results in borderline spectrum of the disease with a tendency to upgrade toward the tuberculoid form or downgrade to the lepro-matous pole. BL leprosy is characterized by multiple skin lesions tending toward symmetry.1,2 The disease typically begins as hypopigmented or copper-colored macules which pro-gressively become indurated, forming plaques and nodules. Peripheral nerve trunks are thickened, and nerve involvement also tends to be bilaterally symmetrical. Severe nerve damage is characteristically seen with longstanding disease or in reac-tional episodes.1,2 Several atypical presentations of leprosy have been reported with disease masquerading as pityriasis versicolor, sarcoidosis, granuloma annulare, leishmaniasis, xan-thomatosis, psoriasis, pityriasis rosea, lichen planus, and cuta-neous lupus erythematosus.1
The presence of erythematous concentric rings in our patient mimicked the presentation of tinea pseudoimbricata. Tinea pseudoimbricata is a variant of tinea incognito (steroid modified tinea) characterized by multiple pruritic, concentric, erythema-tous, scaly, annular plaques that mimic tinea imbricata caused by Trichophyton concentricum.3,4
Akin to tinea pseudoimbricata, partial immunosupression caused by application of topical corticosteroids might explain the atypical presentation in our case hitherto rare in leprosy. We propose the term “leprosy pseudoimbricata” for such patients of steroid modified leprosy presenting as concentric rings. Because of such obfuscating presentation, the disease can easily be misdiagnosed. The index of suspicion needs to be high for early diagnosis of such cases in order to prevent permanent disability and interrupt transmission to close con-tacts.
Sheetanshu Kumar1
,
MD Hitaishi Mehta1,
MBBSDivya Aggarwal2
,
MD Debajyoti Chatterjee2,
MD, DM Tarun Narang1*,
MD, MNAMSSunil Dogra1
,
MD, MNAMS, FRCP1
Department of Dermatology, Venereology and Leprology, Postgraduate Institute of Medical Education and Research, Chandigarh, India 2
Department of Histopathology, Postgraduate Institute of Medical Education and Research, Chandigarh, India *E-mail: narangtarun@yahoo.co.in Conflict of interest: None.
Funding source: None. doi: 10.1111/ijd.14783
References
1 Kundakci N, Erdem C. Leprosy: a great imitator. Clin Dermatol 2019; 37: 200–212.
2 Lastoria JC, Abreu MA. Leprosy: review of the epidemiological, clinical, and etiopathogenic aspects - part 1. An Bras Dermatol 2014; 89: 205–218.
3 Singal A, Jakhar D, Kaur I, et al. Tinea pseudoimbricata as a unique manifestation of steroid abuse: a clinico-mycological and dermoscopic study from a Tertiary Care Hospital. Indian Dermatol Online J 2019; 10: 422–425.
4 Lim SP, Smith AG. "Tinea pseudoimbricata": tinea corporis in a renal transplant recipient mimicking the concentric rings of tinea imbricata. Clin Exp Dermatol 2003; 28: 332–333.
Gabapentin treatment in notalgia paresthetica: a
preliminary report
Dear Editor,
Notalgia paresthetica (NP) is an isolated sensory neuropathy involving the dorsal spinal nerves. The typical presentation is an itching, well-circumscribed, hyperpigmented patch located uni-laterally on the scapular region occasionally accompanied by paresthesia and/or hyperesthesia. The pathogenesis remains
(a)
(b)
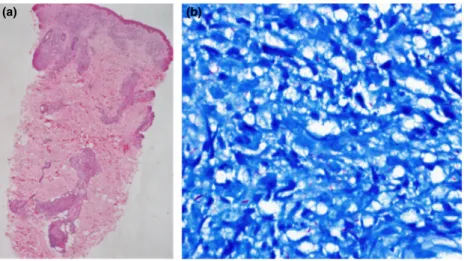
Figure 2 (a) Thinned out and flattened epidermis with preserved grenz zone. The dermis showed perivascular and periadnexal lymphohistiocytic collection with vague granuloma formation, while perineural involvement was noted in deeper dermis (H&E,940). (b) Fite stain for lepra bacilli was strongly positive
ª 2019 The International Society of Dermatology International Journal of Dermatology 2020, 59, e102–e128 Correspondence e125
unclear; however, it is most likely an entrapment syndrome involving the posterior rami of T2–T6 nerve roots sometimes associated with degenerative changes of the vertebrae. Other theories involve hereditary predisposition, increased dermal innervation, or neurotoxicity because of certain chemicals.1,2
We used gabapentin in a small series of consecutive patients with NP (eight female and one male) admitted to the dermatol-ogy outpatient clinic complaining of dermal patches, pruritus, and/or burning-intruding pain on the back (Fig. 1). Patients were well-informed, and seven accepted and consented to a 6-month course of 2,400 mg/day gabapentin therapy for pain and pares-thesia. Gabapentin was started at a dose of 300 mg/day and titrated gradually to the target dose of 2,400 mg/day in all patients. Before the onset of therapy and 6 months after treat-ment, patients were requested to grade their symptoms of pruri-tus, pain, or paresthesia on a scale of 0–10 (0 as no symptoms and 10 as the worst). Treatment success was defined as “at least 3-point decrease” in symptom scores.
The mean age of the patients was 40.8 (30–55) years. Neuro-logical examination and neurophysiologic tests (nerve conduction studies and tibial somatosensory evoked potentials) were normal in all patients. In four (44.4%) patients, there were degenerative changes and minor disc protrusions at T2–T7 levels on MRI. Five patients (71.4%) completed the 6-month course of 2,400 mg/day gabapentin, whereas two patients (28.6%) terminated treatment
early because of adverse effects (severe nausea-vomiting, irri-tability-mood disturbance, and ataxia).
Among five patients who completed the therapy, one (14.3%) patient became completely asymptomatic while 3–4 points (in the 0–10 scale) decrease in symptom scores was noted in four (57.1%) patients compared to pretreatment values. Thus, the overall treatment success-response was 5/7 (71.4%). Patients who completed the therapy complained of mildly disturbing side effects, namely dizziness, somnolence, and nausea.
As stated in the excellent review by Howard et al.,2the treat-ment of NP is challenging. The condition is usually refractory to standard itch-relieving medications. Available modalities are constrained by futile, temporary, and partial outcomes. Consid-ering the chronic nature of the disease, new treatment modali-ties are required.
Gabapentin is an anticonvulsant that binds selectively to a special subunit in calcium channels particularly in the brain and spinal cord and reduces influx into the cells interfering with synaptic transmission.3,4 It also binds to primary sensory neu-rons in the dorsal root ganglia and decreases the ectopic dis-charge and resultant hypersensitivity.3,4 Gabapentin was reported to be beneficial in pruritus associated with sensory neuropathies like brachioradial pruritus and uremia.5–7 Side effects are usually mild (sedation, somnolence), acceptable, and might decline by time. In order to achieve a therapeutic effect, a step-wise titration protocol is recommended, starting with a dose of 300 mg/day and gradually increasing the dose until the desired effect is attained, up to a maximum of 3,600 mg/day. Up to now, only one study and two case reports have documented therapeutic results for gabapentin in NP in a total of 12 patients.8–10There were contradictory outcomes in two case reports; one reporting complete alleviation of itching with gabapentin at a dose of 600 mg/day, whereas the other reported unsatisfactory response to the drug at the same dose.8,9However, in the largest series by Maciel et al.10, pruri-tus was statistically significantly improved in 10 patients with NP who had received gabapentin 300 mg/day for 4 weeks, com-pared to 10 patients with NP who had received topical capsaicin 0.025% for 4 weeks. In our series, overall treatment success was 71.4%, which appears promising. We used gabapentin at a higher dose and for a longer duration of 6 months. A more rig-orous higher quality study with randomization and placebo could not be initially possible because of patient expectancy for urgent therapy and discomfort coming to a referral center. Further large-scale and long-term studies are required to confirm the efficacy of gabapentin treatment in NP.
Funda Uysal Tan1
*,
MD Rabia Soylu Koc1,
MD Emel Erkek Ozturk Durmaz2,
MD Fatma Tuncez Akyurek3,
MD Figure 1 Notalgia paresthetica patient with a unilateralhyperpigmented patch on the lower scapula
International Journal of Dermatology 2020, 59, e102–e128 ª 2019 The International Society of Dermatology Correspondence
1Department of Neurology, Faculty of Medicine, Kirikkale University, Kirikkale, Turkey 2Department of Dermatology, Faculty of Medicine, Kirikkale University, Kirikkale, Turkey 3Department of Dermatology, Faculty of Medicine, Selcuk University, Konya, Turkey *E-mail: fundauysaltan@yahoo.com Funding source: None.
Conflict of interest: None. doi: 10.1111/ijd.14702
References
1 Savk E, Savk O, Bolukbasi O, et al. Notalgia paresthetica: a study on pathogenesis. Int J Dermatol 2000; 39: 754–759. 2 Howard M, Sahhar L, Andrews F, et al. Notalgia paresthetica: a
review for dermatologists. Int J Dermatol 2018; 57: 388–392. 3 Jensen ST, Madsen CS, Finnerup NB. Pharmacology and
treatment of neuropathic pains. Curr Opin Neurol 2009; 22: 467–474.
4 Devor M. How does gabapentin relieve neuropathic pain? Pain 2009; 145: 259.
5 Bueller HA, Bernhard JD, Dubroff LM. Gabapentin treatment for brachioradial pruritus. J Eur Acad Dermatol Venereol 1999; 13: 227–228.
6 Kanitakis J. Brachioradial pruritus: report of a new case responding to gabapentin. Eur J Dermatol 2006; 16: 311–312. 7 Gunal AI, Ozalp G, Yoldas TK, et al. Gabapentin therapy for pruritus in
haemodialysis patients: a randomized, placebo-controlled, double-blind trial. Nephrol Dial Transplant 2004; 19: 3137–3141.
8 Loosemore MP, Bordeaux JS, Bernhard JD. Gabapentin treatment for notalgia paresthetica, a common isolated peripheral sensory neuropathy. J Eur Acad Dermatol Venereol 2007; 21: 1440–1441.
9 Shin J, Kim YC. Neuropathic itch of the back: a case of notalgia paresthetica. Ann Dermatol 2014; 26: 392–394.
10 Maciel AA, Cunha PR, Laraia IO, et al. Efficacy of gabapentin in the improvement of pruritus and quality of life of patients with notalgia paresthetica. An Bras Dermatol 2014; 89: 570–575.
Arcuate pink plaques in a female with Down syndrome
Dear Editor,
A 17-year-old Hispanic female with Down syndrome (DS) pre-sented with a 2-year history of thick, pink, scaly lesions on her abdomen, neck, and upper and lower extremities. She also had a history of multiple hospitalizations for erythroderma. Prior to presentation, her skin findings had been stable in size and num-ber and were intermittently pruritic. Treatment with mid- and high-potency topical steroids resulted in varying efficacy, but at the time of evaluation by dermatology, she was only applying petrolatum. She had no family history of erythroderma and denied joint pain, joint flexibility, or premature aging. She was not on any systemic medications and had never taken penicillamine.
Physical examination revealed arcuate and polycyclic well-de-marcated, thick pink plaques with white scale on the posterior neck, abdomen, bilateral knees, and elbows (Figs. 1 and 2). Some plaques had an erythematous, raised border. There was no umbilication. With this patient’s history of DS and the arcuate morphology of plaques on physical exam, elastosis perforans serpiginosa (EPS) was considered in the differential diagnosis, and thus a biopsy was performed. The differential diagnosis also included psoriasis, granuloma annulare, and dermatophyte infection.
Shave biopsies of the neck and left knee revealed psoriasi-form hyperplasia and parakeratosis. Tortuous dilated capillaries were present in the papillary dermis, and there were collections of neutrophils in the spinous and cornified layers. Periodic Figure 1 Posterior neck. Well-demarcated thick arcuate pink plaques with overlying white scale and surrounding erythematous border
Figure 2 Right lower back. Thick pink arcuate plaques with erythematous borders and thick white scale
ª 2019 The International Society of Dermatology International Journal of Dermatology 2020, 59, e102–e128 Correspondence e127