Full Terms & Conditions of access and use can be found at
https://www.tandfonline.com/action/journalInformation?journalCode=nbrr20
Biological Rhythm Research
ISSN: 0929-1016 (Print) 1744-4179 (Online) Journal homepage: https://www.tandfonline.com/loi/nbrr20
The effect of individual biological rhythms on dry
eye
Halil İbrahim Yener, Yavuz Selvi & Rukiye Tekdemir
To cite this article: Halil İbrahim Yener, Yavuz Selvi & Rukiye Tekdemir (2019) The effect of individual biological rhythms on dry eye, Biological Rhythm Research, 50:5, 659-664, DOI: 10.1080/09291016.2018.1478683
To link to this article: https://doi.org/10.1080/09291016.2018.1478683
Published online: 25 May 2018.
Submit your article to this journal
Article views: 66
View related articles
View Crossmark data
https://doi.org/10.1080/09291016.2018.1478683
The effect of individual biological rhythms on dry eye
Halil İbrahim Yenera, Yavuz Selvib and Rukiye TekdemirbaDepartment of ophthalmology, Konya eye center, Konya, turkey; bDepartment of Psychiatry, Faculty of medicine, selcuk University, sam Neuroscience Research center, Konya, turkey
ABSTRACT
This study aims to assess whether an individual’s chronotype (i.e. morningness versus eveningness) has an impact on tear film. Eighty-six dry eye patients not having any underlying systemic or metabolic diseases and either a morning or evening chronotype were included in the study. Tear film break-up time (BUT) and Schirmer tests are common objective tests that are used to diagnose the eye dryness. Using multivariate analysis of covariance (MANCOVA), we investigated the interaction effect of chronotype x sex on insomnia, Schirmer (mm) and BUT (sec) measurements after adjusting for age. We found that the participants who were more prone to evening chronotype characteristics reported to have more severe dry eye signs which monitor with the aid of the Schirmer and tear film break-up time test. In addition, those with higher scores in insomnia severity index had lower Schirmer test and tear film break-up time scores. These findings suggest that chronobiological factors may play a crucial role in the dry eye symptom severity.
Introduction
The tear film is composed of lipid, aqueous, and mucin layers. The lipid layer protects the aqueous layer of tear film from evaporation as the mucin layer adheres the tear film to the surface epithelium. The aqueous layer secreted by lacrimal glands is the most important layer for ocular surface health (Lemb MA 2007). Dry eye is a multifactorial disease of the ocular surface characterized by a loss of homeostasis of the tear film and accompanied by ocular symptoms such as eye discomfort, grittiness, and visual disturbance. Dry eye disrupts homeostasis at the ocular surface, resulting in surface damage, epithelial cell apoptosis, loss of goblet cells, and squamous metaplasia. The changes and inflammation of the ocular surface subsequently produce tear instability, which causes an increase in the tear osmolality and provokes the inflammatory cascades (Johnson and Murphy 2004). Tear film secretion is regulated by an integrated array of neural and hormonal processes. Direct innervation of the lacrimal and meibomian glands and goblet cells has been demonstrated, with m3 class cholinergic receptors predominating in the lacrimal gland. Androgens appear to have a positive effect on the tear secretion. Dry eye symptoms have been associated with multiple causes, including depressive disorders, drug uses, hormonal status, and systemic diseases.
© 2018 informa UK limited, trading as taylor & Francis group
KEYWORDS
Dry eye; chronotype; biological rhythm
ARTICLE HISTORY
Received 16 april 2018 accepted 20 april 2018
660 H. İ. YENER ET AL.
Environmental conditions such as high altitude, dryness, extreme heat, and severe light (Savini et al. 2008; Kamperis et al. 2010).
Timing of daily activities is associated with markers of circadian time and show inter-in-dividual differences. Biological rhythm researches indicate that some of many biological events – i.e. body temperature, hormonal changes (growth hormone, melatonin, cortisol, etc.), social programs (meal time, appetite, task performance), and mood – have been adjusted by individual sleep–wake cycle (Bailey and Heitkemper 1991; Baehr et al. 2000; Griefahn 2002; Selvi et al. 2011).
Chronotypes are individual biological and behavioral rhythm characteristics that show preference as to a sleep–wake cycle. It is well established in many studies that morning types showed a marked preference for waking at an early hour and went to bed early, while evening types woke up late and stay out late and exposure to artificial bright light (Gau et al. 2007; Selvi et al. 2007; Jankowski and Ciarkowska 2008).
This study aims to assess whether an individual’s chronotype (i.e. morningness versus eveningness) has an impact on tear film.
Method
Morningness–eveningness questionnaire was conducted for patients diagnosed with dry eye. Schirmer test and break-up time (BUT) were performed when diagnosing with dry eye. Those whose Schirmer tests were found below 10 mm and BUT below 10 s were regarded as the dry eye. A complete ophthalmic examination was carried out for the patients enrolled in the study. Those with any eye disease affecting ocular surface, those undergoing any eye surgery, those using eye drops for glaucoma, and those using systemic drugs which may cause dry eye were excluded from the study.
Participants
This study was conducted over a span of two months between March and April 2016 at Konya Eye Center, Turkey. Patients were informed about the aims of the study and their written approvals were obtained. The study protocol was approved by the Selcuk University Ethics Committee. Morning and evening types were evaluated, and intermediate types were excluded from the study to assess the effects of the most divergent chronotypes on the tear film.
We restricted our study to morning and evening types in order to determine whether differences in the severity of dry eye could be detected in the most divergent chronotypes. The routine physical examination and laboratory tests include biochemistry, blood count, and serological tests. They were not compensated for their participation in any way. Finally, 86 cases of eye dryness not having any underlying systemic or metabolic diseases and were either a morning or evening chronotype were included in the study. Of the sample, 37 patients were men (43%). Age of the participants ranged from 18 to 49 and their mean age was 38.7 years (SD ± 8.2), with 38.6 ± 7.9 for males and 39.2 ± 9.1 for females.
The morningness–eveningness questionnaire (MEQ) of Horne and Östberg was used to determine the chronotypes (Horne and Östberg 1976). The MEQ is a 19-item questionnaire that assesses habitual rising and bed times, preferred times of physical and mental perfor-mance, and subjective alertness after rising and before going to bed. The range of scoring
is from 16 to 86; the participants scoring between 59 and 86 are considered as morning types; those scoring 42–58 as neither types; and those scoring 16–41 as evening types. Agargun et al. translated the questionnaire into Turkish and tested the Turkish version for its psychometric properties (Agargun et al. 2007).
Insomnia Severity Index (ISI) is a reliable and valid instrument that quantifies perceived insomnia severity. The scale consists of 7 items measuring severity of difficulties with sleep onset, sleep maintenance, early morning awakenings, sleep problem interference with daily functioning, indications to others of impairment due to sleep problems, degree of concern about current sleep problem, and satisfaction/dissatisfaction with current sleep pattern (Bastien et al. 2001). Each item is rated on a 0–4 scale and the total score ranges from 0 to 28. The higher score is, the more severe the insomnia. The ISI takes less than 5 min to com-plete and can be scored in less than 1 min. Turkish validity and reliability study was conducted by Boysan et al. (Boysan 2014).
Tear film break-up time is a common objective test that is used to diagnose dry eye. Tears are stained with fluorescein dye and the time interval is measured between a complete blink to the first appearance of a dry spot in the pre-corneal tear film. Values less than ten seconds indicate the disruption of tear film stability.
For Schirmer test, the Schirmer tear strip is placed on one-third outer side of the eye. After 5 min-waiting time, the amount of wetting of the paper is read from the millimetric lines on the graph paper. Values less than 10 mm is considered abnormal.
Statistical analysis
Descriptive statistics were calculated for the sample. One-way analysis of variance model was utilized to assess the effect of the morning and evening chronotypes on their mean dry eye severity and insomnia severity scores. SPSS (Windows, version 16.0, SPSS Inc., Chicago, IL) was used to analyze the data. A p-value of 0.05 is considered on the borderline of statistical significance.
Participants
A total of 86 patients ranged their age from 18 to 49 were included in the study. The mean age was 30.06 (SD ± 7.48) and 57.65% of the sample were comprised of females (n = 49). Using one-way analysis of variance, we found that participants allocated to the evening-type group were older than morning-type individuals (F(1, 83)=9.565 p < 0.01 η2=0.103). Gender
proportions did not significantly vary according to morningness and eveningness groups (χ2 (1)=0.426 p = 0.514).
Results
Using multivariate analysis of covariance (MANCOVA), we investigated the interaction effect of chronotype x sex on insomnia, Schirmer (mm), and BUT (sec) measurements after adjusting for age. We found that the interaction effect of chronotype x sex and main effect of sex were not significant (p > 0.05). Contrarily, multivariate difference between morning type and evening type was significant after controlling for chronotype x sex interaction effect, main effect of sex and age as a covariate (Wilk’s λ =,727; F(3, 78)= 9.760 p < 0.001 η2 = 0.273).
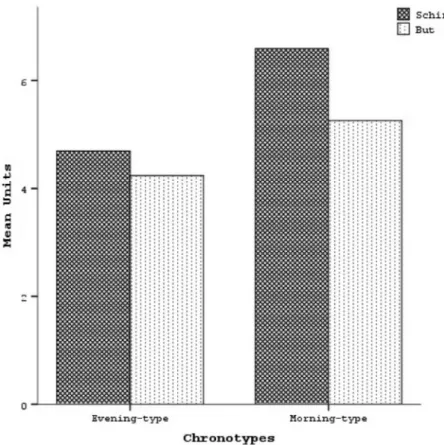
Schirmer (unit/mm) (F(1,80)= 24.468 p < 0.001 η2 = 0.234) and But (unit/sec) (F(1,80)= 4.343 p < 0.05 η2 = 0.051) (Table 1) measurements were significantly low among evening-type
patients with eye dryness problem compared to morning-type patients (see Figure 1).
Discussion
We found that the participants who were more prone to evening chronotype characteristics reported to have more severe dry eye signs monitored with the aid of the Schirmer and tear film break-up time test. In addition, those with higher scores in insomnia severity index had lower Schirmer and BUT scores. These findings suggest that chronobiological factors may play a crucial role in the dry eye symptom severity.
Dry eye is among the most common complaints in the patients referred to an ophthal-mologist. It is an important condition that impairs quality of life. It leads to both eye dryness and problems with visual activities due to the symptoms caused by itself (Apostol et al. 2003; Gayton 2009).
Many environmental factors play a role in the formation of dry eye, as well as risk factors such as gender and advanced age. These environmental factors include lack of moisture, environment dryness, high temperature, air conditioning, smoking, bright light, and occu-pational factors, long-term watching on the screen and nutrition problems.
We aimed to investigate the effect of features of biological rhythm on dry eye. Morning chronotypes, also known as “larks,” go to bed early and wake up early. The evening chrono-types, also known as “owls,” go to bed late and wake up late (Kudielka et al. 2006; Gau et al.
2007; Selvi et al. 2007; Muro et al. 2009; Nielsen 2010; Selvi et al. 2011; Jankowski and Ciarkowska 2008). This causes the evening-type individuals to be much exposed to bright light than morning types. Evening chronotypes also have irregular life styles in uniformity of daily activities, such as eating, exercise, and social rhythms compared to the morning types (Monk et al. 2004).
Table 1. multivariate analysis of covariance (maNcoVa) of the dependent variables according to inter-action between chronotypes and sex.
Note. significant statistics are boldfaced. insomnia severity index adjusted R2 = 0.011; schirmer (mm) adjusted R2 = 0.361;
But (sec) adjusted R2 = 0.136.
Dependent Mean square F df P Partial η2
chronotype x sex Wilk’s λ = 0.972 0.737 3, 78 0.533 0.028 insomnia severity index 4.649 0.245 1, 80 0.622 0.003 schirmer (mm) 2.057 1.141 1, 80 0.289 0.014
But (sec) 4.638 2.111 1, 80 0.150 0.026
chronotype Wilk’s λ = 0.727 9.760 3, 78 <0.001 0.273
insomnia severity index 0.297 0.016 1, 80 0.901 0.000 schirmer (mm) 44.092 24.468 1, 80 <0.001 0.234
But (sec) 9.539 4.343 1, 80 0.040 0.051
sex Wilk’s λ = 0.909 2.590 3, 78 0.059 0.091
insomnia severity index 14.800 0.779 1, 80 0.380 0.010 schirmer (mm) 0.007 0.004 1, 80 0.951 0.000
But (sec) 7.655 3.485 1, 80 0.066 0.042
Covariates
age Wilk’s λ = 0.894 3.096 3, 78 0.032 0.106
insomnia severity index 68.230 3.593 1, 80 0.062 0.043 schirmer (mm) 14.616 8.111 1, 80 0.006 0.092
But (sec) 5.611 2.554 1, 80 0.114 0.031
Recent increasing technological advances and social conditions have caused people to much use the technological devices than ever before. Shift work and spending time in high-lighted places until late hours are becoming common. These conditions bring about the changes in biological rhythms. Moreover, spending more time in especially bright-illumi-nated and dry air heated and cooled spaces leads to an increase in the complaints about eye dryness. Impaired sleep pattern and using screened device disrupt tear film stability, resulting in the dry eye condition (Moss et al. 2008; Catalan et al. 2009). This information suggests that lifestyle and individual biological rhythm may have an impact on dry eye.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
Agargun MY, Cilli AS, Boysan M, Selvi Y. 2007. Turkish version of morningness-eveningness questionnaire (MEQ). Sleep and Hypnosis. 9(1):16.
Apostol S, Filip M, Dragne C, Filip A. 2003. Dry eye syndrome. Etiological and therapeutic aspects. Oftalmologia (Bucharest, Romania: 1990). 59(4):28–31.
Baehr EK, Revelle W, Eastman CI. 2000. Individual differences in the phase and amplitude of the human circadian temperature rhythm: with an emphasis on morningness–eveningness. J Sleep Res. 9(2):117–127.
Bailey SL, Heitkemper MM. 1991. Morningness-eveningness and early-morning salivary cortisol levels. Biol Psychol. 32(2–3):181–192.
Bastien CH, Vallières A, Morin CM. 2001. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. 2(4):297–307.
Boysan M. 2014. Dissociative experiences are associated with obsessive-compulsive symptoms in a non-clinical sample: a latent profile analysis. Nöro Psikiyatri Arşivi. 51(3):253.
Catalan RG, Olivera EJ, Munoz-Hernandez A, Benitez-del-Castillo J-M. 2009. Dry eye and quality of life. Invest Ophthalmol Vis Sci. 50(13):4672–4672.
Lemb MA. 2007. The definition and classification of dry eye disease: report of the defination and classification subcommittee of the international dry eye workshop. Ocul Surf. 5(2):75–94.
Gau SS-F, Shang C-Y, Merikangas KR, Chiu Y-N, Soong W-T, Cheng AT-A. 2007. Association between morningness-eveningness and behavioral/emotional problems among adolescents. J Biol Rhythms. 22(3):268–274.
Gayton JL. 2009. Etiology, prevalence, and treatment of dry eye disease. Clin Ophthalmol. 3:405–412. Griefahn B. 2002. The validity of the temporal parameters of the daily rhythm of melatonin levels as
an indicator of morningness. Chronobiol Int. 19(3):561–577.
Horne JA, Östberg O. 1976. A self-assessment questionnaire to determine morningness-eveningness in human circadian rhythms. Int J Chronobiol. 4:97–110.
Jankowski KS, Ciarkowska W. 2008. Diurnal variation in energetic arousal, tense arousal, and hedonic tone in extreme morning and evening types. Chronobiol Int. 25(4):577–595.
Johnson ME, Murphy PJ. 2004. Changes in the tear film and ocular surface from dry eye syndrome. Prog Retin Eye Res. 23(4):449–474.
Kamperis K, Hagstroem S, Radvanska E, Rittig S, Djurhuus JC. 2010. Excess diuresis and natriuresis during acute sleep deprivation in healthy adults. Am J Physiol Renal Physiol. 299(2):F404–F411. Kudielka BM, Federenko IS, Hellhammer DH, Wüst S. 2006. Morningness and eveningness: The free
cortisol rise after awakening in “early birds” and “night owls”. Biol Psychol. 72(2):141–146.
Monk TH, Buysse DJ, Potts JM, DeGrazia JM, Kupfer DJ. 2004. Morningness-eveningness and lifestyle regularity. Chronobiol Int. 21(3):435–443.
Moss SE, Klein R, Klein BE. 2008. Long-term incidence of dry eye in an older population. Optom Vis Sci. 85(8):668–674.
Muro A, Gomà-i-Freixanet M, Adan A. 2009. Morningness-eveningness, sex, and the alternative five factor model of personality. Chronobiol Int. 26(6):1235–1248.
Nielsen T. 2010. Nightmares associated with the eveningness chronotype. J Biol Rhythms. 25(1):53–62. Savini G, Prabhawasat P, Kojima T, Grueterich M, Espana E, Goto E. 2008. The challenge of dry eye
diagnosis. Clin Ophthalmol. 2(1):31. Auckland, NZ.
Selvi Y, Gulec M, Agargun MY, Besiroglu L. 2007. Mood changes after sleep deprivation in morningness– eveningness chronotypes in healthy individuals. J Sleep Res. 16(3):241–244.
Selvi Y, Aydin A, Atli A, Boysan M, Selvi F, Besiroglu L. 2011. Chronotype differences in suicidal behavior and impulsivity among suicide attempters. Chronobiol Int. 28(2):170–175.