A new criterion to differentiate atrioventricular nodal reentrant
tachycardia from atrioventricular reciprocating tachycardia: Combined
AVR criterion
Abdullah Orhan Demirta
ş, MD
a, Yahya Kemal Icen, MD
a, Onur Kaypakl
ı, MD
b, Hasan Koca, MD
a,
İlker Ünal, PhD
c, Zikret Köseo
ğlu, MD
d, Durmus Y
ıldıray Sahin, MD
a, Mevlut Koc, MD
a,⁎
a
Department of Cardiology, University of Health Sciences - Adana Health Practice and Research Center, Adana, Turkey
bDepartment of Cardiology, Mustafa Kemal University– Faculty of Medicine, Hatay, Turkey c
Department of Biostatistics, Cukurova University– Faculty of Medicine, Adana, Turkey
dEmergency Medicine, Department of Emergency Medicine, University of Health Sciences - Adana Health Practice and Research Center, Adana, Turkey
a b s t r a c t
a r t i c l e i n f o
Aim: A combined aVR criterion is described as the presence of a pseudo r′ wave in aVR during tachycardia in pa-tients without r′ wave in aVR in sinus rhythm and/or a ≥50% increase in r′ wave amplitude compared to sinus rhythm in patients with r′ wave in the basal aVR lead. We aimed to investigate the use of combined aVR criterion in differential diagnosis of atrioventricular nodal reentrant tachycardia (AVNRT) and atrioventricular reciprocat-ing tachycardia (AVRT).
Methods: In this prospective study, 480 patients with inducible narrow QRS supraventricular tachycardia (SVT) were included. Twelve-lead electrocardiogram (ECG) was conducted during tachycardia and sinus rhythm. The patients were divided into two groups according to the arrhythmia mechanism that determined via EPS, AVNRT, and AVRT. Criteria of narrow QRS complex tachycardia were compared between the two groups. Results: AVNRT was present in 370 (77%) patients and AVRT in 110 (23%) patients. Combined aVR criterion was found to be more frequent in patients with AVNRT (84.1% and 9.1%, pb 0.001). In logistic regression analysis, combined aVR criterion and classical ECG criterion were found to be the most important predictors of AVNRT (pb 0.001). The sensitivity, specificity, positive predictive value, and negative predictive value of the combined aVR criterion for AVNRT were 84.1%, 90.9%, 96.9%, and 62.9%, respectively.
Conclusion: In the differential diagnosis of patients with SVT, the combined aVR criterion identifies the presence of AVNRT with an independent and acceptable diagnostic value. In addition to classical ECG criteria for AVNRT, it is necessary to evaluate the combined aVR criterion in daily practice.
© 2018 Elsevier Inc. All rights reserved.
Keywords:
Supraventricular tachycardia aVR derivation
Pseudo r′ wave
R′ wave amplitude increase
Introduction
The most common type of supraventricular tachycardia (SVT) is atrioventricular nodal reentrant tachycardia (AVNRT), and the most common AVNRT type is typical AVNRT [1,2]. In typical AVNRT, the antegrade conduction occurs from the“slow pathway” and retrograde conduction occurs from the“fast pathway.” Therefore, it is also called “slow-fast AVNRT.” The 12-lead electrocardiogram (ECG) during tachy-cardia and sinus rhythm provides important information about the eti-ology in patients with SVT. The noninvasive differential diagnosis of AVNRT and atrioventricular reciprocating tachycardia (AVRT) with
12-lead ECG before ablation gives important information regarding the se-lection of the catheter and the ablation method (radiofrequency [RF] or cryoablation), informing the patient and his/her relatives, process suc-cess, avoidance of radiation exposure, duration of the procedure, and complications.
Some studies have investigated the differential diagnosis of tachy-cardia using 12-lead ECG in patients with SVT [3–14]. Most of these studies have been done a decade ago. A few studies have also been con-ducted in recent years. [3,6,7]. The classic ECG criterion for AVNRT, ac-cepted by the 2015 American College of Cardiology/American Heart Association/Heart Rhythm Society (ACC/AHA/HRS) adult SVT treatment guidelines, is the pseudo r′ wave in V1 lead and pseudo s wave in infe-rior leads (DII, DIII, and aVF) [1]. Although it is not used in routine prac-tice, a few studies have investigated the discriminative ability of the aVR derivation in patients with SVT [3–7]. In a previous study, ST segment elevation in the aVR was found to indicate AVRT as the tachycardia
⁎ Corresponding author at: Department of Cardiology, University of Health Sciences -Adana Health Practice and Research Center, Dr. Mithat Özsan Bulvarı Kışla Mah. 4522 Sok. No: 1 Yüreğir, Adana, Turkey.
E-mail address:drmevlutkoc@gmail.com(M. Koc).
https://doi.org/10.1016/j.jelectrocard.2018.08.027 0022-0736/© 2018 Elsevier Inc. All rights reserved.
Contents lists available atScienceDirect
Journal of Electrocardiology
j o u r n a l h o m e p a g e :w w w . j e c g o n l i n e . c o mmechanism [4]. In this study, retrograde P waves in AVRT were thought to cause ST segment elevation [4]. Haghjoo M. et al. [3] showed that a retrograde P wave may cause a pseudo r′ deflection in aVR due to a short VA interval in patients with AVNRT.
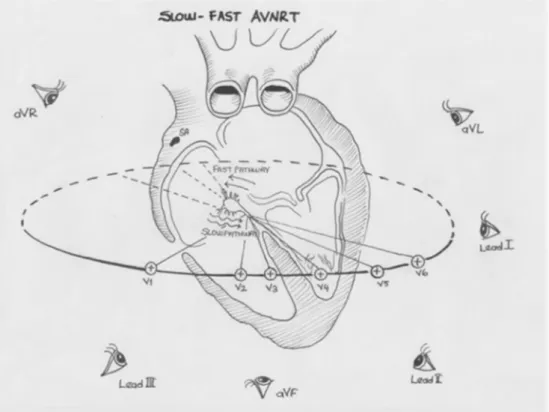
We thought that differential diagnosis of AVNRT with the use of an aVR lead should be evaluated and investigated because of four separate clinical and physiopathological evidences. These include the following: (1) The aVR lead is placed on the opposite side of the retrograde P wave of the slow-fast AVNRT proceeding in the caudo-cranial direction (Fig. 1). For this reason, the greatest positive retrograde P wave should be in aVR. (2) Most of the population with or without SVT in the 12-lead ECG at the sinus rhythm, there is a r′ wave especially in the AVR lead. For this reason, retrograde P wave is added to the basal r′ wave during AVNRT, which increases the current r′ wave. This increase in the r′ wave in the aVR lead does not occur in the AVRT because of the reentry rings length. (3) In populations with normal heart and cardiovascular disease, there may be pseudo r′ wave in V1 and aVR leads in sinus rhythm, so in most AVNRT patients, the amount of increase in the r′ wave must be evaluated instead of the pseudo r′ wave occurrence. (4) In addition, chest leads are not always used in patient monitoring, especially in emergencies, in which case it may be wiser to use an aVR lead instead of V1 during tachy-cardia. That is why we have a new criterion: The combined aVR criterion is defined as (1) the presence of a pseudo r′ wave in the aVR lead during tachycardia in patients without r′ wave in the aVR lead in sinus rhythm and/or (2) a≥50% increase in r′ wave amplitude compared to sinus rhythm in patients with r′ wave in the basal aVR lead.
Thus, we planned to investigate the usefulness of the combined aVR criterion in differential diagnosis of AVNRT and AVRT in patients with SVT. Material and methods
Study protocol and population
In this prospective study, 579 patients who underwent electrophys-iology study (EPS) due to palpitation complaints and narrow QRS
complex SVT between January 2017 and May 2018 were screened. Pa-tients with atrialfibrillation or atrial flutter, structural heart disease, or branch block during sinus rhythm and those who refused to participate in the study were excluded. Patients with two different arrhythmia mechanisms (9 patients), AVRT with multiple accessory pathways (7 patients), atrial tachycardia (AT; 24 patients), bundle branch block dur-ing tachycardia (14 patients), noninducible SVTs (41 patients), and pa-tients whose SVT mechanism could not be clearly identified (4 patients) were excluded from the study. A total of 480 patients (155 men, 325 women; mean age 46.2 ± 8.6 years) with inducible narrow QRS SVT, in which the mechanism of tachycardia is clearly demonstrated and cannot be induced after successful ablation in the EPS, were included in the study. There was narrow QRS complex and 1:1 AV transmission in all patients in the EPS. The study was accepted by our institutional ethics committee. All patients signed an informed consent form before the procedure.
12-Lead electrocardiography
Twelve-lead ECG was conducted in all patients immediately before the start of the EPS procedure and after tachycardia induction with a MAC 2000 ECG Machine (GE Medical, Milwaukee, WI, USA). The classi-cally recommended rate (25 mm/s) and amplitudes (10 mm/mV) were used for ECG acquisition in order to standardize the procedure in all pa-tients. The same person performed the ECG during sinus rhythm and tachycardia for each patient to ensure that the chest leads (in particular, V1) were not affected. All ECGs during sinus and tachycardia were eval-uated by two electrophysiologists (D.Y.S. and Y.K.I.) who had at least 5 years of electrophysiological experience and who performed≥200 SVT ablations per year and were unaware of the patient's clinical status, tachycardia mechanism, EPS, or ablation procedure. As a result of this evaluation, in the case of inconsistent results between the two electro-physiologists, a definitive decision was made by a third electrophysiol-ogist in our clinic (M.K.).
Fig. 1. In 12-lead electrocardiography, each of the 12 leads can be thought of as looking at the heart from a different direction. The aVR lead is placed on the exact opposite side of the retrograde P wave of the slow-fast AVNRT proceeding in the caudo-cranial direction. For this reason, the greatest positive retrograde P wave should be in aVR.
In 12-lead ECG, 11 criteria were used for discrimination between AVNRT and AVRT. These are (1) development of pseudo r′ wave in V1 during tachycardia in patients without r′ wave in V1 in sinus rhythm (pseudo r′ wave in V1); (2) development of pseudo s wave in inferior leads during tachycardia in patients without s wave in inferior leads in sinus rhythm (pseudo s wave in DII-III-aVF); (3) combination of previ-ous two criteria, pseudo r′ wave in V1 and/or pseudo s wave in DII-DIII-aVF (classical AVNRT criteria); (4) development of notching in aVL dur-ing tachycardia in patients without a notch in aVL in sinus rhythm (notching in aVL); (5) development of pseudo r′ wave in aVR during tachycardia in patients without r′ wave in aVR in sinus rhythm (pseudo r′ wave in aVR); (6) a ≥50% increase in r′ wave amplitude compared to sinus rhythm in patients with r′ wave in the basal aVR lead (≥50% r wave amplitude increase in aVR) (7) development of pseudo r′ wave in aVR and/or≥50% r′ wave amplitude increase in aVR (combined aVR crite-rion); (8) horizontal or down-sloping ST segment depression of ≥2.0 mm 80 ms after J point in inferior and precordial leads (ST segment depression); (9) horizontal and up-sloping≥1.0 mm or downsloping ≥1.5 mm ST segment elevation 80 ms after J point in aVR (ST segment elevation in aVR); (10) detection of retrograde P wave in ST segment or after QRS at least one derivation (retrograde P wave after the QRS); (11)≥1-mm variation in the QRS amplitude in any derivation (QRS alternans).
Electrophysiology and ablation procedure
EPS was conducted on patients with palpitations or SVT. EPS was performed at least 1 week after SVT and after 5 half-lives of anti-arrhythmic drugs. The EPS procedure was performed using the Work-Mate Claris™ device (St. Jude Medical, St. Paul, MN, USA). Right and left inguinal regions were prepared for EPS. One quadripolar and one decapolar catheter were placed to high right atrium (HRA) and coronary sinus (CS) via the left femoral vein. The right ventricular apex quadripolar diagnostic catheter and multicurve RF ablation catheter with long sheath were placed via right femoral vein. If a left concealed accessory pathway was present in the patient, left ventricle access was provided via right femoral artery, and the patient was then heparinized. SVT was induced by routine EPS protocols, and the tachycardia mecha-nism was determined by differential diagnosis maneuvers (AVNRT, AVRT, and other SVT). Successful ablation of arrhythmia was achieved in all patients.
Statistical analysis
All analyses were carried out using SPSS 20.0 (SPSS for Windows 20.0; SPSS Inc., Chicago, IL, USA). Data are expressed as mean ± SD for continuous variables and as percentage for categorical variables. The Shapiro-Wilk test was used to determine the normality, and a p value N 0.05 was defined as normally distributed data. Continuous variables that showed a normal distribution were compared using Student's t-test and analysis of variance. The Mann-Whitney U t-test and Kruskal-Wallis tests were used for nonnormally distributed variables. Categori-cal variables and frequencies were compared using theχ2test.
Statisti-cal significance was defined as a p value b 0.05 for all comparisons. Pearson's and Spearman's correlations were used to examine the rela-tionship between continuous variables. Multivariate, stepwise forward conditional logistic regression analysis was used to determine the inde-pendent predictors of AVNRT diagnosis. All significant parameters in the univariate analysis were selected in the multivariate model. The kappa coefficient was used to examine the interobserver variability of the di-agnostic ECG criteria for differential diagnosis of AVNRT and AVRT. Sen-sitivity, specificity, and predictive values were calculated using the standard statistical formula for the predictive ability of ECG criteria for AVNRT. A receiver-operator characteristic (ROC) curve analysis [15] was carried out to identify the optimal cutoff points of r′ wave ampli-tude increase for the detection of AVNRT. The value of the area under
the curve was calculated as a measure of the accuracy of the test. A two-tailed p value ofb0.05 was considered statistically significant. Results
Electrophysiological and demographic characteristics of study population It was determined that 370 (77%) and 110 (23%) patients had AVNRT and AVRT, respectively. Twenty-five patients were found to have atypical AVNRT. A total of 442 and 38 patients were treated with RF energy or cryoablation, respectively. The patients were divided into two groups as AVNRT and AVRT, and the results were compared be-tween the two groups.
Patients with AVNRT were older, and a higher proportion were fe-male (Table 1). Concealed accessory pathways were found to be in the left lateral, left-right posteroseptal, left posterior, right free wall, and mid-paraseptal regions in patients with AVRT (49, 34, 15, 8, and 4, re-spectively). Cohen kappa values that evaluate interobserver variability wereN90% for all ECG criteria.
Comparison of electrocardiographic parameters
Heart rate in tachycardia was similar between the two groups. All ECG criteria except ST segment elevation in aVR were found to be differ-ent between the two groups (Table 1). Pseudo r′ wave in V1, pseudo s wave in DII-III-aVF, classical AVNRT criteria, notching in aVL, pseudo r′ wave in aVR,≥50% r′ wave increase in aVR, and combined aVR criterion were found to be more frequent in patients with AVNRT (pb 0.05 for all). ST segment depression, retrograde P waves after QRS, and QRS alternans were found to be more frequent in patients with AVRT (pb 0.05 for all).
Diagnostic value of ECG criteria in patients with AVNRT
To measure diagnostic performance of ECG criteria for diagnosing AVNRT patients, we calculated well-known diagnostic measures: sensi-tivity, specificity, positive predictive value (PPV), and negative predic-tive value (NPV). These measures are given inTable 2. The sensitivity, specificity, PPV, and NPV of combined aVR criteria for diagnosing AVNRT patients were 84.1%, 90.9%, 96.9%, and 62.9%, respectively. These values indicated that it is highly recommended to use combined aVR criteria for differential diagnosis of AVNRT (Table 2).
Table 1
Demographic and electrocardiographic characteristics of study groups.
AVNRT n = 370 AVRT n = 110 p value Age (years) 49.3 ± 6.1 35.8 ± 7.3 b0.001 Gender female, n (%) 281 (75.9) 44 (40.0) b0.001 Sinus heart rate (ms) 752 ± 81 762 ± 80 0.280 Tachycardia heart rate (ms) 353 ± 21 298 ± 35 b0.001 Body mass index (kg/m2
) 24.8 ± 2 25.4 ± 4.7 0.235 Disease duration (years) 6.5 ± 2.6 6.0 ± 2.7 0.082 Pseudo r′ wave in V1, n (%) 157 (42.4) 8 (7.3) b0.001 Pseudo s wave in DII-III-aVF, n (%) 132 (35.7) 12 (10.9) b0.001 Classical AVNRT criteria, n (%) 224 (60.5) 20 (18.2) b0.001 Notching in aVL, n (%) 91 (24.6) 7 (6.4) b0.001 Pseudo r′ wave in aVR, n (%) 92 (24.9) 6 (5.5) b0.001 Increased r′ wave by ≥%50 in aVR, n (%) 219 (59.2) 7 (6.4) b0.001 Combined AVR criterion, n (%) 311 (84.1) 10 (9.1) b0.001 ST segment depression, n (%) 70 (18.9) 38 (34.5) 0.001 ST segment elevation in aVR, n (%) 102 (27.6) 40 (36.4) 0.076 Identifiable P wave after the QRS, n (%) 74 (20) 78 (70.9) b0.001 QRS alternans, n (%) 55 (14.9) 32 (29.1) 0.001 AVNRT, atrioventricular nodal reentrant tachycardia; AVRT, atrioventricular reciprocating tachycardia; classical AVNRT criteria, pseudo r′ wave in V1 and/or pseudo s wave in DII-III-aVF; combined AVR criterion, pseudo r′ wave in aVR and/or increased r′ wave by ≥50% in aVR.
Use of the combined aVR criterion in patients with AVNRT
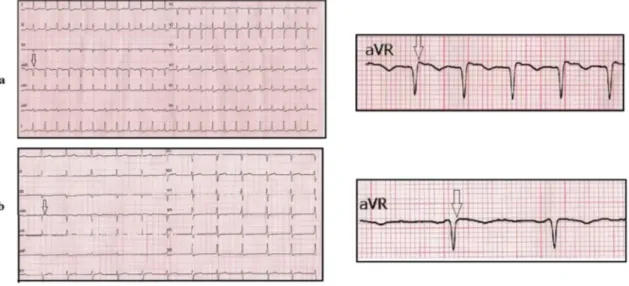
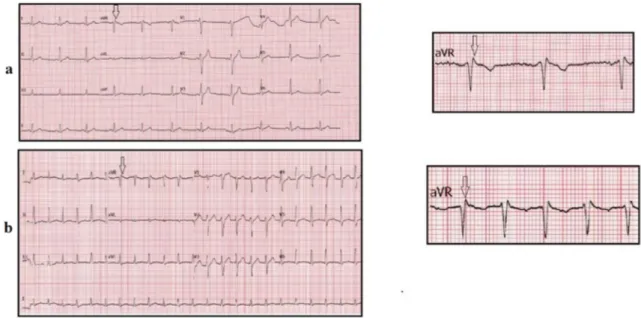
In our study, 20.4% of 480 patients had pseudo r′ in aVR during tachycardia (AVNRT 24.9% and AVRT 5.5%,Fig. 2). During the sinus rhythm, 332 patients (69%) were found to have an r′-wave in the aVR lead (Figs. 3a and4a). A total of 259 (70%) AVNRT patients had an r′ wave in sinus rhythm, and 218 (84.2%) of these patients had≥50% r wave increase during tachycardia (Fig. 3b). Fifty-nine (15.9%) patients with AVNRT did not meet the combined aVR criterion. Twenty-one of these patients had atypical AVNRT with long VA interval (N100 ms). Only 33 of these patients had typical AVNRT diagnosis. A total of 73 (66.4%) AVRT patients had an r′ wave in sinus rhythm, and 66 (90.4%) of these patients did not have≥50% r wave increase during tachycardia (Fig. 4b).
Multivariate analysis of AVNRT diagnosis
All statistically significant parameters in univariate analyses were selected for multivariate analysis. Logistic regression analysis was per-formed to determine the independent ECG criteria for AVNRT diagnosis. Combined aVR and classical AVNRT criteria were found to be indepen-dent criteria for predicting patients with AVNRT (pb 0.001;Table 3). Combined aVR and classical AVNRT criteria were found to increase the possibility of AVNRT by 4.87 (95% confidence interval [CI]: 1.99–8.38) and 3.70 (95% CI: 1.95–7.07), respectively (Table 3).
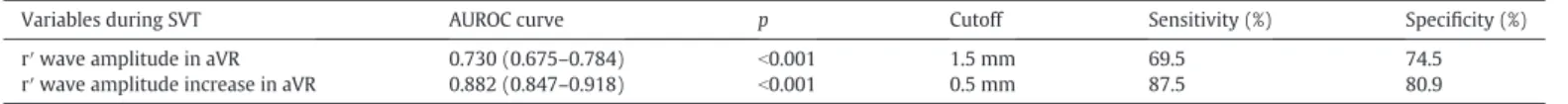
ROC curve analysis to determine predictive value of r′ wave amplitude and r′ wave amplitude increase in aVR during SVT for AVNRT diagnosis
The r′ wave amplitude in aVR during tachycardia and r′ wave ampli-tude increase in aVR during tachycardia were found to predict AVNRT significantly (p b 0.05;Table 4andFig. 5). The cutoff values for r′ wave amplitude and r′ wave amplitude increase during SVT were 1.5 mV (sensitivity: 69.5%, specificity: 74.5%) and 0.5 mV (sensitivity: 87.5%, specificity: 80.9%), respectively.
Discussion
To our knowledge, this is thefirst study to investigate the efficacy of a combined aVR criterion for differential diagnosis of AVNRT. The com-bined AVR criterion is described as (1) the presence of a pseudo r′ wave in aVR lead during tachycardia in patients without r′ wave in aVR lead in sinus rhythm and/or (2) a≥50% increase in r′ wave amplitude in pa-tients with r′ wave in aVR lead in sinus rhythm. The main findings of this study are as follows: (1) The combined aVR criterion was found to be a significant and independent predictor of AVNRT diagnosis. (2) The combined aVR criterion was found to have higher sensitivity, PPV, and NPV than all ECG criteria, including the classic AVNRT criterion recommended in the guideline.
Noninvasive differential diagnosis of AVNRT and AVRT with ECGs in sinus rhythm and tachycardia before EPS procedure is of great value. The correct estimation of the tachycardia mechanism results in reduced ablation duration, reduced radiation exposure, and decreased number of vascular access. This information is also important for patient counseling, physician procedural planning, and logistics. Other than the classical ECG criteria, there are several known ECG criteria in the dif-ferential diagnosis of these two tachycardias [3–14]. Pseudo r′ in V1 [14]; pseudo s in DII, DIII, and aVF [14]; absence of a P wave after QRS or on ST segment; and notching in aVL are well-known ECGfindings that are the results of short RP interval in patients with AVNRT. Retro-grade P wave after QRS [14], ST segment depression in inferior and pre-cordial leads [9,10], ST segment elevation in aVR, and QRS alternans [13,14] are ECGfindings cause by a long RP interval in patients with AVRT. For this reason, AVNRT and AVRT are often distinguished via mea-surement of retrograde RP interval. In typical AVNRT, atrial stimulation is retrogradely conducted by the fast pathwayfirst to this region, then to the septal RA, proximal and distal CS, the upper part of the septum, and thenfinally to HRA [16,17]. This caudo-cranial activation leads to the formation of a positive retrograde P wave in V1 and more prominently
Table 2
Sensitivity, specificity, positive predictive value, and negative predictive value of selected electrocardiographic criteria for the diagnosis of AVNRT.
Sensitivity (%) Specificity (%) PPV (%) NPV (%) Pseudo r′ wave in V1, n (%) 42.4 92.7 95.2 32.4 Pseudo s wave in DII-III-aVF, n (%) 35.7 89.1 91.7 29.2 Classical AVNRT criteria, n (%) 60.5 81.8 91.8 38.1 Notching in aVL, n (%) 24.6 93.6 92.9 27.0 Pseudo r′ wave in aVR, n (%) 24.9 94.5 93.9 27.2 Increased r′ wave by ≥50% in aVR, n
(%)
59.2 93.6 96.9 40.6
Combined AVR criterion, n (%) 84.1 90.9 96.9 62.9 AVNRT, atrioventricular nodal reentrant tachycardia; classical AVNRT criteria, pseudo r′ wave in V1 and/or pseudo s wave in DII-III-aVF; combined AVR criterion, pseudo r′ wave in aVR and/or increased r′ wave by ≥50% in aVR; PPV, positive predictive value; NPV, negative predictive value.
Fig. 2. Typical AVNRT and normal sinus rhythm after conversion via overdrive pacing in our EPS study. (a) The arrows point to the P waves, which are inscribed at the end of the QRS complex, seen best in the inferior leads and as a slightly positive r′ in V1 and aVR (pseudo r′ in V1 and pseudo r′ in V1). Pseudo r′ wave in aVR is more prominent than in V1. (b) When the patient is in sinus rhythm, the arrow indicates where the r′ waves are absent in V1 and aVR.
in AVR and a negative P wave in the inferior leads. Because the aVR lead is an augmented limb lead, it provides more localized information than the bipolar limb leads and gives information about the basal part of RA, right ventricular outflow tract, and septum in particular. Other aug-mented limb leads and bipolar leads are not on the direct opposite side of the retrograde P wave vector. Therefore, we expected the largest positive retrograde P wave to be in the aVR lead, which is placed exactly opposite to the caudo-cranial retrograde P wave. We evaluated the change in the terminal portion of the QRS in the aVR derivation formed by the retrograde P wave. There are several studies and reviews evalu-ating the changes in aVR in patients with AVNRT [3,7,18]. In these stud-ies, the presence of a pseudo r′ wave in the AVR lead and the absence of ST segment elevation were found to be associated with AVNRT. In addi-tion, positive P wave in aVR was also found to be associated with the paraseptal accessory pathways along with AVNRT [18]. ST segment ele-vation in aVR, which may be due to the retrograde P wave, was found to be more frequent in patients with AVRT than AVNRT in previous studies.
Thisfinding was suggested to be used in the differential diagnosis of these two tachycardias [4,7]. However, our results did not support this finding.
In sinus rhythm, the r′ wave must be absent to state that there is a pseudo r′ wave during tachycardia in any derivation such as V1 or aVR. However, we found r′ wave in aVR to be present in 12-lead ECG in sinus rhythm in a large majority (69%) of patients with AVNRT. Therefore, we decided to investigate a novel ECG change: r′ wave ampli-tude increase during tachycardia due to the addition of retrograde P wave to r′ wave in aVR. We found this change to be present in 59.2% of patients with AVNRT. In our study, we found an r′ wave amplitude in-crease≥50% in aVR during tachycardia to be useful to differentiate AVNRT. Thus, we formed a novel ECG criterion with the combination of development of pseudo r′ wave in aVR and/or ≥50% r′ wave ampli-tude increase in aVR, which we described as“combined aVR criterion.” Most of the classical and other ECG criteria used in the diagnosis of AVNRT were described more than a decade ago. The use of the pseudo
Fig. 3. Typical AVNRT and normal sinus rhythm after conversion via overdrive pacing in EPS study. (a) When the patient is in sinus rhythm, the arrow indicates where the prominent r′ waves are in V1 and aVR. (b) The arrows point to the P waves, which are inscribed at the end of the QRS complex, seen best in the inferior leads and as a slightly positive r′ in V1 and aVR (r′ increase by 50% in V1and aVR). The r′ wave increase in aVR is more prominent than in V1.
Fig. 4. AVRT and sinus rhythm after conversion via overdrive pacing in electrophysiological study. In sinus rhythm, the patient had short PR interval (98 msn) and minimal pre-excitation. (a) When the patient is in sinus rhythm, the arrow indicates where the prominent r′ waves are in lead aVR. (b) When the patient is in tachycardia, the arrow indicates r′ waves in lead aVR which doesn't increase.
r′ wave in aVR for the diagnosis of AVNRT has been investigated in only 2 prospective studies [3,6]. Previously, Haghjoo et al. [3] found pseudo r′ in aVR to have higher sensitivity, specificity, PPV, and NPV (67%, 90%, 91%, and 62%, respectively) than the classical AVNRT criteria for deter-mining AVNRT diagnosis. Haghjoo M et al. [3] reported that the fre-quency of pseudo r′ wave in aVR was very high (53.3%). However, Haghjoo et al. did not report the rates of r′ waves in aVR in sinus rhythm and r′ wave amplitude increase. In a recent study by Medeiros et al. [6], ECG criteria such as notching in aVL, absence of retrograde P wave, pseudo r′ wave in aVR, notching in D1, and absence of deflection 100 ms after QRS were tested in addition to classic ECGfindings. In this study, not all these criteria but the presence of pseudo s wave in in-ferior leads and/or pseudo r′ in V1 (classical AVNRT criterion) were found to independently predict the diagnosis of AVNRT. In the same study, the presence of a pseudo r′ wave in aVR was observed in only 25 (10%) of 256 patients with SVT. Ninety-two percent of these 25 pa-tients were AVNRT, and 8% were AVRT. In our study, there was r′ wave in aVR in sinus rhythm in 69% of patients. A total of 20.4% (24.9% with AVNRT and 5.5% with AVRT) of 480 patients had pseudo r′ in aVR. Of these patients, 94% were AVNRT and 6% were AVRT. Our results were concordant with the study of Medeiros JL et al. [6] but were discor-dant with the study of Haghjoo M et al. [3] regarding pseudo r′ wave in aVR during tachycardia. Our study is thefirst in the literature to evaluate the discriminative ability of the novel combined aVR criterion, which is described as the development of pseudo r′ wave in aVR and/or a ≥50% increase in r′ wave amplitude in aVR during tachycardia. The combined aVR criterion was found to be present in 84.1% of patients with AVNRT and in 9.1% of patients with AVRT. We also found combined aVR criteria to have higher sensitivity, specificity, PPV, and NPV (84.1%, 90.9%, 96.9%, and 62.9%, respectively) than all other ECG criteria, even than the classi-cal AVNRT criterion.
In clinical practice, the configuration of the aVR and V1 leads is very similar. In many cardiovascular diseases, these two leads are affected to-gether. In acute coronary syndrome with left main coronary artery or critical 3-vessel disease, ST segment elevation is seen in these two leads with ischemic effect in the basal portion of the septum [4,18,19], and ST segment elevation in AVR is more pronounced than V1 [20]. In acute pericarditis and Takotsubo cardiomyopathy, although there is ST segment elevation in other leads, there is usually ST segment depression in aVR and V1 [21]. Pulmonary embolism also causes ST segment eleva-tion in aVR and V1 leads [18,22]. Our study also showed that the retro-grade positive P wave in patients with AVNRT affects the QRS terminal portion of both leads in a similar way. However, physiopathologically, there should be a more prominent positive P wave in aVR than V1 in pa-tients with AVNRT. Because V1 is placed anteriorly, aVR is placed poste-riorly to the atriums parallel to the caudo-cranial advancement of retrograde P wave. Another significant advantage of aVR relative to V1 is that it can be interpreted by the limb lead connection only, because
the aVR lead is an augmented limb lead. Thus, especially in ambulances, emergency service, and intensive care units, AVNRT diagnosis can be made without a 12-lead connection.
Limitations
Fast-slow and slow-slow AVNRTs also form a positive P wave in the aVR [4]; however, because of the retrograde slow path and long RP in-terval, the formation of the P wave does not coincide with the terminal portion of the QRS. In our study, combined aVR criterion was absent in most cases of atypical AVNRT. Therefore, our combined aVR criterion is useful only in identifying patients with typical AVNRT. Similarly, com-bined aVR criterion is not useful in patients with AT, another type of par-oxysmal SVT, because the P wave can come across QRS with various RP intervals due to lack of steady 1:1 AV conduction.
Conclusion
In differential diagnosis of patients with SVT, the combined aVR cri-terion identifies the presence of AVNRT with an independent and ac-ceptable diagnostic value. In our study, the diagnostic value of this criterion was found to be higher than all of the existing criteria. For this reason, in addition to classical ECG criteria for AVNRT, it is necessary to evaluate the occurrence of pseudo r′ in the aVR and/or ≥50% increase in r′ wave amplitude during tachycardia in daily practice. Combined aVR criterion can be used simply with limb leads only without the need to connect 12 leads.
Conflicts of interest None declared.
Table 3
Independent risk factors for diagnosis of AVNRT in the binary logistic regression analysis.
Presence variable OR 95% CI p Classical AVNRT criteria 3.709 1.945–7.073 b0.001 Combined AVR criterion 4.872 1.994–8.376 b0.001 AVNRT, atrioventricular nodal reentrant tachycardia; classical AVNRT criteria, pseudo r′ wave in V1 and/or pseudo s wave in DII-III-aVF; combined AVR criterion, pseudo r′ wave in aVR and/or increased r′ wave by ≥50% in aVR; CI, confidence interval; OR, odds ratio.
Table 4
ROC analysis for the detection of patients with AVNRT.
Variables during SVT AUROC curve p Cutoff Sensitivity (%) Specificity (%) r′ wave amplitude in aVR 0.730 (0.675–0.784) b0.001 1.5 mm 69.5 74.5 r′ wave amplitude increase in aVR 0.882 (0.847–0.918) b0.001 0.5 mm 87.5 80.9 AVNRT, atrioventricular nodal reentrant tachycardia; SVT, supraventricular tachycardia.
Fig. 5. The ROC curve analysis for r′ wave amplitude and r′ wave amplitude increase during SVT for determining patients with AVNRT.
Funding
This research received no grant from any funding agency in the pub-lic, commercial or not-for-profit sectors.
References
[1]Page RL, Joglar JA, Caldwell MA, et al. 2015 ACC/AHA/HRS guideline for the manage-ment of adult patients with supraventricular tachycardia: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol 2016;67:e27-115. [2]Lockwood D, Otomo K, Wang X, et al. Electrophysiological characteristics of
atrio-ventricular nodal reentrant tachycardia: implications for the reentrant circuits. In: Zipes DP, Jalife J, editors. Cardiac electrophysiology: from cell to bedside. , 4th ed. Philadelphia, PA: Saunders Elsevier Publishing; 2004. p. 537e557.
[3]Haghjoo M, Bahramali E, Sharifkazemi M, Shahrzad S, Peighambari M. Value of the aVR lead in differential diagnosis of atrioventricular nodal reentrant tachycardia. Europace 2012;14:1624–8.
[4]Ho YL, Lin LY, Lin JL, Chen MF, Chen WJ, Lee YT. Usefulness of ST-segment elevation in lead aVR during tachycardia for determining the mechanism of narrow QRS com-plex tachycardia. Am J Cardiol 2003;92:1424–8.
[5]Gonzalez-Torrecilla E, Almendral J, Arenal A, Atienza F, del Castillo S, Fernández-Avilés F. Independent predictive accuracy of classical electrocardiographic criteria in the diagnosis of paroxysmal atrioventricular reciprocating tachycardias in pa-tients without pre-excitation. Europace 2008;10:624–8.
[6]Filgueiras Medeiros J, Nardo-Botelho FM, Felix-Bernardes LC, et al. Diagnostic accu-racy of several electrocardiographic criteria for the prediction of atrioventricular nodal reentrant tachycardia. Arch Med Res 2016;47:394–400.
[7]Jain D, Nigam P, Indurkar M, Chiramkara R. Clinical significance of the forsaken aVR in evaluation of tachyarrhythmias: a reminder. J Clin Diagn Res 2017;11:OM01–4. [8]Tai CT, Chen SA, Chiang CE, et al. A new electrocardiographic algorithm using
retro-grade P waves for differentiating atrioventricular node reentrant tachycardia from atrioventricular reciprocating tachycardia mediated by concealed accessory path-way. J Am Coll Cardiol 1997;29:394–402.
[9]Jaeggi ET, Gilljam T, Bauersfeld U, Chiu C, Gow R. Electrocardiographic differentiation of typical atrioventricular node reentrant tachycardia from atrioventricular recipro-cating tachycardia mediated by concealed accessory pathway in children. Am J Cardiol 2003;91:1084–9.
[10]Riva SI, Della Bella P, Fassini G, Carbucicchio C, Tondo C. Value of analysis of ST seg-ment changes during tachycardia in determining type of narrow QRS complex tachycardia. J Am Coll Cardiol 1996;27:1480–5.
[11]Green M, Heddle B, Dassen W, Wehr M, Abdollah H, Brugada P, et al. Value of alter-nation in determining the site of origin of narrow QRS supraventricular tachycardia. Circulation 1983;68:368–73.
[12]Di Toro D, Hadid C, Lopez C, Fuselli J, Luis V, Labadet C. Utility of the aVL lead inlectrocardiographic diagnosis of atrioventricular node re-entrant tachycardia. Europace 2009;11:944–8.
[13]Morady F, DiCarlo L, Baerman JM, de Buitleir M, Kou WH. Determinants of QRS alternans during narrow QRS supraventricular tachycardias. J Am Coll Cardiol 1987;9:489–99.
[14]Kalbfleisch SJ, El-Atassi R, Calkins H, Lanberg JJ, Morady F. Differentiation of paroxys-mal narrow QRS complex tachycardias using the 12-lead electrocardiogram. J Am Coll Cardiol 1993;21:85–9.
[15] Unal I. Defining an optimal cut-point value in ROC analysis: an alternative approach. Comput Math Methods Med 2017;2017(14):3762651.https://doi.org/10.1155/ 2017/3762651.
[16]Sung RJ, Waxman HL, Saksena S, Juma Z. Sequence of retrograde atrial activation in patients with dual atrioventricular nodal pathways. Circulation 1981;64:1059–67. [17]Amaty Leon F, Dhingra RC, Wu D, Denes P, Wyndham C, Rosen KM. Catheter
map-ping of retrograde atrial activation. Observations during ventricular pacing and AV nodal re-entrant paroxysmal tachycardia. Br Heart J 1976;38:355–62.
[18]Gorgels AP, Engelen DJ, Wellens HJ. Lead aVR, a mostly ignored but very valuable lead in clinical electrocardiography. J Am Coll Cardiol 2001;38:1355–6.
[19]Hurst JW. Methods used to interpret the 12-lead electrocardiogram: pattern memo-rization versus the use of vector concepts. Clin Cardiol 2000;23:4–13.
[20]Yamaji H, Iwasaki K, Kusachi S, et al. Prediction of acute left main coronary artery ob-struction by 12-lead electrocardiography: ST segment elevation in lead aVR with less ST-segment elevation in lead V1. J Am Coll Cardiol 2001;38:1348–54. [21]Zhong-qun Z, Chong-quan W, Sclarovsky S, Nikus KC, Chao-rong H, Shan M.
ST-segment deviation pattern of takotsubo cardiomyopathy similar to acute pericardi-tis: diffuse ST-segment elevation. J Electrocardiol 2013;46:84–9.
[22]Sreeram N, Cheriex EC, Smeets JL, Gorgels AP, Wellens HJ. Value of the 12-lead elec-trocardiogram at hospital admission in the diagnosis of pulmonary embolism. Am J Cardiol 1994;73:298–303.