUCTION
The incidence of fractures in the intertrochanteric region is increasing because of high-energy traffic accidents in young adults (16,21). Intertrochanteric fractures are grouped in the AO/OTA classification as simple (31-A1), multi-fragmentary (31-A2) and reverse (31-A3). Reverse fractures have their own specific mechanical characteristics and are considered to be more unstable than the other types
(16,21). Where the integrity of the lateral femoral wall is impaired in these fractures, it is recommended that treatment is made with intramedullary nails which prevent lateral sliding of proximal fragment and medialisation of the shaft rather than dynamic hip screws (7, 12,15, 21).
A comparison of the InterTan nail and proximal femoral fail
antirotation in the treatment of reverse intertrochanteric femoral fractures
Ahmet İmerci, Nevres H. Aydogan, Kursad Tosun
From the Mugla Sitki Kocman University, Faculty of Medicine, Mugla, Turkey
n Ahmet Imerci1. n Nevres H. Aydogan1.
n Kursad Tosun2.
1Mugla Sitki Kocman University, Faculty of Medicine,
Department of Orthopaedics and Traumatology, Mugla, Turkey.
2Mugla Sitki Kocman University, Faculty of Medicine,
Department of Biostatistics, Mugla, Turkey
Correspondence : Ahmet Imerci; Mugla Sitki Kocman University, Faculty of Medicine, Department of Orthopaedics and Traumatology, Mugla, Turkey phone:+90 506 893 52 76 Fax; +90 252 211 13 45 ; Address: Karamehmet Mah. 19 sokak No:10 A blok daire:9 Mentese/Mugla.
E-mail : ahmetimerci@hotmail.com © 2018, Acta Orthopaedica Belgica.
Many brands of nail with different mechanical properties are on the market for use in the treatment of proximal femoral fractures. The PFNA device (Synthes, Oberdorf, Switzerland) provides rotational and angular stability by obtaining a large surface area with a single helical lag screw in the femoral neck (4). The InterTan nail (Smith & Nephew, Memphis, TN, USA) reduces stress on the lateral cortex with screw medialisation providing linear compression with 2 integrated lag screws
(20). In a biomechanical study it was shown that the InterTan nail had some biomechanical advantages over the PFNA in intertrochanteric fractures (9). In a recent, the conclusion was reached that the InterTan nail was better than PFNA in the treatment of 31-A2 and 31-A3 intertrochanteric fractures (30).
However, to the best of our knowledge, there has not been any study in literature which has compared the clinical and radiological results of PFNA and InterTan nailing in the treatment of only 31-A3 intertrochanteric fractures.
The aim of this study was to compare the clinical and radiological results of PFNA and InterTan nailing in the treatment of reverse intertrochanteric fractures where the lateral cortex was fractured.
PATIENTS AND METHODS
The data of all patients with a 31-A3 inter-trochanteric fracture who presented at the Emergency Department of our hospital between March 2008 and April 2015 were retrospectively evaluated for inclusion in the study. Patients with pathological fractures, died in the early postoperative period and those treated with implants other than InterTan/ PFNA were excluded from the study. Thus, a total of 69 patients with a minimum of 1 year follow-up were included in the study.
Choice of implant
All of the operations were performed in the same department by participation of one of two surgeons who were experienced in trauma surgery (A.I. and C.Y.K.). Both PFNA and InterTan nail were available concurrently and given that there was no clear evidence to support the use of one system
over the other, the choice of implant was randomly made. PFNA device was used on 33 patients and InterTan nailing was used on 36 patients.
Surgical Technique and Follow-up protocol Antibiotic prophylaxis (cefalozin sodium 1 gr/day IV) were administered to all patients half an hour before the skin incision was made. The operations in both groups were made under spinal or general anaesthesia. The patients were operated on in the lateral decubitus position under C-arm fluoroscopy. A fracture table was not used. The intervention was applied with closed reduction of the fracture. An open surgery approach was only used on patients where suitable reduction could not be obtained with closed maneuvers. In the postoperative period, low molecular weight heparin (enoxaparin sodium 40 mg/0.4 mL/day) was administered together with standard medical care. With the assistance of a physiotherapist in the postoperative period, depending on the patient’s tolerance, the stability of the biomechanical structure and the quality of the bone, the patient was encouraged to attempt partial weight-bearing as much as possible and the day that weight could be given was recorded. The patients were followed up at regular intervals for clinical and radiological evaluation of time to union and for physiotherapy. The Harris Hip Scores were recorded at 1 year.
Clinical and radiological assessment
The age, gender and preoperative ASA scores of the patients were recorded (Table I). On postoperative day 1, plain anteroposterior (AP) and lateral radographs were taken. The quality of reduction on these radiographs was graded as good, acceptable (5°-10° varus or valgus and /or anteversion or retroversion) or poor (>10° varus or valgus and /or anteversion or retroversion) (26)
(Table II). According to the Cleveland-Bosworth Quadrants, center-center and inferior-center quadrants were accepted as optimal and the remaining quadrants were accepted as suboptimal (5).
Fracture union was defined as osseous bridging seen in at least 3 cortices on the AP and lateral
Characteristics PFNA (n=33) InterTan (n=36) P value Age (years) 54.64±18.94 57.86±22.00 0.259 Female/Male 14/19 13/23 0.477 Laterality: Right/Left 18/15 16/20 0.161 AO/OTA classification 31-A3.1 31-A3.2 31-A3.3 10 5 18 8 9 19 0.531 ASA score 3 or 4 1 or 2 12 21 16 20 0.661 Table I. — The demographic characteristics of the patients treated with PFNA and InterTan
PFNA (n=33) InterTan (n=36) P value
Harris hip score 79.82±10.18 82.56±11.33 0.294
Union time (weeks) 17.76±4.82 17.11±4.65 0.573
Partial weight-bearing (days) 6.73±4.01 5.47±2.91 0.145 Quality of reduction Good Acceptable Poor 22 8 3 27 6 3 0.791 Implant position Optimal Suboptimal 27 6 26 10 0.510 Neck shaft angle change (degrees) 5.32±6.02 3.72±3.5 0.187
Teleskoping, mm 7.21±7.13 4.18±4.32 0.039
Complication (cases) Shaft fracture
Cut-out Cut-through
Severe lateral migration screw Nonunion 1 4 1 2 1 0 0 0 0 1 0.0001
Table II. — Comparison of the radiological and functional values, the time to union, time to mobilisation and reduction quality
radiographs and pain-free full weight-bearing (17). Functional results were evaluated with the Harris Hip Score. A record was made of mechanical complications which could develop in follow-up, such as varus collapse, hip screw or blade migration, cut-out, cut-through, shaft fracture and non-union.
On the postoperative day 1 and final follow-up radiographs, the neck shaft angle and telescoping were measured using the picture archiving and
communication system (PACS). Telescoping, was defined as the distance along the blade from the lateral border of the nail to the blade end. The difference in telescoping is considered as the amount of sliding of the proximal fragment (27). Measurements were standardized and significant measurements were evaluated by 2 experienced orthopaedic surgeons. To prevent any prejudice in the radiological evaluations, they were completed before the evaluations of the functional results.
group and 4.18±4.32 mm in the InterTan group and the difference was not statistically significant (p = 0.039) (Table II).
A statistically significantly lower rate of complications was determined in the patients treated with InterTan (2.8%) compared to the patients treated with PFNA (27.3%) (one-sided proportion test, p < 0.0001). Revision surgery was required with a long nail in 1 patient of each group due to femoral shaft fracture. Second surgery was performed to 8 (24.2%) patients in the PFNA group because of mechanical failure and to one in the InterTan group. As blade cut-out occurred in 4 patients of the PFNA group, arthroplasty was applied. In 1 patient, erosion developed in the acetabulum because of blade protrusion and total hip arthroplasty was applied. There was a need for revision surgery in 1 patient because of symptomatic non-union and in 2 patients because of severe blade lateral migration. One case of non-union were observed in the InterTan group (Fig. 3).
DISCUSSION
Reverse intertrochanteric fractures have unique anatomic and biomechanical characteristics
(7,14,15). In these types of injuries where there is
a fracture of the lateral femoral wall, because of high rates of implant failure which develop with sliding hip screw plate systems, the application of intramedullar nailing is currently recommended
(21). Due to the complications of second generation
intramedullar fixation devices, including femoral shaft fracture, Z effect, fixation failure and distal locking complications, which require re-operation, third generation intramedullar nail designs have been developed (1,2, 8,20,23).
In studies by Zhang et al. (30), Yu et al. (28) and
Seyhan et al. (22) comparing PFNA and InterTan in the treatment of unstable intertrochanteric fractures, the Harris Hip Scores of both groups were found to be similar. In the currrent study, the Harris Hip Scores were obtained similar in both groups. In a previous report, varus collapse was reported to be significantly greater in the PFNA group (11.1%) and in another report, no difference was reported in the change in the neck shaft angle [20,21]. In the To eliminate differences in measurements arising
from the position of the extremity or radiological magnifications, corrections were made in the ratio of the variables of known screw length and measured screw length (12).
Statistical analysis
Differences in harris hip scores, telescopings, neck shaft angle changes, union times and partial weight-bearings between the nail types were assessed by using two-sample t-tests. In the tables, we use Mean±Standard Deviation notation to summaries the data. To evaluate the associations between nail types and quality of reduction, AO classification, ASA scores and implant positions in the studied patient cohorts, Chi-square tests, were used. All statistical testing was performed with software R(www.r-project.org) (19).
RESULTS
The mean age of the patients was 54.64 ± 18.94 years in the PFNA group and 57.86 ± 22.00 years in the InterTan group (p = 0.259). No statistically significant difference was determined between the groups in respect of gender, AO/OTA classification and ASA scores (p = 0.477, p = 0.531 and p = 0.661, respectively). The demographic characteristics of the patients treated with PFNA and InterTan are shown in Table I.
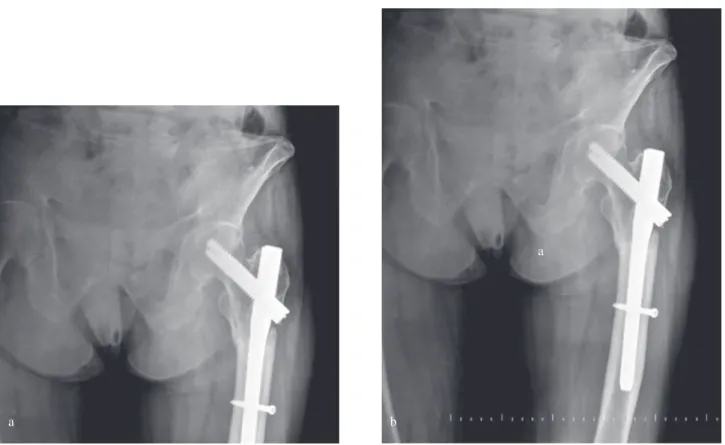
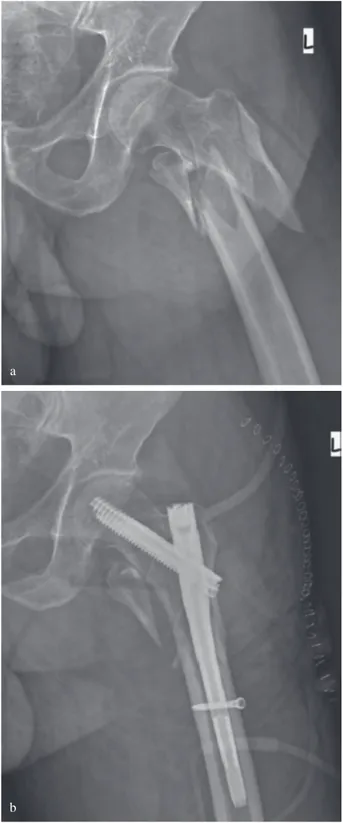
In the 33 patients in the PFNA group, closed reduction was applied to 19 (57.6%) patients and open surgery to 14 (42.4%) (Fig. 1). In the 36 patients in the InterTan group, closed reduction was applied to 18 (50%) patients and open surgery to 18 (50%) (Fig.2). No infection developed in any patient.
No statistically significant difference was determined between the groups in respect of Harris Hip Scores, changes in neck shaft angle, time to union and time to partial weight-bearing (p = 0.294, 0.187, 0.461, 0.573 and 0.145, respectively). There was no association between the nail types and quality of reduction and implant position (p = 0.793 and 0.510, respectively). Mean telescoping was determined as mean 7.21±7.13mm in the PFNA
Fig. 1. — (a) AP Radiographs pre-operative (b) post-operative and (c) lateral radiographs, after PFNA fixation of an reverse
intertrochanteric fracture (AO/OTA 31-A3.1 type)
our study, no significant difference was determined between the groups in respect of change in the angle between neck and shaft which demonstrates varus collapse (p = 0.187, two-sample t-test). However, to the best of our knowledge, there has been no study in literature comparing PFNA device and InterTan nail in only reverse intertrochanteric fractures where the effective forces are completely different. The type of nail was not seen to affect the time to union or partial weight-bearing.
Significantly greater shortening in the femoral neck was reported by Zhang et al. (30) in the
InterTan group and by Yu et al. (28) and Seyhan et al. (22) in the PFNA group. In the current study, the
amount of telescoping which shows shortening of the femoral neck was seen to be statistically greater in the PFNA group (t-tests, p = 0.039).
In a biomechanical study, it was reported that InterTan nail was biomechanically superior to the PFNA device and mechanical failure was
a
screw (5,11,25). In the study findings there was no significant difference between these factors which could change the complication rate between the two groups. As these complications were seen mostly in the cases at the beginning of the series, they can be associated with the learning curve.
The revision rate of 24.2% in the PFNA group because of mechanical failure was found to be higher than that of cephalomedullar implants used in literature (10,23,26). In a similar study, Makki et al. (13) used PFNA in 36 reverse oblique intertrochanteric fractures and while implant failure was observed in 8 (22.2%) cases, no failure was observed in any case where trochanteric antegrade nails were used. In another study where InterTan nails were used in 100 displaced intertrochanteric fractures, no reduction loss, uncontrolled neck collapse, non-union, varus malunion, femoral shaft fracture or implant failure was seen in any case (20). Superior implant protrusion developed in 2 cases caused by poor initial implant placement early in observed less (9). In clinical studies of unstable
intertrochanteric fractures, while blade cut-out was observed in 6 (6.9%) cases reported by Yu et al.
(28), in 2 (4.3%) cases by Zhang et al. (30) and in 8 (9.4%) cases by Zehir et al. (29), no postoperative cut-out was observed in any cases in the InterTan groups. In a series reported by Turgut et al. (25), cut-out was observed in 14 (4.7%) patients. Takigami et al. (24) reported cut-out at 4% suggesting that this could have resulted from an inadequate insertion depth of the spiral blade and early full weight-bearing. Frei et al. (6) also showed that cut-out of blades may occur with weight-bearing after PFNA device placement. In the PFNA group of the current study, cut-out was seen in 4 (12.1%) cases as the most frequent mechanical failure, and it was not observed at all in the InterTan group. The most important factors to prevent cut-out complications have been reported to be the avoidance of varus reduction and centre-centre or inferior-centre quadrant implantation of the helical blade or lag
Fig. 2. — (a) AP Radiographs pre-operative and (b) 1 year post-operative, after InterTan fixation of an reverse intertrochanteric
fracture (AO/OTA 31-A3.3 type)
a b
When the fracture gap is not well closed and the patient starts weight-bearing, uncontrolled collapse may occur following shortening of the femur and
Fig. 3. — (a) AP Radiograph of the left hip showing a AO/
OTA 31-A3.3 fracture (b) post-operative 1. day and (c) At eleven months, a case of mechanical insufficient due to the non-union of an InterTan fixation
the series (20). The high rate in the current study can be attributed to the inclusion of reverse trochanteric fractures only.
a
b
migration of the hip screw. It has been reported that there may be unacceptable shortening in the head and neck segment or neck malunion as a result of collapse (4,22). Seyhan et al. (22) reported
that InterTan provided more effective compression during surgery and allowed the fracture gap to be closed in an effective way. Thus, screw backup which results in femoral shortening is observed less often. Previous studies have reported severe lateral hip screw migration during follow-up at rates of 5.8% and 8.9% in the PFNA group and in no cases of the InterTan group (28,29). In the our study, the
amount of telescoping which shows the amount of lateral migration of the lag screw was greater in the PFNA group. In the PFNA group, revision with arthroplasty was applied to 2 patients because of excessive lateral blade migration and to 1 patient because of cut-through.
The complication of fracture of the femoral shaft at the tip of the nail is known to be associated with the use of intramedullary nail in the treatment of proximal femoral fractures (3,18). In the PFNA
group of the current study, femoral shaft fracture was seen in 1 (3%) case and in the InterTan group in zero case, whereas Yu et al. (28) reported 8 (11.1%) PFNA group cases and 1 (1.3%) InterTan group case.
Limitations of the current study were that it was a retrospective and its susceptibility to associated risks of bias. However, the two groups were well matched and this allowed us to conclude that the differences observed between the two implants were not related to patients’ demographics or the severity of fracture. Fracture reduction was performed without a fracture table in all cases, thus the risk of varus reduction could have been influenced negatively.
CONCLUSİON
The findings of this study showed that as there is greater lateral migration in PFNA, there is a greater tendency for mechanical failure. As InterTan has a low complication rate, it can be considered more advantageous in patients with reverse intertrochanteric fractures and can be an optimal treatment choice.
Conflicts of Interest: No conflicts declared.. REFERENCES
1. Al-yassari G, Langstaff RJ, Jones JW, Al- Lami M. The AO/ASIF proximal femoral nail (PFN) for the treatment of unstable trochanteric femoral fracture. Injury. 2002;33:395-399.
2. Banan H, Al-Sabti A, Jimulia T, Hart AJ. The treatment of unstable, extracapsular hip fractures with the AO/ASIF proximal femoral nail (PFN)—our first 60 cases. Injury. 2002;33:401-405.
3. Brammar TJ, Kendrew J, Khan RJ, Parker MJ. Reverse obliquity and transverse fractures of the trochanteric region of the femur; a review of 101 cases. Injury. 2005;36:851-7. 4. Brunner A, Büttler M, Lehmann U, Frei HC, Kratter R, Di Lazzaro M, et al. What is the optimal salvage procedure for cut-out after surgical fixation of trochanteric fractures with the PFNA or TFN?: A multicentre study. Injury. 2016;47:432-8.
5. Cleveland M, Bosworth DM, Thompson FR, Wılson HJ Jr, Ishızuka T. A ten-year analysis of intertrochanteric fractures of the femur. J Bone Joint Surg Am. 1959;41-A:1399-408.
6. Frei HC, Hotz T, Cadosch D, Rudin M, Käch K. Central head perforation, or “cut through,” caused by the helical blade of the proximal femoral nail antirotation. J Orthop Trauma. 2012;26:e102–7.
7. Haidukewych GJ. Intertrochanteric fractures: ten tips to improve results. J Bone Joint Surg Am. 2009;91:712-9. 8. Honkonen SE, Vihtonen K, Jarvinen MJ. Second
generation cephalo medullary nails in the treatment of reverse obliquity intertrochanteric fractures of the proximal femur. Injury. 2004;35:179–183.
9. Huang Y, Zhang C, Luo Y. A comparative biomechanical study of proximal femoral nail (InterTAN) and proximal femoral nail antirotation for intertrochanteric fractures. Int Orthop. 2013;37:2465-73.
10. Irgit K, Richard RD, Beebe MJ, Bowen TR, Kubiak E, Horwitz DS. Reverse Oblique and Transverse Intertrochanteric Femoral Fractures Treated With the Long Cephalomedullary Nail. J Orthop Trauma. 2015;29:e299-304. 11. Kashigar A, Vincent A, Gunton MJ, Backstein D, Safir
O, Kuzyk PR. Predictors of failure for cephalomedullary nailing of proximal femoral fractures. Bone Joint J. 2014;96-B:1029-34.
12. Kim Y, Bahk WJ, Yoon YC, Cho JW, Shon WY, Oh CW, et al. Radiologic healing of lateral femoral wall fragments after intramedullary nail fixation for A3.3 intertrochanteric fractures. Arch Orthop Trauma Surg. 2015;135:1349-56. 13. Makki D, Matar HE, Jacob N, Lipscombe S, Gudena R.
Comparison of the reconstruction trochanteric antigrade nail (TAN) with the proximal femoral nail antirotation (PFNA) in the management of reverse oblique intertrochanteric hip
fractures. Injury. 2015;46:2389-93.
14. Matre K, Havelin LI, Gjertsen JE, Vinje T, Espehaug B, Fevang JM.Sliding hip screw versus IM nail in reverse oblique trochanteric and subtrochanteric fractures. A study of 2716 patients in the Norwegian Hip Fracture Register. Injury. 2013;44:735-42.
15. Min WK, Kim SY, Kim TK, Lee KB, Cho MR, Ha YC, et al. Proximal femoral nail for the treatment of reverse obliquity intertrochanteric fractures compared with gamma nail. J Trauma. 2007;63:1054-60.
16. Ozkan K, Eceviz E, Unay K, Tasyikan L, Akman B, Eren A. Treatment of reverse oblique trochanteric femoral fractures with proximal femoral nail. Int Orthop. 2011;35:595-8.
17. Park SY, Yang KH, Yoo JH, Yoon HK, Park HW. The treatment of reverse obliquity intertrochanteric fractures with the intramedullary hip nail. J Trauma. 2008;65:852-7. 18. Paul O, Barker JU, Lane JM, Helfet DL, Lorich DG.
Functional and radiographic outcomes of intertrochanteric hip fractures treated with calcar reduction, compression, and trochanteric entry nailing. J Orthop Trauma. 2012;26:148-54.
19. R Core Team. R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. 2016. ISBN 3-900051-07-0, URL http:// www.R-project.org/.
20. Ruecker AH, Rupprecht M, Gruber M, Gebauer M, Barvencik F, Briem D, et al. The treatment of intertrochanteric fractures: results using an intramedullary nail with integrated cephalocervical screws and linear compression. J Orthop Trauma. 2009;23:22-30.
21. Sadowski C, Lubbeke A, Saudan M, Riand N, Stern R, Hoffmeyer P. Treatment of reverse oblique and transverse interthrochanteric fractures with use of an intramedullary nail or a 958 screw-plate: a prospective, randomized study. J Bone Joint Surg 2002;84:372–81.
22. Seyhan M, Turkmen I, Unay K, Ozkut AT. Do PFNA devices and Intertan nails both have the same effects in the treatment of trochanteric fractures? A prospective clinical study. J Orthop Sci. 2015;20:1053-61.
23. Simmermacher RK, Ljungqvist J, Bail H, Hockertz T, Vochteloo AJ, et al. The new proximal femoral nail antirotation (PFNA) in daily practice: results of a multicentre clinical study. Injury. 2008;39:932-9.
24. Takigami I, Matsumoto K, Ohara A, Yamanaka K, Naganawa T, Ohashi M, et al. Treatment of trochanteric fractures with the PFNA (proximal femoral nail antirotation) nail system - report of early results. Bull NYU Hosp Jt Dis. 2008;66:276-9.
25. Turgut A, Kalenderer Ö, Karapınar L, Kumbaracı M, Akkan HA, Ağuş H. Which factor is most important for occurrence of cutout complications in patients treated with proximal femoral nail antirotation? Retrospective analysis of 298 patients. Arch Orthop Trauma Surg. 2016;136:623-30. 26. Vidyadhara S, Rao SK. One and two femoral neck screws
with intramedullary nails for unstable trochanteric fractures of femur in the elderly--randomised clinical trial. Injury. 2007;38:806-14.
27. Yoo JH, Kim TY, Chang JD, Kwak YH, Kwon YS. Factors influencing functional outcomes in united intertrochanteric hip fractures: a negative effect of lag screw sliding. Orthopedics. 2014;37:e1101-7.
28. Yu W, Zhang X, Zhu X, Hu J, Liu Y. A retrospective analysis of the InterTan nail and proximal femoral nail anti-rotation-Asia in the treatment of unstable intertrochanteric femur fractures in the elderly. J Orthop Surg Res. 2016;11:10.
29. Zehir S, Şahin E, Zehir R. Comparison of clinical outcomes with three different intramedullary nailing devices in the treatment of unstable trochanteric fractures. Ulus Travma Acil Cerrahi Derg. 2015;21:469-76.
30. Zhang S, Zhang K, Jia Y, Yu B, Feng W. InterTan nail versus Proximal Femoral Nail Antirotation-Asia in the treatment of unstable trochanteric fractures. Orthopedics. 2013;36:e288-94.