www.medicinescience.org | Med-Science 919
Comparison of Liquid Based Cytology Results with Conventional Cytology
Results in Screening Cervical Cancer
Nezaket Kadioglu1, Sibel Ozler2, Eda Gulmez3, Basak Gumus4, Ebru Aslan Patlakoglu5
1
Sereflikochisar State Hospital, Ankara, Turkey 2
Zekai Tahir Burak Women's Health Education and Research Hospital, Ankara, Turkey 3
Department of Gynecology, Medical Park, Usak, Turkey 4
Liv Hospital, Ankara, Turkey
5Department of Gynecology, Dumlupınar University, Kutahya, Turkey
Abstract
Our objective is to compare and evaluate the liquid based cytology (LBC) results with the conventional cytology (CC) results for cervical cancer. Cross sectional study. The results of 1531 women, applied to our outpatient clinic, for cervical cancer screening between the years 2012- 2015, were evaluated. We have applied liquid based cytology on 958 (62.6%) of the patients, and conventional cytology on 573 (37.4%) of the patients. Unsatisfactory smear results for examination were found to be significantly lower in LBC compared to CC (20.3% vs. 0.4%, p<0.001). Atypical squamous cells of undetermined significance (ASC-US) and atypical squamous cells, cannot exclude high-grade lesion (ASC-H) detection rates were significantly higher in LBC compared to CC (3% vs. 1.7%, p<0.001). Between the ages 18 to 35, ASC-US and ASC-H rates were also significantly higher in LBC, when compared to CC (5.2% vs. 1%, p<0.001). Even though ASC-US and ASC-H rates in patients aged 18 to 35 were higher than other groups, no significant difference was observed. Age was a significant risk factor in cervical epithelial anomalies (p<0.001). LBC was found to be a better method than CC for obtaining accurate results on cervical epithelial anomalies, in all ages.
Keywords: Liquid based cytology, conventional cytology, cervical cancer screening, smear test
(Rec.Date: Dec 29, 2015 Accept Date: Jan 19, 2016)
Corresponding Author: Sibel Ozler, Zekai Tahir Burak Women's Health Education and
Research Hospital, Ankara, Turkey
www.medicinescience.org | Med-Science 920
Introduction
Cervical cancer is the third caused of death amoung women, and squamous cell carcinomas (SSC), are the most common type of this group [1]. HPV 16 and 18 have a role in the ethiopathogenesis of the 70-75% of the cervical cancers [2]. Cervical cancer does not develop suddenly, but arise depending on precancerous cervical changes, throughout the years [3]. The incidence in Turkey is 4.2/100 000 [3]. Cervical cytological changes can be determined in premalignant or low grade stages with the help of the liquid based cytology (LBC) and conventional cytology (CC) methods. Screening programs can be used most effectively on cervical cancer than all other cancer types. Having easy, fast resulting, low budget, and reliable tests is reducing the incidence of cervical cancer. The incidence of cervical cancer is getting lower in the last 30 years depending on screening programs [4]. Results are evaluated according to Bethesta system. LBC has an increased rate of sensitivity in determining cervical changes [5-6]. 6.5% of the normal results obtained by using CC, were shown to be abnormal in LBC [6]. Furthermore in 24 meta-analysis, it has been shown that LBC provides more accurate results, and determines more sufficient materials than CC, on cervical epithelial anomalies in uterus [5].
According to Bethesta system, 5-10% of the ASC-US results are proceeding to cervical malignancy [7]. For the reason that HPV is seen in adolescents, it is important to determine cervical changes in early period and obtain sufficient material to increase the accuracy of cervical screening results.
Our objective in this study, is to compare LBC and CC methods, and also search malignancy risk factors, and see which method gives more accurate results, by evaluating LBC and CC results in age groups.
Material and Methods
Our study included 1531 women, aged 18 to 70, who were sexually active and applied for routine cervical cancer screening in our outpatient clinics, in the years 2012- 2015. We have applied liquid based cytology on 958 (62.6%) of the patients, and conventional cytology on 573 (37.4%) of the patients. These patients are homogenized by their age, body mass index (BMI), parity, and cigarette smoking.
www.medicinescience.org | Med-Science 921 Women having a history of gynecologic malignancy and pelvic radiation and previous suspicious cervical lesions or being in their menstrual cycle and being pregnant were not included in the study.
We generated informed consent forms and they were filled by the patients included in this study, and these forms with questions and answers were saved.
Samples were taken directly with cytobrush from cervical tissue, and washed in fixative solution for the LBC, and labeled with patient’s information, and sent to pathological laboratory in appropriate conditions. In conventional method, a special lam prepared for each patient. Cervical samples were spread on to lam as soon as they were taken, and stabilized on lam with fixative. Both LBC and CC smear samples were dyed with pap staining technique and Papanicolaou stain. Samples were evaluated according to Bethesta system by the pathologists [9]. Pap smear results were grouped as; normal, satisfactory (reactive changes, inflammation/ infection), unsatisfactory (squamous metaplasia, erosive smear) and atrophy. Epithelial anomalies were identified as; atypical squamous cells of undetermined significance (ASCUS), and atypical squamous cells, cannot exclude high-grade lesion (ASC-H). The screening test has been repeated by convantional method, which resultes inadequate or erosive. The screening test has been repeated by convantional methods, which resultes inadequate or erosive. In these womens has not been undetermined malignita. Women were led to the thertiery center who has been resulted insufficient the again screening tests.
Statistical Analyses
The obtained data were evaluated using visual (histograms, probability plots) and statistical methods (Kolmogorov-Simirnov/Shapiro-Wilk's test) to determine normal distribution. The cytological abnormalities detected with the chi-square test were utilized and p values were derived. Linear regression analyses were used to determine risk factors of ASC-US or more severe lesions. An overall 5% type-1 error was used to infer statistical significance. Statistical analyses were performed using the SPSS software version 17 (SPSS Inc. Chicago, USA, 2008).
www.medicinescience.org | Med-Science 922
Results
1531 patients were evaluated in this study, and LBC was applied on 958 (62.6%) of the patients, and CC on 573 (37.4%) of the patients. These patients were homogenized by their age, body mass index (BMI), number of births, and cigarette smoking. The average age in LBC group was 38.8 ± 12.2, and in CC group it is 39.6 ± 11.6 (Table 1).
Table 1. Demographic data between groups
Smear Type p value* Liquid Based (LBC) n=958 (62.6%) Conventional(CC) n=573 (37.4%) Age (year) 38.8±12.2 39.6±11.6 0.078 Smoking 142 (%14.8) 148 (%25.8) 0.872 Gravida (count) 2 [1 – 9] 3 [0 – 10] 0.447
BMI (body mass index) kg/m2
27.3±4.7 27.9±4.4 0.063
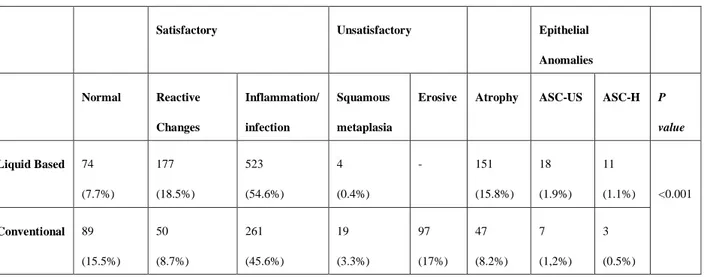
When smear results are compared between LBC and CC respectively; normal 74 (7.7%) / 89 (15.5%), squamous metaplasia 4 (0.4%)/19 (3.3%), and erosive 0 (0%)/97 (17%) smear results were less in LBC method (p<0.001). Reactive changes 177 (18.5%)/ 50 (8.7%), inflammation/infection 523(54.6%)/261(45.6%), atrophy 151 (15.8%)/47(8.2%), ASC-US 18(1.9%)/7(1.2%) and ASC-H 11(1.1%)/3(0.5%) smear results were significantly higher in LBC method (p<0.001) (Table 2).
Table 2. Evaluation of cervical smear results between LBC and CC using Bethesta system
Satisfactory Unsatisfactory Epithelial
Anomalies Normal Reactive Changes Inflammation/ infection Squamous metaplasia
Erosive Atrophy ASC-US ASC-H P value Liquid Based 74 (7.7%) 177 (18.5%) 523 (54.6%) 4 (0.4%) - 151 (15.8%) 18 (1.9%) 11 (1.1%) <0.001 Conventional 89 (15.5%) 50 (8.7%) 261 (45.6%) 19 (3.3%) 97 (17%) 47 (8.2%) 7 (1,2%) 3 (0.5%)
www.medicinescience.org | Med-Science 923 When cervical smear results were compared by age, following results were obtained: At the age group 18-25; normal and inflammation/infection results were lower, but reactive changes were higher in LBC when compared to CC (p<0.001). For ages between 25-35; normal, squamous metaplasia, and erosive results were less, but reactive changes and inflammation/infection indications were higher in LBC, compared to CC (p<0.001). For ages between 36-45; normal, squamous metaplasia, and erosive indications were lower, but reactive changes, inflammation/infection, and atrophy indications were higher in LBC compared to CC (p<0.001). For ages between 46-55; normal, squamous metaplasia, and erosive results were less; but normal, reactive changes, inflammation/infection, and atrophy results were higher in LBC compared to CC (p<0.001). For ages 56 and over; squamous metaplasia, and erosive results were lower, but normal, reactive changes, inflammation/infection, and atrophy indications were higher in LBC compared to CC (p<0.001). Also with LBC method, ASC-US and ASC-H smear result detecting rate was found to be higher than CC method in 25-35, 36-45, 46-55, and 56 and over age groups (p<0.001) (Table 3).
Age was the only risk factor in smear results evaluated as ASC-US and ASC-H in both LBC and CC methods (β=-0.160, p<0.001). Smoking and BMI were not a risk factor for ASC-US and ASC-H (Table 4).
www.medicinescience.org | Med-Science 924
Tablo 3. Comparison of Cervical Screening Results between Ages Groups
AGE GROUPS p value*
18-24 n=75 (4.9%) 25-35 n=408 (26.7%) 36-45 n=416 (27.2%) 46-55 n=409 (26.7%) ≥56 n=222(14.5%) Smoking 12 (%16) 69 (%16.9) 51 (%12.3) 31 (%7.6) 27 (%12.2) 0.002 Gravida 2 [0 – 6] 2 [0 – 9] 3 [0 – 9] 3 [0 – 9] 3 [1 – 10] <0.001 BMI 26.9±4.9 27.9±4.5 27.5±4.5 27.0±4.5 28.1±4.7 0.014 Smear result (LBC) Normal 3 (%9.1) 11 (%5.2) 23 (%9.5) 29 (%9.5) 8 (%4.8) <0.001 Reactive changes 11 (%33.3) 51 (%24.3) 51 (%21) 48 (%15.7) 16 (%9.6) Inflammation/infection 19 (%57.6) 135 (%64.3) 151 (%62.1) 169 (%55.4) 48 (%28.9) Squamous metaplasia - 1 (%0.5) 2 (%0.8) 1 (%0.3) - Erosive indications - - - - - Atrophy - 1 (%0.5) 4 (%1.6) 53 (%17.4) 93 (%56) ASC-US - 3 (%1.4) 9 (%3.7) 5 (%1.6) 1 (%0.6) ASC-H - 8 (%3.8) 3 (%1.2) - - Smear result (CC) Normal 11 (%26.2) 38 (%19.2) 27 (%15.6) 12 (%11.5) 1 (%1.8) <0.001 Reactive changes 1 (%2.4) 26 (%13.1) 14 (%8.1) 6 (%5.8) 3 (%5.4) Inflammation/infection 23 (%54.7) 102 (%51.5) 85 (%41.6) 40 (%38.5) 11 (%19.6) Squamous metaplasia - 4 (%2) 3 (%1.7) 36(%5.8) 6 (%9.7) Erosive indications 7 (%16.7) 25 (%12.6) 42 (%14.3) 19(%17.2) 4(%7.2) Atrophy - 1 (%0.5) - 15 (%14.4) 31 (%55.4) ASC-US - 1 (%0.5) 2 (%1.2) 4 (%3.8) - ASC-H - 1 (%0.5) - 2 (%1.9) -
Table 4. Linear Regression Analysis on factors that increase the risk of ASC-US and ASC-H
Unstandardized Coefficients Standardized Coefficients
t p value B Std. Error Beta Age -.007 .001 -.160 -6.296 <0.001 Smoking -.026 .025 -.026 -1.030 0.303 BMI -.003 .277 .000 -.011 0.991 Discussion
Cervical cancer is seen in 2.1%-2.2% of the women around the world and developing countries, 1.9% of the women in developed countries [7]. The incidence of cervical cancer has been decreased by the implementation of cervical cancer screening programs. Since the 1960 conventional smear (Pap smear) is being used in cancer screening and LBC method was started to be used after 1990. Besides cervical cytological changes, LBC and CC methods were used to determine bacterial, viral, and fungal infections [8]. The prevalence of abnormal smear results in Turkey is 1.8% - 2.8 % [9-10]. In our study, ASC-US and ASC-H determination rate was higher in LBC smear results when compared to CC, for all ages. Premalignant lesions those have the higher cervical lesion prevalence are ASC, Low grade
www.medicinescience.org | Med-Science 925 squamous intraepithelial lesion (LSIL), and High grade squamous intraepithelial lesion (HSIL) (10 %, 2%, and 0.5%). LBC method had higher accuracy in identifying lesions compared to CC [11]. ASCUS-LSIL Triage Study (ALTS) Group stated that LBC method is more sensitive at determining epithelial anomalies, LSIL and HSIL [12].
In our study, reactive changes and inflammation/infection results were the most common results determined in cervical smear evaluation. Unsatisfactory results which were evaluated as squamous metaplasia and erosive epithelium were determined less in LBC compared to CC for all ages. The reason for this might be that all the sample obtained in LBC was taken into thin prep fixative solution therefore exfoliative cell samples were plenty [13]. When Diaz-Rosario et al. compared the smear results of 56339 thin-prep, and 74756 CC in their study, they indicated that LSIL determining ratio was higher in thin-prep compared to CC, and it was related to the amount of sample [14]. Beerman et al. indicated in their studies with 35315 LBS, and 51154 CC, that unsatisfactory sample rate was significantly lower in LBC compared to CC [15]. Also lower unsatisfactory result rates in LBC compared to CC shows that LBC was more accurate. Williams reported that unsatisfactory smear results were decreasing significantly in LBC compared to CC [16].
Veena et al. showed that 46 % of the smear screening results were inflammatory results [17]. Taylor et al. compared the high-grade intraepithelial lesion and cancer (CIN+2) determining performance with LBC and CC methods in 5652 women between the ages 35-65 and have not done smear screening before, and they showed that in LBC, cervical premalignant and malignant lesions can be determined more accurately [6]. In our study, ASC-H and ASC-US rates were higher for the age group 25-35, compared to other age groups, when we evaluated in age groups in county population, and it has been shown that determination rate was higher in LBC, compared to CC. In these indications HPV infection rate was more in women who were sexually active at earlier ages. Yang et al. studied mortality rates according to cervical cancer in different places around the world, and they indicated that cervical cancer primarily affects young adult women [7].
Risk factors which cause cervical epithelial anomalies are; being sexually active at young ages, early age at marriage, giving birth, giving birth three or more times, anti-vegetarian diet, smoking, inappropriate heterosexual activities, and having resistant human papilloma virus
www.medicinescience.org | Med-Science 926 infection [18-19]. In our study, when both LBC and CC results were evaluated, early age is shown to be the only risk factor for cervical epithelial anomalies. Smoking, number of births given, and BMI were not significant risk factors. This shows that marriage at young ages and sexual activity can cause both higher rates of HPV infection at early ages, and the occurrence of cervical epithelial anomalies’.
Conclusion
Our similar results with the literature show that early age is a risk factor for cervical epithelial anomalies regardless of smear screening methods. Also when CC and LBC compared, unsatisfactory smear results are significantly decreased by LBC method. So we recommend the LBC method in screening cervical cancer, at least in the high risk groups like adolescents.
Conflicts of Interest
The authors have no conflicts of interest relevant to this article
References
1. Parkin DM, Bray F, Ferlay J, Pisani P. Global cancer statistics, 2002. CA Cancer J Clin. 2005;55(2):74-108.
2. Munoz N, Bosch FX, Castellsagué X, Díaz M, de Sanjose S, Hammouda D, Shah KV, Meijer CJ. Against which human papillomavirus types shall we vaccinate and screen? The international perspective. Int J Cancer. 2004;111(2):278-85.
3. Smith RA, Cokkinides V, Brawley OW. Cancer screening in the United States, 2009: a review of current American Cancer Society guidelines and issues in cancer screening. CA Cancer J Clin. 2009;59(1):27-41.
4. Gustafsson L, Ponten J, Bergstrom R, Adami HO. International incidence rates of invasive cervical cancer before cytological screening. Int J Cancer. 1997;71(2):159-65. 5. Bernstein SJ, Sanchez-Ramos L, Ndubisi B. Liquid-based cervical cytologic smear
study and conventional Papanicolaou smears: a metaanalysis of prospective studies comparing cytologic diagnosis and sample adequacy. Am J Obstet Gynecol. 2001;185(2):308-17.
6. Abulafia O, Pezzullo JC, Sherer DM. Performance of ThinPrep liquid-based cervical cytology in comparison with conventionally prepared Papanicolaou smears: a quantitative survey. Gynecol Oncol. 2003;90(1):137-44.
7. Yang BH, Bray FI, Parkin DM, Sellors JW, Zhang ZF. Cervical cancer as a priority for prevention in different world regions: an evaluation using years of life lost. Int J Cancer. 2004;109(3):418-24.
www.medicinescience.org | Med-Science 927 8. Solomon D, Davey D, Kurman R, Moriarty A, O'Connor D, Prey M, Raab S, Sherman
M, Wilbur D, Wright T Jr, Young N; The 2001 Bethesda System: terminology for reporting results of cervical cytology. JAMA. 2002; 287(16): 2114-9.
9. Turkish Cervical Cancer And Cervical Cytology Research Group (Ayhan A, Dursun P, Kuşçu E, Mülayim B, Haberal N, Ozen O, Kose MF, Turan AT, Ozgul N, Demir OF, Cavuşoğlu HD, Yuce K, Kuzey GM, Salman MC, Velipasaoglu M, Yenen MC, Dede M, Onan MA, Güner H, Taskiran C, Erdem O, Saraçoglu F, Serin S, Ozçelik B, Soyer I, Güzin K, Doğanyilmaz S, Kara F, Kiran G, Metindir J, Ozan H, Ozalp S, Vardar MA, Zeren H, Dilek S, Bozkaya H, Güven S, Ersöz S, Açikalin A, Meydanli M, Cetinarslan I, Gökaslan H, Eren F, Celik C, Yilmaz O, Celik H, Aksaz Z, Koçak C, Bağci H, Davutoğlu BS, Hakverdi AU, Soysal ME, Kaya G, Yanik A, Arici S, Cetin H, Mutlu AE, Kolusari A, Kosem M, Sahin G, Demirtürk F, Gültekin M, Karaca M, Harma M, Harma M, Batur S, Demirbag N, Baykal C, Doğan I, Sam AD). Prevalence of cervical cytological abnormalities in Turkey. Int J Gynaecol Obstet. 2009;106(3):206-9.
10. Atilgan R, Celik A, Boztosun A, Ilter E, Yalta T, Ozercan R. Evaluation of cervical cytological abnormalities in Turkish population. Indian J Pathol Microbiol. 2002;55(1):52-5.
11. Klinkhamer PJ, Meerding WJ, Rosier PF, Hanselaar AG. Liquid-based cervical cytology. Cancer. 2003;99(5):263-71.
12. ASCUS-LSIL Traige Study (ALTS) Group. A randomized trial on the management of low-grade squamous intraepithelial lesion cytology interpretations. Am J Obstet Gynecol. 2003;188(6):1393-400.
13. Berman ML. Advances in cervical cancer management from North American cooperative group clinical trials. Yonsei Med J. 2002;43(6):729-36.
14. Diaz-Rosario LA, Kabawat SE. Performance of a fluid-based, thin-layer papanicolaou smear method in the clinical setting of an independent laboratory and an outpatient screening population in New England. Arch Pathol Lab Med. 1999;123(9):817-21. 15. Beerman H, Van Dorst EB, Kuenen-Boumeester V, Hogendoorn PC. Superior
performance of liquid-based versus conventional cytology in a population-based cervical cancer screening program. Gynecol Oncol. 2009;112(3):572-6.
16. Williams AR. Liquid-based cytology and conventional smears compared over two 12-month periods. Cytopathology. 2006;17(2):82-5.
17. Kashyap V, Bhambhani S. Incidence and cytomorphological peculiarities of lower genital tract infections in vault (post hysterectomy) smears versus pap smears from non-hysterectomy subjects: a retrospective study. J Obstet Gynaecol India. 2001;61(5):558-61.
18. Juneja A, Sehgal A, Mitra AB, Pandey A. A survey on risk factors associated with cervical cancer. Indian J Cancer. 2003;40(1):15-22.
19. Reiter PL, Katz ML, Ferketich AK, Ruffin MTt, Paskett ED. Measuring cervical cancer risk: development and validation of the CARE Risky Sexual Behavior Index. Cancer Causes Control. 2009;20(10):1865-71.