Vascular Ischemia as a Cause of Transient Global Amnesia: A Patient Series
Geçici Global Amnezi’ye Neden Olan Vasküler İskemi: Hasta Serisi
Özlem GÜNGÖR TUNÇER
1, Bahar AKSAY KOYUNCU
2, Zeynep VİLDAN OKUDAN
1, Ebru ALTINDAĞ
3, Reha TOLUN
4,
Yakup KRESPİ
2Correspondence Address/Yazışma Adresi: Dr. Özlem Güngör Tunçer, Department of Neurology, Istanbul Bilim University Faculty of Medicine, İstanbul, Turkey Phone: +90 212 224 49 50-5602 E-mail: ozlemgtuncer@hotmail.com
Received/Geliş Tarihi: 04.10.2013 Accepted/Kabul Tarihi: 11.12.2013
1Department of Neurology, Istanbul Bilim University Faculty of Medicine, İstanbul, Turkey 2Clinic of Neurology, Şişli Memorial Hospital, İstanbul, Turkey
3Clinic of Neurology, Şişli Florence Nightingale Hospital, İstanbul, Turkey 4Clinic of Neurology, Memorial Hizmet Hospital, İstanbul, Turkey
Introduction: Epileptic, migrainous, and vascular pathologies may cause transient global amnesia (TGA); however, the mechanism of causation remains unclear. We investigated possible vascular causes of TGA. Methods: We retrospectively evaluated the clinical and radiologic studies of 13 patients with TGA. On admission, patients underwent diffusion-weighted imaging (DWI) and intra- and extracranial magnetic resonance angiography (MRA); vascular risk factor profiles for diabetes, hypertension, and hyperlipidemia; electroencephalography; and neuropsychological tests. Seven patients underwent control DWIs 24 h after symptom onset. Results: One patient had two punctiform acute infarcts in the left hippocampus, and one had a left pontine paramedian acute infarct. In the
second patient, control DWI showed additional left hippocampal and right frontal acute infarcts. None of the patients had electroencephalographic evidence of epileptic activity. All patients except for one had at least one vascular risk factor. The second patient was shown to have paroxsysmal atrial fibrillation during follow-up.
Conclusion: Minor posterior circulation ischemic stroke appears to cause TGA in some patients. Evaluations such as DWI and vascular risk factor assessment may be helpful in making the diagnosis.
Keywords: Transient global amnesia, diffusion MR, ischemia
Amaç: Geçici global amnezi (GGA) etyolojisinde, mekanizmaları tam bi-linmemekle beraber epileptik, migrenöz ve vasküler patolojilerin sorumlu olabileceği düşünülmektedir. Bu çalışmamızda, GGA’nın vasküler nedenle-rini araştırmayı amaçladık.
Yöntem: GGA anamnezi ile başvuran 13 hastanın klinik ve radyolojik bil-gileri retrospektif olarak değerlendirildi. Hastaların difüzyon MR, intra ve ekstrakranyal MRanjiografi incelemeleri, vasküler risk faktörlerine yönelik tetkikleri, elektroensefalografi ve nöropsikolojik testleri yapıldı. Yedi has-tanın semptomların başlangıcından 24 saat sonra kontrol difüzyon MR incelemesi yapıldı.
Bulgular: Bir hastada sol hipokampusta iki adet punktiform akut infarkt saptanırken bir hastada da sol pontin paramedyan infarkt izlendi. İkinci
hastanın kontrol difüzyon MR incelemesinde, pontin paramedyan infarkta ek olarak sol hipokampal ve sağ frontal akut infarkt saptandı. Elektroen-sefalografik incelemelerde hiç bir hastada epileptik aktivite izlenmedi. Bir hasta dışında tüm hastalarda en az 1 vasküler risk faktörü saptandı. Akut infarkt saptanan ikinci hastada klinik takipler sırasında paroksismal atrial fibrilasyon tespit edildi.
Sonuç: Posterior sirkülasyon minor inmeleri bazı hastalarda GGA nedeni olabilir. Bu hastalarda difüzyon MR incelemesi ve vasküler risk faktörlerini değerlendirmek tanı ve tedavide yardımcı olabilir.
Anahtar kelimeler: Geçici global amnezi, difüzyon MR, iskemi
ABSTRACT
ÖZET
INTRODUCTION
Transient global amnesia (TGA) is a temporary amnestic condition lasting 1-24h. It is characterized by anterograde and recent retro-grade memory disorders, with loss of place and time orientation but without a disturbance in consciousness (1). The exact cause of TGA is still unknown. Epileptic transient amnesia may be seen in complex partial seizures and mimic TGA but should not be confused with it (2,3). Migraine, physical exercise, emotional stress, sexual intercourse, psychologic disorders, cervical hyperextension, vertebral angiography, and jugular vein incompetency are among the triggering factors/responsible mechanisms (4,5). In addition, recent diffu-sion-weighted magnetic resonance imaging (DWI MRI) studies suggest that delayed detected hippocampal ischemia contributes to the cause of TGA; however, its mechanism remain obscure (6).
In animal studies, migraine has been reported to cause glutamate-mediated transient neuronal and glial depolarization through cortical spreading depression, which in turn affects CA1 neurons in the hippocampus, thereby disrupting cortical integrity and resulting in TGA (7).
©Copyright 2015 by Turkish Association of Neuropsychiatry - Available online at www.noropskiyatriarsivi.com ©Telif Hakkı 2015 Türk Nöropsikiyatri Derneği - Makale metnine www.noropskiyatriarsivi.com web sayfasından ulaşılabilir.
However, the presence of cortical spreading depression in the hippocam-pus has not been confirmed in human studies (8).
Because of its high sensitivity and specificity in detecting ischemia in small areas, DWI MRI has been increasingly used to investigate vascular caus-es of TGA. Studicaus-es often report that the foci of signal increascaus-es in the mesial temporal areas, which is consistent with punctuate and focal isch-emia (4,9). Serial MR studies showing the time dynamics of DWI lesions suggest that the underlying mechanism is delayed ischemia rather than acute focal cerebral ischemia (5,6).
In this study, we looked for evidence of vascular ischemia in patients di-agnosed as having TGA by evaluating their early and late cranial MRI and clinical characteristics.
METHODS
The study was approved by the Institutional Review Board. The data from all patients who presented to the neurology emergency service between January 2006 and January 2011 and in whom TGA was diagnosed were retrospectively analyzed.
All patients underwent cranial MRI, including DWI and intra- and extracranial magnetic resonance angiography (MRA), at presentation. In some of them, a control DWI examination was performed 24 h
after admission. The possibility of an associated epileptic amnesia was assessed with electroencephalography (EEG). The amnestic process was evaluated with neuropsychological tests in some patients. The pres-ence of precipitating factors such as emotional stress, physical activity, vascular risk factors (diabetes, hypertension, and hyperlipidemia), histo-ry of migraine, somatic symptoms during TGA throughout the duration of the episode, and history of similar episodes were determined from the medical records.
RESULTS
We evaluated 13 patients (eight women) between ages 51 and 78 years [mean (SD) age 65 years (11)]. Mean (median−interquartile ranges) duration of symptoms was 8 (8−3.5/11) h (Table 1). Mean interval be-tween the onset of symptoms and MRI examination was 11h.
Infarcts were detected in the early phase in 2 of the 13 patients, whereas 1 of the 7 patients who underwent control DWI imaging had a new lesion in addition to the ischemic lesions detected in the initial DWI. The control DWI study of patient (11) showed no additional findings, whereas patient 13 had additional ischemic infarcts in the left hippocampal and right frontal areas (Table 1). In patient 4, right posterior cerebral artery P2 stenosis was causing a hippocampal perfusion defect despite the absence of an acute ischemic lesion in the same territory. Interestingly, there was a chronic in-farction in the right posterior cerebral artery (PCA) territory (Table 1). Table 1. Clinical and radiological findings in patients with a diagnosis of transient global amnesia
Patient number, Findings from initial Findings from Magnetic
sex, and age, y diffusion-weighted Control diffusion- resonance Vascular risk TGA imaging weighted imaging angiography factors EEG duration, h
1 F 78 - - - HT, HL N 10
2 F 60 - - - HL N 4
3 M 71 - - Left ICA mid cervical - N 2
segment moderate stenosis
4 F 73 - - Lack of flow in right PCA, HT, HL, DM Disorganization in the 1 stenosis of left PCA in P2 anterior of the
and left MCA at M2. hemispheres Extracranial MRA showed
80% and 40% narrowing in left and right ICA.
5 F 64 - - R VA V4 stenosis HL N 6 a 6 M 51 - - - HL, MG N 24 7 M 66 - - - HT, HL N 7.5 8 F 70 - - - HT, HL N 3.5 a 9 F 60 - - - - N 12 10 M 75 - - 7x6 mm bilobulated HT, HL N 10 left PCOMA aneurysm
11 F 56 Two punctuate acute - - HL, MG Disorganization 12 infarcts in the left in the anterior of the
hippocampus, hemispheres
12 M 57 - - - HT, HL, DM Left frontotemporal 3 disorganization 13 F 62 Left pontine Punctuate ischemic - HL, MG Rapid rhythms in the 10a
paramedian acute infarcts in the left anterior of the infarct hippocampus and hemispheres
right frontal areas aA history of TGA
N: normal; MG: migraine; ICA: internal carotid artery; PCA: posterior cerebral artery; MCA: medial cerebral artery; VA: vertebral artery; PCOMA: posterior communicating artery; HT: hypertension; Hl: hyperlipidemia; DM: diabetes mellitus
Eleven patients had at least one of the following vascular risk factors: diabetes mellitus (n=2), hypertension (n=7), or hyperlipidemia (n=11). Three patients had a history of migraine. All patients underwent EEG; patient 11 underwent EEG during the episode and all the other pa-tients underwent EEG after the episode. No papa-tients had an epileptic activity. Three patients had disorganization in the anterior aspects of the hemispheres, and one had rapid rhythms in the anterior aspects of the hemispheres. Neuropsychological evaluations after the attacks showed that eight patients had no amnestic deficits. Symptoms began after an emotional stress in four patients and while driving in two patients. One patient also had paresthesias in the legs during the attack. We would pro-vide detailed information about selected patients with TGA who also had an evidence of vascular ischemia in our series.
Case 1
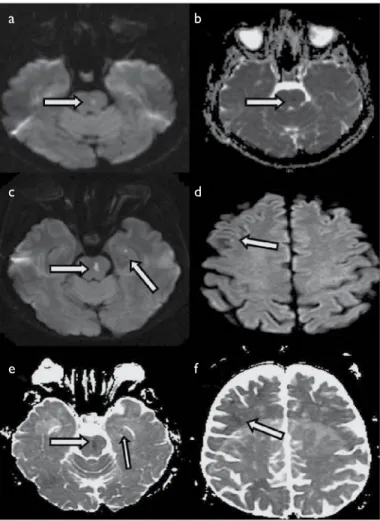
A 56-year-old woman (patient 11) had a history of hyperlipidemia and migraine. Neurologic examination was normal. A DWI MRI taken 7 h after the onset of symptoms showed two hippocampal focal diffusion restriction areas in the medial aspect of the temporal lobe. The re-sults of intra- and extracranial MRA studies were normal (Figure 1). Her symptoms improved after 8 h, although the same lesions were visible in her control DWI MRI taken after 17 h. Except for mild disorganization in the anterior of the hemispheres, EEG results were normal. Electrocardi-ography showed a sinus rhythm, and transesophageal echocardiElectrocardi-ography and Holter monitoring results were normal. Antiplatelet and antihyper-lipidemic treatments were initiated. She had no symptoms during the 1-year follow-up.
Case 2
A 62-year-old woman (patient 13) had an amnestic episode 1 year ago that lasted for approximately an hour. She also had hyperlipidemia and a history of migraine. Results of a neurologic examination were normal. Her symptoms improved within 10 h; however, she had a migraine at-tack 15 h later, which resolved with symptomatic treatment. A DWI MRI taken 7 h after the onset of symptoms showed a paramedian acute isch-emic area in the superior aspects of the left pons. The results of cervical and intracranial MRA and perfusion MR studies were normal (Figure 2). Electrocardiography showed normal sinus rhythm. Transesophageal echo-cardiography, performed to determine the possibility of ischemic stroke with cardioembolic origin, showed the ejection fraction to be 65% and the left atrial diameter to be 3.8 cm, with mild mitral and aortic insuffi-ciency and no evidence of intracardiac thrombus. The control cranial MRI taken 36 h after the onset of symptoms showed additional acute infarct areas in the left hippocampal and right frontal areas, a millimeter-sized diffusion restriction not visible in the initial MRI (Figure 2). Neuropsycho-logical tests revealed only a mild disturbance in long-term spontaneous recall. The anterior aspects of the hemispheres showed rapid rhythm in EEG. Holter monitoring showed paroxysmal atrial fibrillation, and the pa-tient was started on warfarin 3 months after presentation. Her symptoms did not recur during the 1-year follow-up.
Case 3
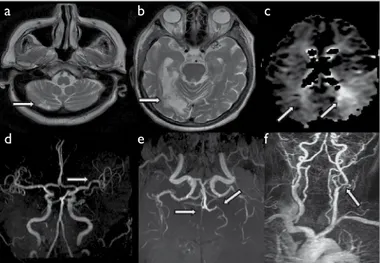
A 73-year-old woman (patient 4) with a history of hypertension, hy-perlipidemia, diabetes mellitus, and ischemic stroke at presentation had TGA. These symptoms improved one hour after onset. Neurologic examination revealed only a left homonymous hemianopsia sequela. No acute ischemic lesions were visible on the DWI taken 3.5 h after symptom onset; however, there were chronic ischemic infarcts in the right cerebellum and right PCA perfusion area (Figure 3). Perfusion MRI showed perfusion defects in the left PCA and left middle cerebral artery
(MCA) inferior perfusion areas. Intracranial MR angiography showed oc-clusion of the right PCA and stenosis of the left PCA in P2 and the left MCA at M2. Extracranial MRA showed 80% and 40% narrowing in the left internal carotid artery (ICA) and right ICA, respectively. Disseminated intra- and extracranial atherosclerosis was suspected. EEG showed disor-ganization in the anterior aspects of both hemispheres. A control DWI MR obtained 24 h after the onset of symptoms showed no new lesions. Because the patient had a history of hypertension, hyperlipidemia, and diabetes, treatment of vascular risk factors was reviewed and anticoagula-tion treatment was continued.
Figure 1. Cranial MRI of case 1(patient number 11). There are 2 punctuate
in-farcts in the left hippocampus, (a) hyperintense in DWI MR, and, (b) hypointense in ADC imaging
a
b
Figure 2. MR images of case 2(patient number 13). (a) Hyperintense lesion of
the left paramedian pons in DWI MR, (b) ADC shows hypointensity in the same location. In the control DWI MR, (c) and (d) shows punctuate DWI MR hyperin-tensity in the left hippocampal and right frontal areas, respectively. Control ADC shows hypointensity in the same locations (e,f)
a
c
e
b
d
f
61DISCUSSION
The prevalence of patients with TGA having lesions detectable by DWI ranges from 52% to 84% (5,6,10). These high rates have been linked to serial MRIs in these studies, which observed that ischemic lesions were mostly detected between 12 and 72 h after symptom onset (10). Enzinger et al. found 14 punctuate lesions in 10 of 86 patients with TGA undergoing DWI, mostly in the mesial temporal areas, hippocampus, den-tate gyrus, cornu ammonis, and the parahippocampal gyrus (4). In our group, 2 out of 13 patients (15%) had an ischemic lesion, and 1 out of 7 patients (13%) had a delayed additional ischemic lesion on control MRI. Functional anatomic analysis of these lesions revealed a selective distribution into the CA1 area of the hippocampal cornu ammonis. It is hypothesized that the selective sensitivity of CA1 neurons to metabolic stress may be the key link in the pathological cascade of TGA. The augmented metabolic stress in these neurons increases the glutamate-mediated intracellular Ca+2
influx; thus, anaerobic glycolysis and the production of lactate are increased. This condition decreases cellular diffusion and causes the transient lesions seen on DWI. These changes reportedly disrupt the CA1 cycle; however, functional compensation is rapid (4-12h) and leads to structural-functional improvements (8). It is considered that these may be the pathophysiologic mechanism of hippocampal dysfunction and TGA lesions.
The hippocampal location of punctuate lesions in our patients is consis-tent with other reports; however, the lesions in the first patient were seen earlier than lesions known as delayed ischemia. In addition, in patient 13, ischemic lesions were seen in various arterial territories in addition to hippocampal lesions, which may indicate an embolic process rather than delayed ischemia.
Amnestic stroke is essentially a condition in which prolonged or perma-nent amnesia secondary to vascular lesions is associated with a focal neu-rologic deficit. The involvement of the hippocampus and parahippocampal gyrus in PCA ischemias may cause hemianopsia, quadrantanopsia, color anomia, and pure alexia in addition to amnesia (11). Hemiparesis,
hemia-taxia, hemi-sensorial, and hemi-visual deficits may also accompany anterior choroidal artery lesions (11). Amnestic syndromes mostly occur after bi-lateral thalamic lesions; however, they may also occur in unibi-lateral thalamic infarcts (12,13). In two of our patients who had lesions consistent with acute ischemia on DWI, no additional neurologic deficit or permanent amnesia pointed to a classical amnestic stroke condition.
Numerous DWI studies have found no lesions in most patients with TGA, and some other DWI studies have reported normal MRI results in patients with TGA (14,15). Performing DWI studies in the early phase of TGA or technical difficulties or limitations in detecting lesions with DWI and ADC defects in small ischemic areas may explain the absence of lesions in many patients. Considering that the hippocampal ischemia was actually responsible for the clinical presentation in patient 13, its absence in the first DWI may indicate that a single DWI may be inadequate and that repeated imaging are required. The presence of infarcts in multiple perfusion areas in this patient suggests an embolic process.
Ischemic lesions in the left mesial temporal lobe (16) and bilateral mesial temporal lobe infarcts have been reported in a patient who experienced TGA after cerebral angiography (17). The presence of ischemic foci in locations other than in the expected hippocampus locations (18,19,20), including in the posterior or even the anterior circulation and in regions which may not result in memory disturbance, may indicate multiple ischemic foci arising from cardioembolism. This finding correlates with the pontine and frontal infarcts that are thought to be unrelated to TGA in patient 13. Ischemia in the posterior circulation other than hippocampus, particularly the vertebrobasilar system, is also linked to TGA (21,22,23). The TGA in patient 4 occurred in the presence of an old temporo- occipital infarct associated with bilateral perfusion deficit in the PCA territory due to widespread intracranial atherosclerosis. The presence of mesial temporal hypoperfusion, including the hippocampus, may have facilitated the development of TGA in the neuronal network of this area.
Although there is no agreement on the contribution of ischemic injury to the occurrence of TGA, ischemic vascular processes appear to con-tribute to the cause in a subset of TGA patients. Our results also strong-ly support vascular ischemia as a cause in some patients. Neuroimaging studies and vascular risk factor assessments are important components of diagnosis.
Conflict of Interest: The authors declared no conflict of interest. Financial Disclosure: The authors declared that this study has re-ceived no financial support.
Çıkar Çatışması: Yazarlar çıkar çatışması bildirmemişlerdir.
Finansal Destek: Yazarlar bu çalışma için finansal destek almadıklarını beyan etmişlerdir.
REFERENCES
1. Hodges JR, Warlow CP. The aetiology of transient global amnesia. A case-con-trol study of 114 cases with prospective follow-up. Brain 1990; 113:639-657.
[CrossRef]
2. Butler CR, Graham KS, Hodges JR, Kapur N, Wardlaw JM, Zeman AZ. The syn-drome of transient epileptic amnesia. Ann Neurol 2007; 61: 587-598. [CrossRef]
Figure 3. MR images of case 3 (patient number 4). (a-b) T2 MRI shows
chron-ic ischemchron-ic infarcts in the right cerebellum and right PCA perfusion areas. (c) Perfusion MRI shows perfusion defects in the left PCA and left MCA inferior perfusion areas. (d,e) Intracranial MR angiography showed lack of flow in the right PCA, stenosis of the left PCA in P2 and the left MCA at M2. (f) Extracranial MRA showed 80% and 40% narrowing in the left ICA and right ICA, respectively. PCA: posterior cerebral artery; MCA: medial cerebral artery; ICA: internal carotid artery.
a
d
b
e
c
f
623. Zeman AZ, Boniface SJ, Hodges JR. Transient epileptic amnesia: a description of the clinical and neuropsychological features in 10 cases and a review of the literature. J Neurol Neurosurg Psychiatry 1998; 64:435-443. [CrossRef]
4. Enzinger C, Thimary F, Kapeller P, Ropele S, Schmidt R, Ebner F, Fazekas F. Transient global amnesia: diffusion-weighted imaging lesions and cerebrovas-cular disease. Stroke 2008; 39:2219-2225. [CrossRef]
5. Sander K, Sander D. New insights into transient global amnesia: recent imaging and clinical findings Lancet Neurol 2005; 4:437-444. [CrossRef]
6. Sedlaczek O, Hirsch JG, Grips E, Peters CN, Gass A, Worhle J, Hennericci M. Detection of delayed focal MR changes in the lateral hippocampus in transient global amnesia. Neurology 2004; 62:2165-2170. [CrossRef]
7. Wernsmann B, Pape HC, Speckmann EJ, Gorji A. Effect of cortical spreading depression on synaptic transmission of rat hippocampal tissues. Eur J Neurosci 2006; 23:1103-1110. [CrossRef]
8. Bartsch T, Deuschl G. Transient global amnesia: functional anatomy and clinical implications. Lancet Neurol 2010; 9:205-214. [CrossRef]
9. Ay H, Furie KL, Yamada K, Koroshetz WJ. Diffusion-weighted MRI charac-terizes the ischemic lesion in transient global amnesia. Neurology 1998; 51:901-903. [CrossRef ]
10. Toledo M, Pujadas F, Grivé E, Alvarez-Sabin J, Quintana M, Rovira A. Lack of evidence for arterial ischemia in transient global amnesia. Stroke 2008; 39:476-479. [CrossRef]
11. Ott BR, Saver JL. Unilateral amnesic stroke. Six new cases and a review of the literature.Stroke 1993; 24:1033-1042. [CrossRef]
12. Akiguchi I, Ino T, Nabatame H, Udaka F, Matsubayashi K, Fukuyama H, Ka-mayama M. Acute-onset amnestic syndrome with localized infarct on the dominant side--comparison between anteromedial thalamic lesion and pos-terior cerebral artery territory lesion. Jpn J Med 1987; 26:15-20.[CrossRef]
13. Goldenberg G, Podreka I, Pfaffelmeyer N, Wessely P, Deecke L. Thalamic isch-emia in transient global amnesia: a SPECT study. Neurology 1991; 41:1748-1752.
[CrossRef]
14. Gass A, Gaa J, Hirsch J, Schwartz A, Hennerici MG. Lack of evidence of acute ischemic tissue change in transient global amnesia on single-shot echo-planar diffusion-weighted MRI. Stroke 1999; 30:2070-2072. [CrossRef]
15. Huber R, Aschoff AJ, Ludolph AC, Riepe MW. Transient Global Amnesia. Evidence against vascular ischemic etiology from diffusion weighted imaging. J Neurol 2002; 249:1520-1524. [CrossRef]
16. Greer DM, Schaefer PW, Schwamm LH. Unilateral temporal lobe stroke causing ischemic transient global amnesia: role for diffusion-weighted imaging in the initial evaluation. J Neuroimaging 2001; 11:317-319. [CrossRef]
17. Woolfenden AR, O’Brien MW, Schwartzberg RE, Norbash AM, Tong DC. Diffusion-weighted MRI in transient global amnesia precipitated by cerebral angiography. Stroke 1997; 28:2311-2314. [CrossRef]
18. Saito K, Kimura K, Minematsu K, Shiraishi A, Nakajima M. Transient global amnesia associated with an acute infarction in the retrosplenium of the corpus callosum. J Neurol Sci 2003; 210:95-97. [CrossRef]
19. Ravindran V, Jain S, Ming A, Bartlett RJ. Transient global amnesia in a patient with acute unilateral caudate nucleus ischemia. J Clin Neurosci 2004; 11:669-672.
[CrossRef]
20. Raffaele R, Tornali C, Genazzani AA, Vecchio I, Rampello L. Transient global am-nesia and cerebral infarct: a case report. Brain Inj 1995; 9:815-8. [CrossRef]
21. Taylor RA, Wu GF, Hurst RW, Kasner SE, Cucchiara BL. Transient global amne-sia heralding basilar artery thrombosis. Clin Neurol Neurosurg 2005; 108:60-62.
[CrossRef]
22. Longridge NS, Hachinski V, Barber HO. Brain stem dysfunction in transient global amnesia. Stroke 1979; 10:473-474. [CrossRef]
23. Milandre L, Donnet A, Rumeau C, Cherif AA, Khalil R. Transient global am-nesia followed by vertebrobasilar ischemia in a case of dolichoectatic basilar artery. Acta Neurol Belg 1990; 90:248-253.