Saudi J Kidney Dis Transpl 2020;31(2):528-532
© 2020 Saudi Center for Organ Transplantation
Case Report
Mesalazine Induced Focal Segmental Glomerulosclerosis in a Patient
with Ulcerative Colitis
Fatih Yılmaz1, Bora Uslu2, Bahar Akkaya3, Ramazan Cetinkaya4 1
Department of Nephrology, Antalya Atatürk State Hospital, Antalya,2Department of Nephrology, Liv Hospital, University of Istinye, Istanbul, Departments of3Pathology and4Nephrology, Akdeniz
University, Faculty of Medicine, Antalya, Turkey
ABSTRACT. Focal segmental glomerulosclerosis (FSGS) and other glomerulonephritis due to the use of 5-aminosalicylic acid derivatives have been reported in the literature. A 38-year-old male who had been using mesalazine for four years because of ulcerative colitis applied to doctor due to swelling in the lower extremities. The patient was diagnosed with nephrotic syndrome (NS). Renal biopsy was performed, and FSGS was diagnosed. Antiproteinuric treatments were initiated with steroid therapy. The patient has been followed with the normal renal function of the after treatment. 5-aminosalicylic acid derivatives affect renal functions at different levels and caused in NS.
Introduction
Ulcerative colitis (UC) affects the colon mucosa and extra intestinal findings may be seen unrelated to disease activity. Renal problems in inflammatory bowel disease (IBD) are frequently associated with calcium oxalate stones, stone-related pyelonephritis and hydronephrosis, and amyloidosis associated with disease duration.1 Local and systemic forms of 5-aminosalicylic acid (5-ASA) deri-vatives are used in the first-line treatment of
Correspondence to: Dr. Fatih Yilmaz,
Department of Nephrology, Antalya Atatürk State Hospital, Antalya, Turkey.
E-mail: fthylmz79@gmail.com
mild-to -moderate IBD. 5-ASA derivatives affect the kidneys as idiosyncratic and dose-dependent manner. Acute and chronic tubulo-interstitial nephritis (TIN) due to hypersensi-tivity reactions frequently develop as idio-syncratic, while analgesic nephropathy with cyclo-oxygenase enzyme inhibition is predo-minantly dose dependent.2 Minimal change disease presenting with nephrotic syndrome (NS) due to 5-ASA has been reported in both UC3-5 and Crohn’s disease.6
Focal segmental glomerulosclerosis (FSGS) is glomerular diseases had podocyte injury predominates7and characterized by NS, hyper-tension, and progressive deterioration in renal function. FSGS is the primary glomerular disease most commonly associated with end-stage renal failure.8 FSGS has also been reported as a case presentation in patients with
Saudi Journal
of Kidney Diseases
and Transplantation
UC.9,10In this case report, we present a patient who developed FSGS due to mesalazine usage and the improvement of renal function with short-term high-dose steroid treatment.
Case Report
Informed consent was obtained from the patient before publishing the case.
A 38-year-old male admitted to a nephrology clinic due to bilateral lower limbs edema and weight gain during one month. He got 8 kg during this period. He had UC for four years and used mesalazine 1500 mg/day. For the past two years, the disease was clinically at remission and there was no evidence of extra intestinal disease. On physical examination, arterial blood pressure was 127/74 mm Hg, pulse rate was 84/min, and fever was 36.3°C. System examinations were at normal limits. There were three positive edemas at the lower extremities. There were no arthralgia and skin rash.
There were 3+ protein, 2 red cells per area, and 4 leukocytes at the urine analysis. Dysmorphic erythrocyte and erythrocyte leu-kocyte casts were not observed in the micros-copic analysis of the urine. 24-h urine protein level was 8054 mg/day. Laboratory tests were blood urea nitrogen: 18 mg/dL, serum crea-tinine: 0.8 mg/dL, sodium: 141 meq/L, potas-sium: 4.3 meq/L, albumin: 2.8 g/dL, white blood cell: 9250/mm3, hemoglobin: 14.5 g/dL, platelets: 265.000/µL, C-reactive protein: 0.5 mg/dL, and erythrocyte sedimentation rate: 32 mm/h. Serologic tests for antinuclear anti-bodies, anti-dsDNA, cytoplasmic, and peri-nuclear anti-neutrophil cytoplasmic antibodies, antiglomerular basement membrane antibody, serum immunoglobulins G, A, M, rheumatoid factor, and complement (C3, C4) were all normal.
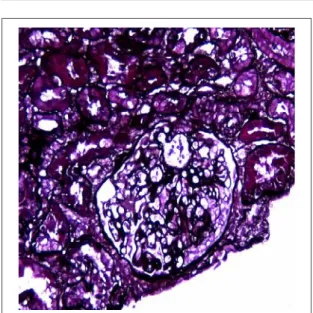
Renal ultrasonography was normal. The patient was diagnosed NS and renal biopsy was performed. Segmental sclerotic changes were observed in four of eight glomeruli at biopsy. Immunoglobulin G, A, M, C3c, kappa, lambda, and fibrinogen were detected negative in immunofluorescence analysis. Crystal violet
and Congo red were detected negative and there was no evidence of interstitial nephritis. Pathological findings were compatible with FSGS and secondary FSGS diagnosis was made (Figure 1a-c).
Methylprednisolone (MP) 1 mg/kg/day, rami-pril 10 mg/day, and valsartan 320 mg/day were initiated for treatment to the patient. Mesalazine treatment was stopped immediately. There was no activation at UC afterwards. MP was rapidly
Figure 1. (a) Renal biopsy by light microscopy, Segmental capillary obliteration in the glomerulus, sclerosis area (H and E; ×200).
Figure 1. (b) Renal biopsy by light microscopy, Segmental capillary obliteration in the glomerulus, sclerosis area (H and E, ×200).
Figure 1. (c) Renal biopsy by light microscopy, glomerulosclerosis and visceral epithelium proliferation (Periodic acid–Schiff; ×200).
reduced after the 1st month and decreased at the end of the 3rd month to 4 mg/day. At the end of the 3rdmonth with steroid therapy, proteinuria decreased to 2853 mg/day. At the 9th month, MP therapy was discontinued. The follow-up in 60 months is renal functions were normal and no proteinuria. The patient’s laboratory results in admission and follow-up are shown in Table 1.
Discussion
The most common side effects associated with to use 5-ASA are a headache, vomiting, dyspepsia, skin reactions, pancreatitis, and
TIN.11,12 Mesalazine, olsalazine, and balsalazine have been developed due to side effects of sulfapyridine in the content of the original molecule sulfosalasine. Mesalazine is a slow-release preparation containing only 5-ASA and has a lower profile of side effects. Renal impairment in IBD can occur as an extra-intestinal finding of disease, often seen as acute kidney injury, glomerular abnormalities, and tubular proteinuria.11
5-ASA usage can cause renal damage as acute reversible TIN due to cyclooxygenase enzyme inhibition, dose-dependent analgesic nephropathy, and chronic TIN. Acute and chronic TIN frequently occurs in a dose-dependent manner. Ultrastructural changes similar to those of phenacetin and salicylic acid can be observed with 5-ASA due to inhi-bition of cyclooxygenase enzyme, but papil-lary necrosis is very uncommon.13 Significant TIN findings were not observed in our patient. Although it is associated with TIN and 5-ASA usage, tubular proteinuria correlates with IBD activity, thus indicating that chronic TIN has extraintestinal involvement.14 Although nephro-toxicity due to 5-ASA is often seen within the 1st year after treatment, it has been reported some cases seen after few years later.15 In our patient, NS developed four years later after treatment. In a study evaluating renal disease associated with 5-ASA use, 130 of 19025 patients using 5-ASA for IBD developed renal disease and the incidence was found 0.17/100 patient-years.13 Elseviers et al followed 1529 patients using 5-ASA due to IBD for one year,
Table 1. Laboratory data at admission and during follow-up.
Parameters Admission 1 month 3 months 6 months 12 months 36 months 60 months References Creatinine (mg/dL) 0.80 0.78 0.90 0.86 0.83 0.84 0.88 0.6–1.1 CKD-EPI eGFR (mL/min/1.73 m2) 95.1 112.1 97.8 109.2 108.7 108.6 105.2 Female: 90–110 Male: 90–120 Albumin (g/dL) 2.8 3.8 4.3 4.3 4.4 4.7 4.5 3.5–5.2 LDL-C (mg/dL) 196 128 107 97 121 116 150 70–130 24 h urine proteinurea (mg/day) 8054 3474 2853 1273 511 96 108 <150 mg/day
CKD-EPI eGFR: Chronic kidney disease epidemiology collaboration estimated glomerular filtration rate, LDL-C: Low-density lipoprotein cholesterol.
and at 34 patients, creatinine clearance de-creased and chronic kidney disease developed in 13 of these patients.16
When mesalazine-induced nephrotoxicity develops, the drug should be discontinued immediately and during follow-up period if there is no improvement in renal function, biopsy should be performed to confirm the diagnosis. Short-term high-dose steroid the-rapy is recommended.15 Delay in diagnosis may lead to permanent renal damage. In our patient, late state kidney damage developed, mesalazine treatment was stopped imme-diately, and proteinuria recovered rapidly after steroid therapy was started. The patient’s renal function has been normally followed 36 months after treatment. Patients who used mesalazine with UC and developed NS and their clinical features are summarized in Table 2 according to the literature.
In our patient, NS developed 48 months after mesalazine usage, but the earliest five3 and latest one 844 months later have been reported in the literature. “KDIGO Clinical Practice
Guideline for Glomerulonephritis” recommends a daily dose of MP 1 mg/kg/day (maximum: 80 mg/day) as the initial treatment for minimal change disease and FSGS in adult patients. This treatment is recommended for up to four weeks, followed by high doses of steroid therapy until 16 weeks if complete remission is gained, and later stopping steroid treatment within six months.19 All of the cases in the literature had different durations and doses of steroid use and shorter period than the recom-mended duration, but all had good response. Cyclosporine was used at two patients17,18 because of steroid resistance and good response was obtained. In our case, 1 mg/kg MP was used in the 1stmonth and steroid dose was reduced to 4 mg/day at the 3rdmonth. At the end of the 60th month, renal function was normal and proteinuria was not detected.
In conclusion, renal disease associated with 5-ASA use is a defined side effect of treat-ment, but the incidence is low. There is no guideline suggestion on the monitoring of renal function at during 5-ASA derivatives
Table 2. Summary of reported mesalazine-induced nephrotic syndrome cases 1988–2016
Case no.
Year/
Reference Gender Age
Type of IBD Treatment of IBD and duration mesalasine treatment Type of NS Treatment of NS Outcome 1 19883 Female 61 UC Mesalazine 5 months MCD Prednisone (1 mg/kg/day) Improved 2 19974 Male 44 UC Mesalazine
84 months MCD Steroid Improved 3 19985 Female 59 UC Mesalazine
9 months MCD Steroid Improved
4 20037 Male 33 UC Sulfasalazine+ Mesalazine 12 months FSGS Steroid (1 mg/kg/day) + Ramipril 5 mg/day Improved 5 20138 Female 15 UC Mesalazine FSGS +
AIN Prednisone Improved 6 201217 Male 21 UC Mesalazine 36 months ? Prednisone Cyclosporine Improved 7 201618 Male 17 UC Mesalazine MCD Prednisolone (35 mg/day) + Cyclosporine (250 mg/day) Improved
IBD: Inflamatuary bowel disease, NS: Nephrotic syndrome, UC: Ulcerative colitis, MCD: Minimal change disease, FSGS: Focal segmental glomerulosclerosis, AIN: Acute interstitial nephritis.
usage. More frequent after the 1st month of mesalazine use and twice a year may be a reasonable approach in terms of the early recognition of kidney damage following renal function.
Conflict of interest: None declared. References
1. De Broe ME, Stolear JC, Nouwen EJ, Elseviers MM. 5-Aminosalicylic acid (5-ASA) and chronic tubulointerstitial nephritis in patients with chronic inflammatory bowel
disease: İs there a link? Nephrol Dial
Transplant 1997;12:1839-41.
2. Siveke JT, Egert J, Sitter T, et al. 5-ASA therapy and renal function in inflamatory bowel disease. Am J Gastroenterol 2005; 100:501.
3. Novis BH, Korzets Z, Chen P, Bernheim J. Nephrotic syndrome after treatment with 5-aminosalicylic acid. Br Med J (Clin Res Ed) 1988;296:1442.
4. Fornaciari G, Maccari S, Borgatti PP, et al. Nephrotic syndrome from 5-ASA for ulcerative colitis? Complicated by carcinoma of the colon and sclerosing cholangitis. J Clin Gastroenterol 1997;24:37-9.
5. Skhiri H, Knebelmann B, Martin-Lefevre L, Grunfeld JP. Nephrotic syndrome associated with inflammatory bowel disease treated by mesalazine. Nephron 1998;79:236.
6. Firwana BM, Hasan R, Chalhoub W, et al.
Nephrotic syndrome after treatment of Crohn’s
disease with mesalamine: Case report and literature review. Avicenna J Med 2012;2:9-11.
7. Schell C, Huber TB. New players in the pathogenesis of focal segmental glomerulo-sclerosis. Nephrol Dial Transplant 2012;27: 3406-12.
8. D’Agati VD, Kaskel FJ, Falk RJ. Focal
segmental glomerulosclerosis. N Engl J Med 2011;365:2398-411.
9. Fofi C, Nicoletti MC, Onetti Muda A, Giulio S. Focal segmental glomerulosclerosis with IgA deposits in a patient with ulcerative colitis. G Ital Nefrol 2003;20:641-4.
10. Chirumamilla SR, He C, Racusen LC, Scheimann AO, Cuffari C. Acute kidney injury in a girl with ulcerative colitis and cytomegalo-virus induced focal segmental glomerular sclerosis. World J Pediatr 2013;9:84-6.
11. Corrigan G, Stevens PE. Review article:
İnterstitial nephritis associated with the use of
mesalazine in inflammatory bowel disease. Aliment Pharmacol Ther 2000;14:1-6.
12. Tekin F, Ozütemiz O, Ilter T. Acute tubulo-interstitial nephritis due to 5-aminosalicylic acid in a patient with ulcerative colitis and chronic renal failure. Turk J Gastroenterol 2006;17:153-4.
13. Van Staa TP, Travis S, Leufkens HG, Logan RF. 5-aminosalicylic acids and the risk of renal disease: A large British epidemiologic study. Gastroenterology 2004;126:1733-9.
14. Fraser JS, Muller AF, Smith DJ, Newman DJ, Lamb EJ. Renal tubular injury is present in acute inflammatory bowel disease prior to the introduction of drug therapy. Aliment Pharmacol Ther 2001;15:1131-7.
15. Gisbert JP, González-Lama Y, Maté J. 5-Aminosalicylates and renal function in inflam-matory bowel disease: A systematic review. Inflamm Bowel Dis 2007;13:629-38.
16. Elseviers MM, D’Haens G, Lerebours E, et al. Renal impairment in patients with inflam-matory bowel disease: Association with aminosalicylate therapy? Clin Nephrol 2004; 61:83-9.
17. Sameshima S, Koketsu S, Okuyama T, et al. Ulcerative colitis associated with nephrotic syndrome after treatment with mesalazine developed into rectal carcinoma: A case study. World J Surg Oncol 2016;14:192.
18. The KDIGO practice guideline on glomerulo-nephritis. Kidney Int Suppl 2012;2:143-53. 19. Xinmei Z, Yan C. Nephrotic syndrome and
Moya-moya syndrome in a patient with ulcerative colitis. Inflamm Bowel Dis 2012;18: E798-800.
Date of manuscript receipt: 13 November 2018. Date of revised copy receipt: 30 December 2018. Date of final acceptance: 1 January 2019.