Lower urinary tract symptoms
in women with and without urinary
incontinence
˙Ilkay G ¨ung ¨or, Nezihe Kızılkaya Beji, G ¨uliz Onat Bayram, Habibe Ayyıldız Erkan, S¸ule G ¨okyıldız
and ¨Onay Yalc¸ın
ABSTRACT
Although most women are aware of the more severe end of the spectrum of urinary symptoms, incontinence, there are a myriad of other symptoms that can affect women’s quality of life. The aim of this study is to compare lower urinary tract symptoms (LUTS) and associated factors in women with and without urinary incontinence. This descriptive study compared LUTS and associated factors between 367 incontinent and 401 continent women. LUTS were evaluated with Bristol Female Lower Urinary Tract Symptoms (BFLUTS) questionnaire. LUTS were more common among incontinent women with higher BFLUTS scores, indicating more severe complaints. Filling and voiding symptoms were also common among continent women. The most common symptoms in both groups were urgency, bladder pain, frequency, hesitancy and intermittency. Incontinent women with history of≥4 pregnancy/birth and ≥4 kg fetus had the highest scores. Recurrent infection and flatus were associated with higher scores in both groups. History of diabetes, hypertension and haemorrhoid increased scores among continent women, while pulmonary disease was the only significant medical condition among incontinent women. Overweight and history of≥10 kg weight gain were associated with higher scores among incontinent women. Women with ‘history of incontinence in mother’ had higher scores in continent women while ‘incontinence in relatives’ had more significant effects on BFLUTS scores of incontinent women. LUTS with or without incontinence were common, especially in women with increased parity, high birth weight, chronic diseases diabetes, obesity and family history.
Key words: Incontinence• Lower urinary tract symptoms • Urinary complaints • Urogynecology
BACKGROUND
The term ‘lower urinary tract symptoms’ (LUTS) are an umbrella term that was introduced originally in 1994. It is now recognized that LUTS are a global term that encompasses all urinary symptoms, including storage,
Authors: I Gungor, PhD, Research Assistant, Department of Obstetric
and Gynecologic Nursing, Istanbul University Faculty of Nursing, Istanbul; NK Beji, PhD, Professor, Department of Obstetric and Gynecologic Nursing, Istanbul University Faculty of Nursing, Istanbul; GO Bayram, PhD, Research Assistant, Department of Obstetric and Gynecologic Nursing, Bakırkoy Health School, Istanbul University Health Sciences Faculty, Istanbul; HA Erkan, MSc, Nurse, Istanbul University Istanbul Faculty of Medicine, Capa, Istanbul; S¸ G ¨okyıldız, PhD, Lecturer, C¸ukurova University Adana School of Health, Adana; ¨O Yalc¸in, MD, Professor, Department of Gynecology and Obstetrics, Istanbul Medical Faculty, Istanbul University, Istanbul, Turkey
Address for correspondence: I Gungor, Research Assistant,
Department of Obstetric and Gynecologic Nursing, Istanbul University Faculty of Nursing, Abide-i Hurriyet cad., 34381 Sisli, Istanbul, Turkey
E-mail: ilkay1979@yahoo.com
voiding and postmicturition symptoms. This terminol-ogy links well with the classification proposed by Wein, who suggested that disorders of micturition would be more elegantly characterized as ‘failure to store’ or ‘failure to empty’ (Chapple et al., 2008).
Epidemiological studies during the last decades have shown that LUTS are common in women (Boyle et al., 2003; Norby et al., 2005; Irwin et al., 2006; Kupelian et al., 2006). Urinary incontinence, overac-tive bladder (OAB) and other LUTS are highly prevalent conditions with a profound influence on well-being and quality of life (Milsom, 2009). In a population-based, epidemiological study on LUTS, urinary incontinence and OAB symptoms in adults (18 years old and older) in five countries (Canada, Germany, Italy, Sweden and UK), the general prevalence of LUTS was 67% among females and this rate increased with age (Irwin et al., 2006). Furthermore, the prevalence of LUTS in women was higher than rates reported for other chronic
diseases, such as type 2 diabetes mellitus, which was 5% overall. However, for those older than 65 years of age, LUTS was reported at 15%, asthma was 8% and hypertension was 29% (Beji et al., 2010).
Although most women are aware of the more severe end of the spectrum of urinary symptoms and incontinence, there is a myriad of other symptoms that can affect the health-related quality of women’s life. Despite the substantial negative impact of these symptoms on daily lives, women may not talk about urinary problems with health care providers because of embarrassment and the belief that these symptoms are a normal part of ageing. Health care providers need to be more aware of the impact of urinary symptoms on patients’ lives, more cognizant of the reasons why women hesitate to discuss these problems and more willing to discuss available treatment options (Bradway et al., 2008).
LUTS are not static but dynamic, and many factors may contribute to incidence, progression or remis-sion (Wennberg et al., 2009). Many factors, such as age, childbirth, fecal difficulties, obstetric complica-tions, obesity, pelvic surgery, medicacomplica-tions, functional impairment, chronic diseases, menstrual cycle, race and family history, are associated with urinary inconti-nence and other LUTS (Moller et al., 2000a). It is highly important to determine the factors causing LUTS to select suitable treatment method. There has been a growing interest in these symptoms in recent years as a consequence of the increased awareness of the human and social implications for the individual suf-ferer (Wennberg et al., 2009). An understanding of the prevalence and risk factors of LUTS may help to target treatment resources and provide preventive steps in the future (Zhang et al., 2005).
AIM
The aim of this study was to compare the LUTS and associated factors in women with and without urinary incontinence.
SAMPLE
This descriptive study evaluated the urinary symptoms on a hospital-based sample by comparing the symptoms and associated factors between a continent and an incontinent women group.
This study was conducted in Istanbul University Istanbul Faculty of Medicine between 2007 and 2009. The sample of this study included 367 incontinent women who applied to urogynecology unit and 401 continent women who applied to outpatient gynaecol-ogy clinics with other gynaecological symptoms during
the research period. As the patients of the urogyne-cology unit were women who were referred from the gynaecology clinics with urinary incontinence symp-toms, all women had the clinical diagnosis of urinary incontinence which was defined as any leakage or involuntary loss of urine.
DATA COLLECTION
Data were gathered via face-to-face interviews with a questionnaire prepared by the researchers that addressed sociodemographical, obstetrical and gynae-cological characteristics of women and the factors related to urinary symptoms. The Bristol Female Lower Urinary Tract Symptoms (BFLUTS-SF) questionnaire was also administered to the participants. This ques-tionnaire is a 19-item, multidimensional self-report instrument assessing key dimensions of LUTS, sexual function and quality of life. There are five subscales within the questionnaire. Three subscales focus on incontinence symptoms (BFLUTS-IS), voiding symp-toms VS) and filling sympsymp-toms (BFLUTS-FS). The remaining two focus on sexual function (BFLUTS-sex) and impact on a woman’s quality of life (BFLUTS-Qol). Responses range from none to always, no problem to serious problem and ‘0’ to ‘4’ with higher scores representing the most severe symp-tom. No cut-off values have been established in the literature. BFLUTS was shown to be a reliable tool with a Cronbach’s α of 0·78 (Jackson et al., 1996; Brookes et al., 2004). BFLUTS was translated and adopted into Turkish by G ¨ung ¨or and Yalc¸ın (2005). Cronbach’s α was found as 0·91 in our current study. The question-naires were administered to women while they were waiting for their clinic visit.
The written ethical approval was obtained from the ethical review board of the hospital. Participants were informed about the aims of this study and their verbal consent was obtained prior to the administration of the questionnaire.
DATA ANALYSIS
Data were analysed in SPSS for Windows. The sig-nificance of difference in the frequency of BFLUTS among incontinent and continent women was eval-uated using χ2 test. The significance of difference in mean BFLUTS scores in relation to several vari-ables that might be associated with urinary symp-toms (sociodemographical, obstetrical, gynecologi-cal/medical, lifestyle and incontinence history) was assessed using appropriate analyses including t test, Mann–Whitney, one-way ANOVA and Kruskal–Wallis (Ozdamar, 2003).
Table 1 BFLUTS scores among incontinent and continent women
BLUFTS (minimum–maximum)
Incontinent women BFLUTS mean± SD
Continent women BFLUTS
mean± SD t p Filling 0–15 6·8 ± 3·04 3·35 ± 2·59 −16·854 0·000 Voiding 0–12 2·7 ± 2·7 1·26 ± 1·92 −8·438 0·000 Incontinence 0–20 7·4 ± 3·7 1·15 ± 1·87 −28·854 0·000 Sexual function 0–6 1·26 ± 1·6 0·32 ± 0·78 −10·029 0·000 Quality of life 0–18 8·06 ± 4·4 1·8 ± 2·5 −23·498 0·000 Total BFLUTS 0–71 26·25 ± 11·47 7·9 ± 7·2 −26·170 0·000 BFLUTS, Bristol Female Lower Urinary Tract Symptoms.
RESULTS
The mean ages of women in incontinent and con-tinent groups were 47·3 (SD 10·7) and 42·6 (SD 13·9) years, respectively, and ages ranged between 20 and 80 years. Age group between 40 and 49 ages con-stituted more than 35% of the women in both groups. Most of the women in both groups were married, housewives and primary school or over graduates.
Comparative analysis revealed significant differ-ences (p < 0·05) in BFLUTS scores between incon-tinent and conincon-tinent women (Table 1). Compared with the continent group, incontinent women had signifi-cantly higher BFLUTS scores (p < 0·001), indicating more severe complaints about urinary symptoms that mentioned in all subscales within the BFLUTS ques-tionnaire including filling voiding, incontinence symp-toms, impact on a woman’s sexual function and quality of life. Total BFLUTS scores and subscale scores by age groups in incontinent and continent group women were also shown in Figure 1.
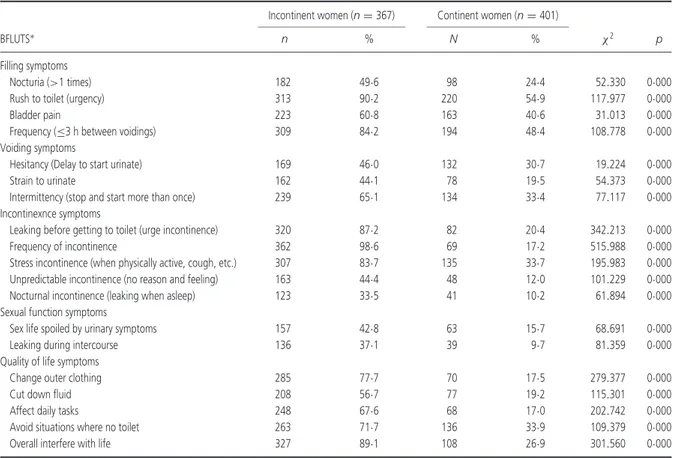
The frequency of BFLUTS among incontinent and continent women was evaluated for each symptom, according to each BFLUTS item in all subscales
(Table 2). Urinary complaints were found to be signifi-cantly more common among incontinent women. How-ever, many urinary symptoms were also seen among continent women and the frequency of these symp-toms, especially filling and voiding symptoms were considerably important. With the exception of incon-tinence, the most common symptoms in both groups were urgency, bladder pain, frequency, hesitancy and intermittency. The rate of women who reported a com-plaint about ‘overall interfere with life’ in any degree were 89·1% among incontinent women, while 26·9% of continent women reported this complaint.
The relationship between mean BFLUTS scores and other variables associated with urinary symptoms, including sociodemographical, obstetrical, gynecolog-ical/medical, lifestyle and incontinence history, were also assessed within the continent and incontinent women separately.
Age group, education level, marital status and employment status were not found to be associ-ated with the BFLUTS scores in both incontinent and continent groups (p > 0·05). BFLUTS scores of incon-tinent women demonstrated statistically significant
0 5 10 15 20 25 30
20–29 30–39 40–49 50–59 ≥60 All ages 20–29 30–39 40–49 50–59 ≥60 All ages
p u o r g t n e n i t n o c n I p u o r g t n e n i t n o C age groups B F LU TS s c o re
Filling Voiding Incontinence Sexual function Quality of life Total BFLUTS
Table 2 The frequency of BFLUTS among incontinent and continent women
Incontinent women (n= 367) Continent women (n= 401)
BFLUTS∗ n % N % χ2 p
Filling symptoms
Nocturia (>1 times) 182 49·6 98 24·4 52.330 0·000 Rush to toilet (urgency) 313 90·2 220 54·9 117.977 0·000 Bladder pain 223 60·8 163 40·6 31.013 0·000 Frequency (≤3 h between voidings) 309 84·2 194 48·4 108.778 0·000 Voiding symptoms
Hesitancy (Delay to start urinate) 169 46·0 132 30·7 19.224 0·000 Strain to urinate 162 44·1 78 19·5 54.373 0·000 Intermittency (stop and start more than once) 239 65·1 134 33·4 77.117 0·000 Incontinexnce symptoms
Leaking before getting to toilet (urge incontinence) 320 87·2 82 20·4 342.213 0·000 Frequency of incontinence 362 98·6 69 17·2 515.988 0·000 Stress incontinence (when physically active, cough, etc.) 307 83·7 135 33·7 195.983 0·000 Unpredictable incontinence (no reason and feeling) 163 44·4 48 12·0 101.229 0·000 Nocturnal incontinence (leaking when asleep) 123 33·5 41 10·2 61.894 0·000 Sexual function symptoms
Sex life spoiled by urinary symptoms 157 42·8 63 15·7 68.691 0·000 Leaking during intercourse 136 37·1 39 9·7 81.359 0·000 Quality of life symptoms
Change outer clothing 285 77·7 70 17·5 279.377 0·000 Cut down fluid 208 56·7 77 19·2 115.301 0·000 Affect daily tasks 248 67·6 68 17·0 202.742 0·000 Avoid situations where no toilet 263 71·7 136 33·9 109.379 0·000 Overall interfere with life 327 89·1 108 26·9 301.560 0·000 BFLUTS, Bristol Female Lower Urinary Tract Symptoms.
∗Responses for BFLUTS other than none/never were excepted as presence of the symptom in any degree of severity.
differences according to several obstetric variables including parity (p= 0·024), the number of pregnancy (p= 0·009), number of births (p = 0·035), vaginal birth with≥4 kg fetus (p = 0·003) and pregnancy with ≥4 kg fetus (p= 0·006). Incontinent women with a history of ≥4 pregnancy/birth had the highest total BFLUTS scores indicating more severe urinary symptoms. How-ever, there were no significant differences (p > 0·05) in BFLUTS scores among incontinent women in relation to number of vaginal birth, number of aborts, number of curettage, mode of the first delivery, place of first vaginal delivery, episiotomy in first vaginal delivery, fundal pressure in first vaginal delivery and perineal tears in first vaginal delivery. On the other hand, none of the obstetric variables showed a significant asso-ciation with BFLUTS scores among continent women (p > 0·05).
Assessment of gynecological/medical characteris-tics revealed that women with a history of recurrent vaginal infection, recurrent urinary infection and flatus had significantly higher BFLUTS scores (p < 0·05) in both incontinent and continent groups. Diabetes mel-litus, hypertension and haemorrhoid were found to be
associated with higher BFLUTS scores among conti-nent women, while pulmonary disease was the only sig-nificant medical condition that effected BFLUTS scores among incontinent women. Nevertheless, menopause, hormone replacement therapy, having gynaecologi-cal operation, medicine use, constipation, herniated disc / varicose veins and stria during pregnancy did not demonstrate a statistically significant difference in BFLUTS scores among both incontinent and continent women groups.
The relationship between BFLUTS scores and several lifestyle factors including smoking, caffeine consumption >2 cups/d, body mass index (BMI ≥25 kg/m2) and≥10 kg increase in body weight except pregnancy were evaluated. None of these factors were found to be associated with BFLUTS scores among continent women. However, being overweight and history of ≥10 kg increase in body weight were significantly associated with higher BFLUTS scores among incontinent women.
Personal and family history of incontinence includ-ing urinary incontinence in childhood, presence of fecal incontinence, history of incontinence in mother
Table 3 Total BFLUTS scores by several characteristics of women in incontinent and continent groups
Incontinent group (n= 367) Continent group (n= 401)
(N= 768) n % BFLUTS mean± SD p n % BFLUTS mean± SD p
Obstetric characteristics number of full term pregnancy
0 23 6·3 20·2 ± 10·1 KW= 13·545 75 18·7 8·8 ± 8·0 F= 0·495 1 41 11·2 27·7 ± 10·5 p= 0·009 63 15·7 8·1 ± 6·9 p= 0·739 2 111 30·2 25·4 ± 11·3 70 17·5 7·4 ± 6·4 3 101 27·5 25·3 ± 11·4 64 16·0 7·7 ± 6·4 ≥4 91 24·8 29·1 ± 11·6 129 32·2 7·5 ± 7·8 Parity Nulliparous 21 5·7 20·7 ± 10·3 z= −2·259 70 17·5 8·7 ± 8·0 t= 1·040 Parous 346 94·3 26·5 ± 11·4 p= 0·024 331 82·5 7·7 ± 7·1 p= 0·299 Number of births 0 21 5·7 20·7 ± 10·3 KW= 10·314 70 17·5 8·7 ± 8·0 F= 0·407 1 36 9·8 26·8 ± 11·0 p= 0·035 61 15·2 8·2 ± 7·1 p= 0·804 2 120 32·7 25·8 ± 11·1 74 18·5 7·8 ± 6·3 3 100 27·2 25·1 ± 11·2 65 16·2 7·4 ± 6·4 ≥ 4 90 24·5 29·0 ± 12·0 131 32·7 7·5 ± 7·8 Vaginal birth of≥4 kg fetus (n = 623)†
Yes 74 22·3 29·7 ± 11·6 t= −2·950 52 17·9 8·5 ± 8·3 t= −0·994
No 258 77·7 25·3 ± 11·3 p= 0·003 239 82·1 7·4 ± 6·6 p= 0·321
Pregnancy with≥4 kg fetus (n = 677)*
Yes 75 21·7 29·8 ± 11·5 t= −2·826 60 18·1 9·0 ± 8·6 t= −1·611 No 271 78·3 25·6 ± 11·2 p= 0·006 271 81·9 7·4 ± 6·6 p= 0·108 Medical characteristics Pulmonary disease Yes 38 10·4 29·9 ± 11·8 t= −2·105 19 4·7 10·7 ± 8·2 Z= −1·665 No 329 89·6 25·8 ± 11·3 p= 0·047 382 95·3 7·7 ± 7·2 p= 0·096 Diabetes mellitus Yes 49 13·4 26·9 ± 11·1 t= −0·475 25 6·2 10·5 ± 8·6 Z= −2·070 No 318 86·6 26·1 ± 11·5 p= 0·635 376 93·8 7·7 ± 7·1 p= 0·038 Hypertension Yes 113 30·8 27·8 ± 11·8 t= −1·832 93 23·2 9·6 ± 8·4 t= −2·629 No 254 69·2 25·5 ± 11·2 p= 0·068 308 76·8 7·3 ± 6·8 p= 0·009
Recurrent vaginal infection
Yes 87 23·7 28·5 ± 11·2 t= −2·105 99 24·7 9·8 ± 7·6 t= −3·171
No 280 76·3 25·5 ± 11·4 p= 0·036 302 75·3 7·2 ± 7·0 p= 0·002
Recurrent urinary infection
Yes 107 29·2 28·7 ± 11·7 t= −2·662 110 27·4 10·0 ± 8·4 t= −3·269 No 260 70·8 25·2 ± 11·2 p= 0·008 291 72·6 7·1 ± 6·6 p= 0·001 Flatus Yes 159 43·3 27·7 ± 11·4 t= −2·221 109 27·2 9·8 ± 7·6 t= −3·390 No 208 56·7 25·0 ± 11·3 p= 0·027 292 72·8 7·1 ± 7·0 p= 0·001 Haemorrhoid Yes 131 35·7 25·4 ± 11·3 t= 1·017 93 23·2 9·3 ± 7·5 t= −2·248 No 236 64·3 26·7 ± 11·5 p= 0·310 308 76·8 7·4 ± 7·1 p= 0·025 Lifestyle factors Body mass index
≥ 25 kg/m2 249 81·1 27·1 ± 11·5 t= −2·857 66 39·8 8·8 ± 8·0 t= −0·544
<25 kg/m2 58 18·9 22·4 ± 10·6 p= 0·005 100 60·2 8·2 ± 7·2 p= 0·587
≥ 10 kg increase in body weight except pregnancy
Yes 169 46·0 27·9 ± 11·9 t= −2·613 88 21·9 8·6 ± 7·6 t= −1·015
Table 3 continued
Incontinent group (n= 367) Continent group (n= 401)
(N= 768) n % BFLUTS mean± SD p n % BFLUTS mean± SD p
Family history Incontinence in mother
Yes 120 32·7 27·0 ± 12·1 t= −0·868 63 15·7 9·9 ± 8·1 t= −2·404
No 247 67·3 25·8 ± 11·1 p= 0·386 338 84·3 7·5 ± 7·0 p= 0·017
Incontinence in relatives (sister, aunt, etc.)
Yes 99 27·0 28·3 ± 12·6 t= −2·130 56 14·0 7·8 ± 7·6 t= 0·033
No 268 73·0 25·4 ± 10·9 p= 0·034 345 86·0 7·9 ± 7·2 p= 0·973
BFLUTS, Bristol Female Lower Urinary Tract Symptoms.
∗Among parous women.
†Among women who had at least one vaginal birth.
and history of incontinence in relatives (sister, aunt, etc.) were evaluated in relation to their effects on BFLUTS scores in both groups. Women with ‘a his-tory of incontinence in mother’ had higher BFLUTS scores in continent women group, while ‘history of incontinence in relatives’ had more significant effects on BFLUTS scores of incontinent women.
DISCUSSION
LUTS are the most common symptoms in women at all age groups worldwide, and their prevalence is increasing with age. LUTS have negative effects on women’s quality of life, especially on the medical, physical, social, psychological, economical and sexual aspects (Bilgic and Beji, 2010). In a study aiming to identify the effects of urinary incontinency on LUTS in Japanese women, Terai et al. (2004) collected data from 1634 women through International Prostate Symptom Score (IPSS) and International Consultation on Incontinence Questionnaire-Short Form (ICIQ-SF). They found that all scores of IPSS and ICIQ-SF were higher in women who had incontinence than those who did not. Findings of this study show that BFLUTS scores were higher in women who had incontinence, and the difference between women with incontinence and without incontinence was statistically significant (Table 1).
Women’s Health in the Lund Area conducted by Teleman et al. (2005) is reportedly a society-based study that aimed at identifying LUTS perception and prevalence in middle-aged women with and without incontinence. This study detected significant differ-ences in all BFLUTS items except for hesitancy and retention. This study detected significant differences between the two groups in all items (Table 2). Both this study and other studies in the literature (Teleman et al., 2005; Zhang et al., 2005) found that women without
incontinence also had urinary complaints, especially filling and voiding symptoms.
Many factors, such as age, childbirth, fecal difficul-ties, obstetric complications, obesity, pelvic surgery, medications, functional impairment, chronic diseases, menstrual cycle, race and family history, are associ-ated with urinary incontinence and other LUTS (Moller et al., 2000a). Studies show that LUTS increased with age (Moller et al., 2000b; Boyle et al., 2003; Terai et al., 2004; Teleman et al., 2005; Zhang et al., 2005; Irwin et al., 2006; Kupelian et al., 2006; Litman et al., 2007; Coyne et al., 2009). This study detected no difference between BFLUTS scores of women with and without incontinence in terms of age (Figure 1).
Zhang et al. (2005) investigated the LUTS preva-lence and associated risk factors in Chinese women who were 20 years old and over and detected LUTS prevalence as 37%. The study found menopause, parity >2, constipation, fetal birth weight and epi-siotomy as common potential risk factors for LUTS, voiding and filling symptoms. Higher BMI increased the occurrence of LUTS and storage symptoms, while caesarean delivery and labour protected against the development of filling symptoms. In their Boston Area Community Health study, Litman et al. (2007) con-ducted a randomized society-based research including men, women and three ethnic groups (Black, Hispanic and White). This study which aimed at identifying the relationship between LUTS and life changes and clinic factors found that there was no difference between ethnic groups, that physical activity decreased LUTS, there was a significant relationship between LUTS and cardiovascular diseases, urinary infections and depressive symptoms, no significant relationship was detected between increased BMI and diabetes, but BMI increase and diabetes caused an increase in LUTS. In their study conducted with 564 women aged between 40 and 60, Moller et al. (2000a) investigated
the factors associated with LUTS and found that LUTS were associated positively with parity, BMI, prior hys-terectomy, use of diuretics, straining at stool and constipation. This study detected that BFLUTS scores of the women with incontinence demonstrated signif-icant relationships with various obstetric parameters such as parity, the number of pregnancy, number of births, vaginal birth with ≥4 kg fetus and pregnancy with≥4 kg fetus. It was also found that women both with and incontinence and continence demonstrated significant relationships between high BFLUTS scores and recurrent vaginal infection, recurrent urinary infec-tion and flatus. Besides, significant relainfec-tionships were detected between diabetes, hypertension and haem-orrhoid in women without incontinence and between pulmonary diseases and higher BFLUTS scores in women with incontinence (Table 3).
CONCLUSION
LUTS with or without urinary incontinence complaints are common in Turkish women and have negative effects on quality of life. Increased parity, high birth weight, diabetes mellitus, hypertension, haemorrhoid, pulmonary disease, obesity and history of incontinence in mother were significantly associated with urinary complaints.
IMPLICATIONS FOR PRACTICE
Women must be encouraged to report their urinary problems while health care providers should raise the issue on routine exams in risk groups. To improve the current management of patients, education and awareness regarding LUTS, its causes and associated co-morbidities are needed. This is also essential for developing a policy of a preventive strategy to decrease these symptoms.
WHAT IS KNOWN ABOUT THIS TOPIC
• Although most women are aware of the more severe end of the spectrum of urinary symptoms and incontinence, there is a myriad of other symptoms that can affect the health-related quality of women’s life.
WHAT THIS PAPER ADDS
• LUTS are more common among incontinent women and they have more severe complaints. However, filling and voiding symptoms are also common among continent women.
• Recurrent infection and flatus are common factors associated with worse symptoms in both continent and incontinent women. • Diabetes, hypertension and haemorrhoid increase the severity of complaints among continent women, while increased parity, high birth
weight, pulmonary disease and overweight may have more negative effects among incontinent women.
REFERENCES
Beji NK, Ozbas A, Aslan E, Bilgic D, Ayyıldız HE. (2010). Overview of the social impact of urinary incontinence with a focus on Turkish women. Urologic Nursing; 30 (6): 327–335. Bilgic D, Beji NK. (2010). Lower urinary tract symptoms in women
and quality of life. International Journal of Urological Nursing; 4 (3): 97–105.
Boyle P, Robertson C, Mazzetta C, Keech M, Hobbs FDR, Four-cade R, Kiemeney L, Lee C. (2003). The prevalence of lower urinary tract symptoms in men and women in four centres.
The UrEpik Study. British Journal of Urology International; 92:
409–414.
Bradway C, Coyne KS, Irwin D, Kopp Z. (2008). Lower urinary tract symptoms in women-a common but neglected problem.
Journal of the American Academy of Nurse Practitioners; 20:
311–318.
Brookes ST, Donovan J, Wright M, Jackson S, Abrams P. (2004). A scored form of the Bristol Female Lower Urinary Tract symptom questionnaire: data from a randomized controlled trial of surgery for women with stress incontinence. American
Journal of Obstetrics & Gynecology; 191: 73–82.
Chapple CR, Wein AJ, Abrams P, Dmochowski RR, Giuliano F, Kaplan S, McVary KT, Roehrborn CG. (2008). Lower urinary
tract symptoms revisited: a broader clinical perspective.
European Urology; 54: 563–569.
Coyne KS, Sexton CC, Thompson CL, Milsom I, Irwin D, Kopp ZS, Chapple CR, Kaplan S, Tubaro A, Aiyer LP, Wein AJ. (2009). The prevalence of lower urinary tract symptoms (LUTS) in the USA, the UK and Sweden: results from Epidemiology of LUTS (EpiLUTS) study. British Journal of Urology International;
104: 352–360.
G ¨ung ¨or F, Yalc¸ın ¨O. (2005). Comparison of the Clinical and
Urodynamic Effects of TVT and TVT-O in the Treatment of Stress Urinary Incontinence. Unpublished PhD Thesis, Istanbul:
Istanbul Universities Institute of Health Sciences, Turkey. Irwin DE, Milsom I, Hunskaar S, Reilly K, Kopp Z, Herschorn S,
Coyne K, Kelleher C, Hampel C, Artibani W, Abrams P. (2006). Population-based survey of urinary incontinence, overactive bladder, and other lower urinary tract symptoms in five countries: results of EPIC study. European Urology; 50: 1306–1315.
Jackson S, Donovan J, Brookes S, Eckford S, Swithinbank L, Abrams P. (1996). The Bristol Female Lower Urinary Tract symptom questionnaire: development and psychometric testing. British Journal of Urology; 77: 805–812.
Kupelian V, Wei JT, O’Leary MP, Kusek JW, Litman HJ, Link CL, McKinlay JB. (2006). Prevalence of lower urinary tract
symptoms and effect on quality of life in racially and ethnically diverse random sample. The Boston Area Community Health (BACH) Survey. Archives of Internal Medicine; 166: 2381–2387. Litman HJ, Steers WD, Wei JT, Kupelian V, Link CL,
McKin-lay JB. (2007). Relationship of lifestyle and clinical factors to lower urinary tract symptoms: results from Boston Area Community Health Survey. Urology; 70: 916–921.
Milsom L. (2009). Lower urinary tract symptoms in women.
Current Opinion in Urology; 19: 337–341.
Moller LA, Lose G, Jorgensen T. (2000a). Risk factors for lower urinary tract symptoms in women 40 to 60 years of age.
Obstetrics & Gynecology; 96: 446–451.
Moller LA, Lose G, Jorgensen T. (2000b). The prevalence and bothersomeness of lower urinary tract symptoms in women 40-60 years of age. Acta Obstetricia et Gynecologica Scandinavica;
79: 298–305.
Norby B, Nordling J, Mortensen S. (2005). Lower urinary tract symptoms in the Danish population: a population-based study of symptom prevalence, health-care seeking behavior and prevalence of treatment in elderly males and females.
European Urology; 47: 817–823.
Ozdamar K. (2003). Biostatistic with SPSS, 5th edn. Turkey: Kaan Publication, Eskisehir (In Turkish).
Teleman P, Lidfeldt J, Nerbrand C, Samsiof G, Mattiasson A. (2005). Lower urinary tract symptoms in middleaged women - prevalence and attitude towards mild urinary incontinence. A community-based population study. Acta Obstetricia et
Gynecologica Scandinavica; 84: 1108–1112.
Terai A, Ueda N, Utsunomiya N, Kouhei N, Ichioka K, Yoshimura K. (2004). Effect of urinary incontinence on lower urinary tract symptoms in Japanese women. Urology; 64: 1139–1143.
Wennberg AL, Molander U, Fall M, Edlund C, Peeker R, Milsom I. (2009). A longitudinal population-based survey of urinary ıncontinence, overactive bladder, and other lower urinary tract symptoms in women. European Urology; 55: 783–791. Zhang W, Song Y, He X, Xu B, Huang H, He C, Hao L, Li Y.
(2005). Prevalence and risk factors of lower urinary tract symptoms in Fuzhou Chinese women. European Urology; 48: 309–313.