Downloaded from http://journals.lww.com/plasreconsurg by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3i3D0OdRyi7TvSFl4Cf3VC4/OAVpDDa8KKGKV0Ymy+78= on 02/19/2021 Downloadedfrom http://journals.lww.com/plasreconsurgby BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3i3D0OdRyi7TvSFl4Cf3VC4/OAVpDDa8KKGKV0Ymy+78=on 02/19/2021
E
ver since its introduction by Taylor et al. in 1975,1 the vascularized fibular free flap has gained popularity; it has become the gold standard for reconstructing challenging bony defects of the head, neck, and extremities.2–4 Vascularized fibular flaps offer a great deal ofversatility, particularly when reconstructing bony defects larger than 6 cm.5 Successful transfer of a viable fibular growth plate together with variable lengths of the diaphysis, a procedure referred to as “vascularized epiphyseal transfer,” has allowed for new advances in the reconstruction of epiphyseal
Disclosure: None of the authors has a financial in-terest in any of the products or devices mentioned in this article.
Copyright © 2018 by the American Society of Plastic Surgeons DOI: 10.1097/PRS.0000000000005127
Mohamed Morsy, M.D. Yoo Joon Sur, M.D., Ph.D. Osman Akdag, M.D. M. Diya Sabbagh, M.D. Marissa A. Suchyta, B.A. Tarek A. El-Gammal, M.D. Nirusha Lachman, Ph.D. Steven L. Moran, M.D.
Rochester, Minn.; Assiut, Egypt; Uijeongbu, Republic of Korea; and Konya, Turkey
Background: Various vascular pedicles have been used to supply the proximal
fibula for vascularized epiphyseal transfer. The optimal pedicle has, however, not been agreed on. This study aimed to describe the detailed vascular anatomy of the proximal fibula to assist the surgeon in choosing the optimal pedicle.
Methods: Twenty-eight lower extremities were injected with latex or a mixture
of latex and barium sulfate. Vessels supplying the proximal fibula were identi-fied and dissected, and the course, diameter, anatomical relations, length, and branches were documented. In the barium group, high-resolution computed tomographic scanning was conducted before dissection. In seven specimens, branches of the deep peroneal nerve to the tibialis anterior muscle were care-fully preserved, and their relation to the proximal fibular vascularity was noted.
Results: An anastomotic vascular network supplied the proximal fibula. This
was formed superiorly by branches of the inferior lateral genicular artery, and inferiorly by branches of the anterior tibial artery, the most important of which were the first and second recurrent epiphyseal arteries. One or more deep peroneal nerve branches passed deep to the first recurrent epiphyseal artery in all specimens examined. In five specimens, all of the branches were superficial to the second recurrent epiphyseal artery, whereas two had branches deep to it.
Conclusions: The proximal fibula can be transferred using the inferior lateral
genicular or anterior tibial artery because of the existing anastomosis. Factors including length of pedicle, potential for nerve injury, and diaphyseal portion to be harvested should be considered in the pedicle choice. (Plast. Reconstr. Surg. 143: 172e, 2019.)
From the Division of Plastic Surgery, Department of Surgery, and the Department of Anatomy, Mayo Clinic; the Depart-ment of Orthopedic Surgery, Assiut University Hospital, Assiut University; the Department of Orthopedic Surgery, Uijeongbu St. Mary’s Hospital, College of Medicine, The Catholic University of Korea; and the Department of Plastic Reconstructive and Aesthetic Surgery, Selcuk University. Received for publication August 23, 2017; accepted June 6, 2018.
Presented in part at the 2017 American Society for Recon-structive Microsurgery Annual Meeting, in Waikoloa, Ha-waii, January 14 through 17, 2017.
Vascularity of the Proximal Fibula and Its
Implications in Vascularized Epiphyseal
Transfer: An Anatomical and High-Resolution
Computed Tomographic Angiography Study
Supplemental digital content is available for this article. A direct URL citation appears in the text; simply type the URL address into any Web browser to access this content. A clickable link to the material is provided in the HTML text of this article on the Journal’s website (www. PRSJournal.com).
SUPPLEMENTAL DIGITAL CONTENT IS AVAIL-ABLE IN THE TEXT.
defects in the pediatric population.3–9 In skeletally immature patients, vascularized epiphyseal trans-fer allows for reconstruction of complex bony defects preserving ongoing longitudinal growth, and provides a reliable articular surface for effec-tive joint function.5,9–11 In addition, in skeletally mature subjects, the proximal fibula has also been used to reconstruct bony defects and restore a functioning joint surface.12–21
Earlier reports of epiphyseal transfer described the use of the peroneal vessels as the pedicle. How-ever, the results were overall disappointing, and the peroneal artery alone was concluded to be insufficient to support the physeal growth plate.7 A bipedicled transfer, using the peroneal vessels to support the diaphysis and the anterior tibial ves-sels or the inferior lateral genicular vesves-sels to sup-port the epiphysis, was attempted.22,23 Although this showed better outcomes, it was technically more demanding and had a higher risk of compli-cations.22 Taylor et al. reported the use of the ante-rior tibial vessels as a single pedicle with success after confirming its role in the blood supply of the fibular diaphysis and epiphysis in a cadaveric study.4 Innocenti et al. further popularized the use of the anterior tibial pedicle after introducing the “reverse-flow” method and describing the harvest technique.24,25 A reported drawback for the use of the anterior tibial pedicle was the occasional need to transect branches of the deep peroneal nerve during the harvest because of their complex rela-tion to the vessels.26 To avoid this, Yang et al. have more recently reported the use of the inferior lat-eral genicular vessels successfully as a single pedi-cle in their case series.27
This variability in the vascular pedicle used mandated the need for a detailed anatomical study of the blood supply of the proximal fibula, including the head region and the supplying ves-sels, to give surgeons appropriate information for choosing the ideal vessel for these complex cases and minimizing donor-site morbidity. To the best of our knowledge, no study has described the ana-tomical relationship of the deep peroneal nerve branches to the tibialis anterior muscle and their relation to the supplying vessels. The purpose of this study was to provide an accurate description of the vascular anatomy of the proximal fibula, including the possible anatomical variations, and the anatomy of the terminal branches of the deep peroneal nerve relevant to the epiphyseal transfer harvest. This information will be critical to better plan and execute this technically demanding pro-cedure and ultimately improve outcomes.
MATERIALS AND METHODS
Twenty-eight fresh cadaveric lower extremi-ties were used for this study, after approval of the study design by our institutional review board biospecimen subcommittee. None of the extrem-ities had any known history of previous trauma or peripheral vascular disease or had undergone any previous surgery. Length of the extremities was measured from the anterior superior iliac spine to the medial malleolus. The femoral artery was identified proximally and cannulated, and the vascular tree was irrigated with normal saline until clear effluent was observed. Eleven lower extremities were injected with Ward’s red latex (Ward’s Science, Rochester, N.Y.), and 17 were injected with a mixture of latex and barium sul-fate. The barium sulfate was prepared as a sus-pension of powder in water at a ratio of 1:2 and then mixed with Ward’s red latex at a 1:2 ratio of the suspension and latex, respectively. After injec-tion, the lower extremities were left to cool at 4°C for 24 to 48 hours. In the first 21 specimens, a vertical incision was performed at the popliteal fossa, and the popliteal artery was dissected care-fully along its course distally, identifying and pre-serving all vessels contributing to the proximal fibular vascularity, including major vessels such as the inferior lateral genicular artery, the ante-rior tibial artery, the tibioperoneal trunk, the posterior tibial artery, and peroneal arteries; and any minor, small-caliber, or previously unidenti-fied vessels. These vessels in turn were followed, and the diameter at the origin, length, detailed course, branching pattern, and anatomical rela-tions were recorded. Each branch was further dissected and its diameter and distribution were recorded. In particular, branches to the fibula were dissected up to their terminal branching points on the fibular surface. These branches, their termination, and any anastomosis were recorded, photographed, and sketched to formu-late the vascular pattern supplying the proximal fibula. In the final seven specimens, an anterolat-eral skin incision was performed in the lower leg and extended proximally over the biceps tendon crossing the fibular head. The common and deep peroneal nerves and their branches were care-fully dissected up to their points of termination within the muscles, with attention to branches supplying the tibialis anterior muscle. The vascu-lar network was then dissected and described as mentioned above, with care taken to preserve the exposed nerves and with the number of muscu-lar branches and their relation to the vessels in
their distribution to the fibular head recorded. Dissection was conducted under 3.5× loupe mag-nification, and all measurements were recorded using an electronic digital caliper except for limb length, which was done using a measuring tape. All relevant steps of the dissection were photo-graphed using a digital camera.
The 17 specimens injected with the latex and barium sulfate mixture were scanned using a high-resolution computed tomography scan-ner (127 SOMATOM Definition FLASH; Siemens Healthcare, Forchheim, Germany). Three-dimen-sional reformats were created using Mimics soft-ware (Materialise, Leuven, Belgium) designed for three-dimensional rendering, finalized using 3-matic software (Materialise) and reviewed, and then used as a guide for the dissections that fol-lowed the above-stated protocol.
RESULTS
Twenty-eight lower extremities (eight male and 20 female) were used for this study, with 14 right and 14 left sides. All of the donors were of Caucasian descent with an average age of 77.2 years (range, 55 to 100 years). The average length of the lower extremities from the anterior supe-rior iliac spine to the medial malleolus was 85.8 cm
(range, 77 to 97 cm), and the average length of the fibula was 36.6 cm (range, 33 to 43 cm).
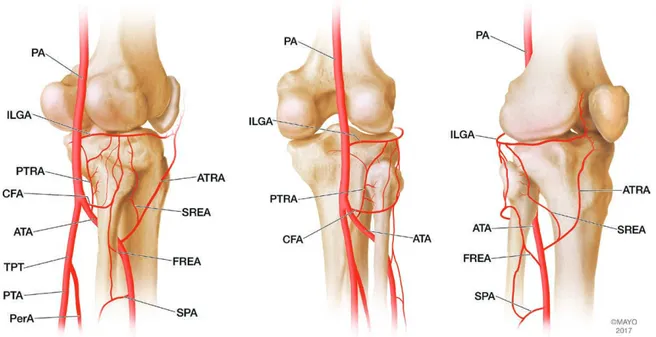
A rich anastomotic network was identified surrounding and supplying the fibular head in all specimens (Fig. 1). Six consistent vessels were present contributing to this anastomosis: the inferior lateral genicular artery, the circumflex fibular artery, the posterior tibial recurrent artery, the first recurrent epiphyseal artery, the second recurrent epiphyseal artery, and the superficial peroneal artery. See Table 1 for a summary of char-acteristics of these supplying vessels. The inferior lateral genicular artery originated from the popli-teal artery in all specimens except one, where the inferior lateral genicular artery originated from an aberrant anterior tibioperoneal trunk arising from a high bifurcating popliteal artery. The ori-gin was located at an average distance of 4.8 mm distal (range, 16 mm proximal to 31.9 mm distal) to the knee joint line. The inferior lateral genicu-lar artery had an average diameter at its origin of 1.5 mm (range, 1.1 to 2 mm) and coursed later-ally, superficial to the popliteus muscle and deep to the lateral head of the gastrocnemius and plantaris muscles. Superior to the fibular head, the inferior lateral genicular artery ran anteriorly between the biceps femoris muscle and the lateral
Fig. 1. Illustration of the most commonly occurring vascular pattern supplying the fibular head: posterolateral view
(left); posterior view (center); and anterolateral view (right). PA, popliteal artery; ATA, anterior tibial artery; TPT, tibio-peroneal trunk; PTA, posterior tibial artery; PerA, tibio-peroneal artery; ILGA, inferior lateral genicular artery; CFA, circumflex fibular artery; PTRA, posterior tibial recurrent artery; ATRA, anterior tibial recurrent artery; FREA, first recurrent epiphy-seal artery; SREA, second recurrent epiphyepiphy-seal artery; SPA, superficial peroneal artery. (Used with permission of Mayo Foundation for Medical Education and Research, all rights reserved.)
collateral ligament superficially and deep to the popliteus tendon and the knee joint capsule. An average of three (range, one to seven) branches to the fibular head were recorded. The inferior lateral genicular artery coursed further on the anterolateral aspect of the knee joint to end by
joining the anastomosis around the patella. The average length of the inferior lateral genicular artery to the first branch to the fibular head was 27.4 mm (range, 6.4 to 45.8 mm) (Fig. 2).
The circumflex fibular artery (also known as the artery of the neck) was present in 27 specimens
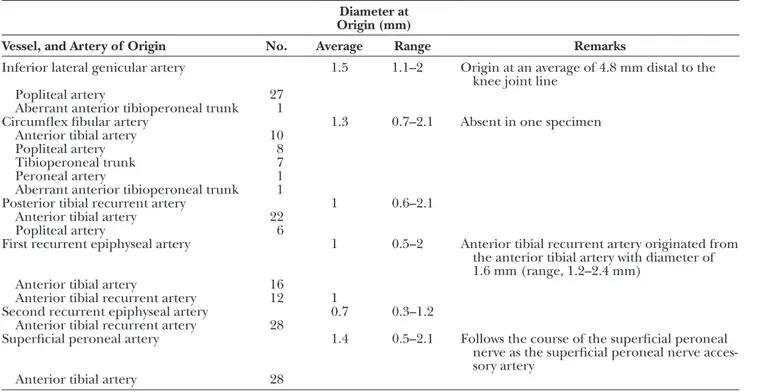
Table 1. Characteristics of the Vessels Supplying the Fibula
Diameter at Origin (mm)
Vessel, and Artery of Origin No. Average Range Remarks
Inferior lateral genicular artery 1.5 1.1–2 Origin at an average of 4.8 mm distal to the
knee joint line
Popliteal artery 27
Aberrant anterior tibioperoneal trunk 1
Circumflex fibular artery 1.3 0.7–2.1 Absent in one specimen
Anterior tibial artery 10
Popliteal artery 8
Tibioperoneal trunk 7
Peroneal artery 1
Aberrant anterior tibioperoneal trunk 1
Posterior tibial recurrent artery 1 0.6–2.1
Anterior tibial artery 22
Popliteal artery 6
First recurrent epiphyseal artery 1 0.5–2 Anterior tibial recurrent artery originated from
the anterior tibial artery with diameter of 1.6 mm (range, 1.2–2.4 mm)
Anterior tibial artery 16
Anterior tibial recurrent artery 12 1
Second recurrent epiphyseal artery 0.7 0.3–1.2
Anterior tibial recurrent artery 28
Superficial peroneal artery 1.4 0.5–2.1 Follows the course of the superficial peroneal
nerve as the superficial peroneal nerve acces-sory artery
Anterior tibial artery 28
Fig. 2. Origin, course, and branches of the inferior lateral genicular artery to the fibular
head in two left specimens. PA, popliteal artery; ATA, anterior tibial artery; TPT, tibiopero-neal trunk; ILGA, inferior lateral genicular artery; CFA, circumflex fibular artery.
and absent in one. The circumflex fibular artery showed variability in the artery of origin being the anterior tibial artery in 10 specimens, the popli-teal artery in eight specimens, the tibioperoneal trunk in seven, the peroneal artery in one, and the previously mentioned aberrant anterior tibiope-roneal trunk in one. The circumflex fibular artery had an average diameter at its origin of 1.3 mm (range, 0.7 to 2.1 mm). It courses laterally deep to the soleus muscle until it reaches the fibula, where it pierces the muscle at its point of attachment to run on the fibular surface at the level of the neck of the fibula, giving off a skin perforator and ter-minating by joining the anastomosis around the fibular head (Fig. 3).
The posterior tibial recurrent artery was pres-ent in all specimens and originated from the anterior tibial artery in 22 specimens and from the popliteal artery in six specimens. The aver-age diameter at its origin was 1 mm (range, 0.6 to 2.1 mm). The posterior tibial recurrent artery traveled superiorly on the posterior surface of the tibia, giving branches to the fibular head and ter-minating by anastomosing with branches from the inferior lateral genicular artery around the fibular head (Fig. 3).
The anterior tibial recurrent artery arose from the anterior tibial artery after crossing the
interosseous membrane to the anterolateral com-partment. The anterior tibial recurrent artery had an average diameter at its origin of 1.6 mm (range, 1.2 to 2.4 mm). It ascended proximally on the anterolateral surface of the tibia, giving branches to the underlying periosteum, the tibialis anterior muscle, the patellar tendon as it ascended lat-eral to it, and ending by joining the anastomosis around the patella (Fig. 4).
Two sizable arteries were consistently identi-fied ascending to supply the head of the fibula. For descriptive purposes, we named them the first and second recurrent epiphyseal arteries. The first is more lateral and is encountered first dur-ing proximal fibular harvest. The first recurrent epiphyseal artery originated from the anterior tibial artery in 16 specimens and from the ante-rior tibial recurrent artery in 12 specimens, with an average diameter at origin of 1 mm (range, 0.5 to 2 mm). It ascended deep to the extensor digitorum longus and peroneus longus muscles to reach the fibular head, giving branches to both muscles, fibular periosteum, and terminating by branches joining the anastomosis around the head of the fibula. The second recurrent epiph-yseal artery originated from the anterior tibial recurrent artery in all specimens, with an average diameter at its origin of 0.7 mm (range, 0.3 to
Fig. 3. Origin, course, and branches of the circumflex fibular artery and posterior tibial recurrent artery in three right specimens
showing variability in the origin of the circumflex fibular artery being from the anterior tibial artery (left), popliteal artery (center), or tibioperoneal trunk (right) in the shown specimens. The anastomoses between the inferior lateral genicular artery, circumflex fibular artery, and posterior tibial recurrent artery can be seen. ILGA, inferior lateral genicular artery; CFA, circumflex fibular artery; PTRA, posterior tibial recurrent artery.
Fig. 4. Origin, course, and branches of the first recurrent epiphyseal artery and
sec-ond recurrent epiphyseal artery in two left specimens. The two variations are shown with the first recurrent epiphyseal artery arising from the anterior tibial recurrent artery (left) and from the anterior tibial recurrent artery (right). ATA, anterior tibial artery; ATRA, anterior tibial recurrent artery; FREA, first recurrent epiphyseal artery; SREA, second recurrent epiphyseal artery; TA, tibialis anterior muscle.
Fig. 5. Two examples of the relation of the deep peroneal nerve branches to the tibialis
anterior muscle in two left specimens. One branch (blue arrow) runs deep to the first recur-rent epiphyseal artery and superficial to the second recurrecur-rent epiphyseal artery (left), two branches (blue arrows) run deep to the first recurrent epiphyseal artery, the second recurrent epiphyseal artery, and the anterior tibial recurrent artery (right). ATA, anterior tibial artery; ATRA, anterior tibial recurrent artery; FREA, first recurrent epiphyseal artery; SREA, second recurrent epiphyseal artery; CPN, common peroneal nerve; TA, tibialis anterior muscle.
1.2 mm). It ascended deep to the tibialis anterior and the extensor digitorum longus muscles, giv-ing branches to the fibular head and terminatgiv-ing by anastomosing with branches from the inferior lateral genicular artery to contribute to the anas-tomosis around the fibular head (Fig. 4).
The superficial peroneal artery originated from the anterior tibial artery at an average dis-tance of 47.1 mm (range, 25.8 to 121.5 mm) distal to the origin of the anterior tibial recurrent artery, with an average diameter at its origin of 1.4 mm (range, 0.5 to 2.1 mm). The superficial peroneal artery gave a minor ascending branch to supply the underlying fibular periosteum and contrib-uted to the anastomosis around the fibular head, muscular branches to the extensor digitorum lon-gus and peroneal muscles, then continued to fol-low the course of the superficial peroneal nerve as the superficial peroneal nerve accessory artery.
To determine the arterial diameter of the anterior tibial artery at the level where the pedicle is most commonly divided, the diameter of the anterior tibial artery was measured in all speci-mens distal to the origin of the superficial pero-neal artery. This diameter measured an average of 3.5 mm at this level (range, 2.3 to 5.5 mm). The point of pedicle division was on average 45.7 mm (range, 23.7 to 120.4 mm) from the origin of the anterior tibial artery from the popliteal artery.
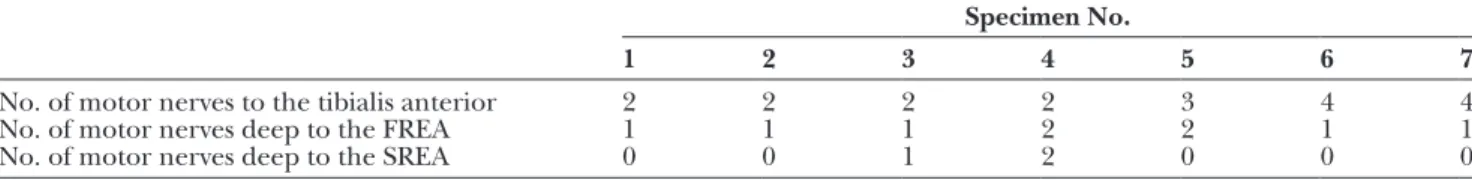
In the seven nerve-oriented dissections, the deep peroneal nerve was found to give an aver-age of 2.7 branches (range, two to four branches) to the tibialis anterior muscle. At least one major branch passed deep to the first recurrent epiph-yseal artery in all seven specimens (range, one to two branches). In five specimens, all of the branches were superficial to the second recurrent epiphyseal artery, one had one branch deep to the second recurrent epiphyseal artery, and one had two branches deep to the second recurrent epiph-yseal artery (Fig. 5). See Table 2 for details of each specimen. Figure 6 shows a simplified illustration of the variation in nerve and vessel relationship. Figure 7 demonstrates intraoperative photo-graphs from the harvest of the proximal fibula for
epiphyseal transfer showing dissection of the ves-sels to show the nerve and vessel relationship.
The three-dimensionally rendered high-reso-lution computed tomographic scans from the 17 specimens injected with the latex and barium sulfate mixture were studied before each dissection to guide the dissections and provide information on the undisturbed anatomy of the region. A reconstruction of the scan from a single specimen that represented an example of the most common vascular pattern is shown in Figure 8. (See Figure, Supplemental Digi-tal Content 1, which demonstrates the three-dimen-sional reconstruction of a high-resolution computed tomographic scan of one specimen showing the most commonly occurring vascular pattern in our study supplying the proximal fibula including the fibular head, http://links.lww.com/PRS/D207.)
Table 2. Number of Motor Nerves to the Tibialis Anterior Muscle from the Deep Peroneal Nerve and Their Relationship to the Recurrent Epiphyseal Arteries
Specimen No.
1 2 3 4 5 6 7
No. of motor nerves to the tibialis anterior 2 2 2 2 3 4 4
No. of motor nerves deep to the FREA 1 1 1 2 2 1 1
No. of motor nerves deep to the SREA 0 0 1 2 0 0 0
FREA, first recurrent epiphyseal artery; SREA, second recurrent epiphyseal artery.
Fig. 6. Variations in relationship between the motor nerves and
the first and second recurrent epiphyseal vessels. ATA, anterior tibial artery; ATRA, anterior tibial recurrent artery; CPN, common peroneal nerve; DPN, distal peroneal nerve; FREA, first recur-rent epiphyseal artery; ICGA, inferior lateral genicular artery; PA, popliteal artery; SPA, superficial peroneal artery; SPN, superficial peroneal nerve; SREA, second recurrent epiphyseal artery; TAMN, tibialis anterior motor nerve. (Used with permission of Mayo Foun-dation for Medical Education and Research. All rights reserved.)
DISCUSSION
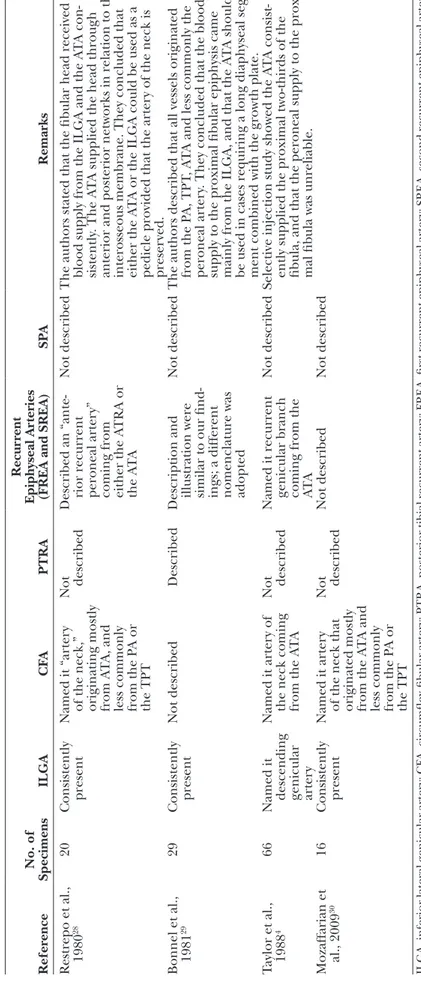
Vascularized transfer of the proximal fib-ula has been used for over three decades to reconstruct a lost growth plate in the skeletally immature subject and articular surfaces in the skeletally mature. This flap has produced mixed clinical results in part because of the complexity of preserving the arterial pedicle supplying the physis and epiphysis.4,7–10,12–24 Despite the fact that a number of anatomical studies have been per-formed to describe the vascularity of the proxi-mal fibula, a standard description of the detailed
vascular pattern around the fibular head does not appear to exist in the reviewed literature. Table 3 summarizes findings from previous anatomi-cal studies and compares them to our findings. Although most authors stressed the importance of preserving the artery of the fibular neck as it supplies the fibular head, descriptions of this artery are highly variable; some describe it to course lateral to the neck of the fibula, whereas others describe it to course medial to the neck of the fibula.4,28–30 In our study, we reported the presence of the artery of the neck in all but one Fig. 7. Intraoperative photographs of the harvest of the proximal fibula for epiphyseal
transfer. The anterior tibial vessels in the interval between the tibialis anterior and the extensor digitorum longus muscles crossed by motor nerves (blue arrows) (above, left); the first and second recurrent epiphyseal arteries and their relationship to the motor nerves (blue arrows) (above, right); and the inferior lateral genicular vessels coming from the pos-terior aspect originating from the popliteal vessels (below). AT, anpos-terior tibial vessels; FREA, first recurrent epiphyseal artery; SREA, second recurrent epiphyseal artery; ILG, inferior lateral genicular vessels; CPN, common peroneal nerve; TA, tibialis anterior muscle; EDL, extensor digitorum longus; P, peroneal muscle group; S, soleus muscle; MG, medial head of gastrocnemius.
specimen, and we preferred to name it the cir-cumflex fibular artery to avoid confusion. This artery was found to consistently course laterally around the neck of the fibula. The circumflex fibular artery had a variable origin where it came from the anterior tibial artery only in 10 speci-mens, which is in accordance with previous stud-ies. This makes us believe that preserving this artery as the main blood supply for epiphyseal transfer is not a good option.
In 1998, Innocenti et al. published their suc-cessful experience with epiphyseal transfer using the reverse-flow anterior tibial vessels. They based their flap on a preserved “recurrent epiphyseal artery” that was a direct branch from the anterior tibial artery, which they demonstrated in preoper-ative angiograms of their patients.24 In our study, two arteries ran in a retrograde direction toward the fibular head in all specimens. We named them the first and second recurrent epiphyseal arter-ies, from lateral to medial according to the order in which they would be encountered during the harvest procedure. The first recurrent epiphyseal artery had a wider diameter and originated from the anterior tibial artery in 16 specimens and from the anterior tibial recurrent artery in 12 speci-mens. The second recurrent epiphyseal artery had a smaller diameter and originated from the ante-rior tibial recurrent artery in all specimens. The relation of these two branches to the deep pero-neal nerve motor branches to the tibialis anterior are of critical importance, and careful dissection of these nerve branches must be undertaken,
especially in proximity to vessels to the fibular head. In some cases, a nerve branch may have to be divided then resutured to preserve the vascu-lar network and restore the tibialis anterior motor power, which is the case when the nerve branch runs deep to the vessel.4,22 In our dissections, the first recurrent epiphyseal artery had at least one major nerve branch running deep to it, whereas the second recurrent epiphyseal artery had one or two branches running deep to it in only two of seven specimens. These data could make the sec-ond recurrent epiphyseal artery more favorable to preserve than the first recurrent epiphyseal artery during epiphyseal harvest, although other fac-tors such as caliber and ease of dissection are to be considered too. We believe that both arteries should provide sufficient vascularity to the fibular head through the rich anastomotic network, and that it might be best to expose both arteries first and then assess the options on a case-by-case basis.
More recently, Yang et al. published a series of four patients with radial longitudinal deficiency who underwent successful proximal fibular epiph-yseal transfer based solely on the inferior lateral genicular artery.27 They reported an average arte-rial diameter of 1.06 mm (range, 0.75 to 1.14 mm) and an average pedicle length of 2.66 cm (range, 2.35 to 2.84 cm), which corroborates our results, where the inferior lateral genicular artery aver-age diameter was 1.5 mm and averaver-age length was 26.7 mm, with the consideration that their mea-surements were taken on pediatric patients. Fig. 8. Three-dimensional reconstruction of a high-resolution computed tomographic scan of one specimen demonstrating
the most commonly occurring vascular pattern supplying the fibular head. A pattern similar to this for the inferior lateral genicular artery was present in 96 percent of specimens, for the circumflex fibular artery in 36 percent of specimens, for the posterior tibial recurrent artery in 79 percent of specimens, for the first recurrent epiphyseal artery in 57 percent of speci-mens, and for the second recurrent epiphyseal artery and superficial peroneal artery in 100 percent of specimens. Posterior view (left), posterolateral view (center), and anterolateral view (right).
Table 3. P re vious Vascular A na tomic al S tudies in C omparison t o O ur F indings Refer ence No. of Specimens ILGA C FA PTRA Recur rent Epiphyseal Ar teries
(FREA and SREA)
SPA Remarks Restrepo et al., 1980 28 20 Consistently present Named it “arter y
of the neck,” originating mostly from A
T
A, and
less commonly from the P
A or
the TPT
Not described
Described an “ante
-rior recurrent peroneal arter
y”
coming from either the A
TRA or
the A
T
A
Not described
The authors stated that the fibular head received blood supply from the ILGA and the A
T A con -sistently . The A T
A supplied the head through
anterior and posterior networks in relation to the interosseous membrane. They concluded that either the A
T
A or the ILGA could be used as a
pedicle provided that the arter
y of the neck is preser ved. Bonnel et al., 1981 29 29 Consistently present Not described Described
Description and illustration were similar to our find
-ings; a different nomenclature was adopted
Not described
The authors described that all vessels originated from the P
A, TPT
, A
T
A and less commonly the
peroneal arter
y. They concluded that the blood
supply to the proximal fibular epiphysis came mainly from the ILGA, and that the A
T
A should
be used in cases requiring a long diaphyseal seg
-ment combined with the growth plate.
Taylor et al., 1988
4
66
Named it descending genicular arter
y
Named it arter
y of
the neck coming from the A
T
A
Not described Named it recurrent genicular branch coming from the ATA
Not described
Selective injection study showed the A
T
A consist
-ently supplied the proximal two-thirds of the fibula, and that the peroneal supply to the proxi
-mal fibula was unreliable.
Mozaffarian et al., 2009 30 16 Consistently present Named it arter y
of the neck that originated mostly from the A
T
A and
less commonly from the P
A or
the TPT
Not described
Not described
Not described
ILGA, inferior lateral genicular arter
y; CF
A, circumflex fibular arter
y; PTRA, posterior tibial recurrent arter
y; FREA, first recurrent epiphyseal arter
y; SREA, second recurrent epiphyseal arter
y;
SP
A, superficial peroneal arter
y; A
T
A, anterior tibial arter
y; A
TRA, anterior tibial recurrent arter
y; P
A, popliteal arter
y; TPT
According to the results of these patient series, and confirmed by our anatomical study, both the inferior lateral genicular artery and the reverse-flow anterior tibial artery could serve efficiently as the pedicle for proximal fibular epiphyseal transfer. Although using the inferior lateral genicular artery may be advantageous, as it is easy to dissect and avoids extensive manipulation of the deep peroneal nerve branches, the obvious disadvantages are its short pedicle and small diameter when one compares it to the reverse-flow anterior tibial artery pedicle, with a diameter in this study of greater than 3 mm. This size difference would be of particular importance in pediatric cases. The anterior tibial artery would also be a safer option when attempting to harvest a long portion of the diaphysis together with the epiphy-sis. See Table 4 for a comparison of the two arteries regarding pedicle use for epiphyseal transfer.
We acknowledge the limitations of this study in that specimens were those of adult subjects, which present some differences from the pediatric popula-tion on which the procedure is performed, includ-ing closure of the physeal plate. This limitation was present in all similar studies by previous authors and is most likely attributable to the limited avail-ability of pediatric specimens, as was the case in the current study. We believe that this does not pose a serious effect on our study because we studied only the extraosseous vascularity, which should be simi-lar in the pediatric and adult populations. As this is an injection study, another theoretical limitation could be the insufficient or nonuniform perfusion of the vessels in different specimens, which would lead to unreliable data. We do not believe this was a problem, as all of our specimens’ vascular trees were appropriately perfused up to the terminal branches and anastomoses. We believe the injection
technique was adequate for the purpose of the study. As a future recommendation, the authors are in favor of further studying the independent roles of the inferior lateral genicular artery and the anterior tibial artery in the vascularity of the fibular epiphysis and diaphysis, with a focus on the vascular territory of each and the intraosseous vascularity.
CONCLUSIONS
The fibular head is surrounded by a rich anastomotic network, formed mainly by the infe-rior lateral genicular artery and branches of the anterior tibial artery. Either of these vessels can be used successfully as the pedicle for vascularized epiphyseal transfer, although the anterior tibial artery would be preferred in cases where a longer length of the diaphysis is to be harvested or a lon-ger pedicle length is required.
Steven L. Moran, M.D.
Division of Plastic Surgery Department of Surgery Mayo Clinic 200 First Street SW Rochester, Minn. 55905 moran.steven@mayo.edu Twitter: @stevenmoranmd ACKNOWLEDGMENTS
The authors would like to acknowledge the noble generosity of the Mayo Clinic’s whole body donors, whose altruistic gift made this study possible. The authors would also like to thank the Department of Anatomy at Mayo Clinic, Rochester, Minnesota, for help in preparing the cadaveric specimens; the Mayo Clinic X-ray Imaging Core facility for extended support; and the Mayo Clinic three-dimensional anatomical modeling laboratory for invaluable assistance and support.
Table 4. Comparison between the Anterior Tibial Arteries and the Inferior Lateral Genicular Artery When Used as a Pedicle for Proximal Fibular Epiphyseal Transfer
Artery Anterior Tibial Artery Inferior Lateral Genicular Artery
Average diameter for
anasto-mosis 3.5 mm (range, 2.3 to 5.5 mm); this measurement is distal to the SPA, to give an idea of the diameter
dis-tal to the fibular head branches, which will be closer to the anastomosis site
1.5 mm (range, 1.1–2 mm)
Length as pedicle Long; virtually the entire length of the ATA from the
fibular head to the ankle joint can be harvested to be anastomosed in the reverse-flow pattern
Short; 27.4 mm (range, 6.4–45.8 mm); this is the length from the origin to the first branch to the fibular head
Consistency of anatomy Consistent in all specimens Consistent in all specimens
Ease of dissection Difficult dissection Easier dissection
Interference with motor
nerves One or more motor nerves to the tibialis anterior muscle cross its course and must be dissected or cut
and sutured back
No motor nerves crossing its course to be dissected or cut and sutured back
Blood supply to diaphysis The proximal two-thirds of the length of the fibula
can be supplied with the ATA according to Taylor et al.
Uncertain because no studies exist addressing this point
REFERENCES
1. Taylor GI, Miller GD, Ham FJ. The free vascularized bone graft: A clinical extension of microvascular techniques. Plast
Reconstr Surg. 1975;55:533–544.
2. Weiland AJ, Daniel RK. Microvascular anastomoses for bone grafts in the treatment of massive defects in bone. J Bone Joint
Surg Am. 1979;61:98–104.
3. Taylor GI, Corlett RJ, Ashton MW. The evolution of free vas-cularized bone transfer: A 40-year experience. Plast Reconstr
Surg. 2016;137:1292–1305.
4. Taylor GI, Wilson KR, Rees MD, Corlett RJ, Cole WG. The anterior tibial vessels and their role in epiphyseal and diaph-yseal transfer of the fibula: Experimental study and clinical applications. Br J Plast Surg. 1988;41:451–469.
5. Houdek MT, Wagner ER, Wyles CC, Nanos GP III, Moran SL. New options for vascularized bone reconstruction in the upper extremity. Semin Plast Surg. 2015;29:20–29.
6. Boyer MI, Bray PW, Bowen CV. Epiphyseal plate transplanta-tion: An historical review. Br J Plast Surg. 1994;47:563–569. 7. Innocenti M, Delcroix L, Romano GF, Capanna R.
Vascularized epiphyseal transplant. Orthop Clin North Am. 2007;38:95–101, vii.
8. Pho RW, Patterson MH, Kour AK, Kumar VP. Free vascula-rised epiphyseal transplantation in upper extremity recon-struction. J Hand Surg Br. 1988;13:440–447.
9. Erdmann D, Garcia RM, Blueschke G, Brigman BE, Levin LS. Vascularized fibula-based physis transfer for pediat-ric proximal humerus reconstruction. Plast Reconstr Surg. 2013;132:281e–287e.
10. Yang YF, Wang JW, Huang P, Xu ZH. Distal radius recon-struction with vascularized proximal fibular autograft after en-bloc resection of recurrent giant cell tumor. BMC
Musculoskelet Disord. 2016;17:346.
11. Innocenti M, Delcroix L, Balatri A. Vascularized growth plate transfer for distal radius reconstruction. Semin Plast Surg. 2008;22:186–194.
12. Rajacic N, Dashti H. Reconstruction of the lateral malleolus using a reverse-flow vascularized fibular head: A case report.
Microsurgery 1996;17:158–161.
13. Russell TA, Kumar A, Davidson RL, Klinar DF, Kuester DJ. Fibular head autograft: A salvage technique for severely com-minuted lateral fractures of the tibial plateau. Report of five cases. Am J Orthop (Belle Mead NJ) 1996;25:766–771.
14. Usui M, Murakami T, Naito T, Wada T, Takahashi T, Ishii S. Some problems in wrist reconstruction after tumor resec-tion with vascularized fibular-head graft. J Reconstr Microsurg. 1996;12:81–88.
15. de Gauzy JS, Kany J, Cahuzac JP. Distal fibular reconstruction with pedicled vascularized fibular head graft: A case report. J
Pediatr Orthop B 2002;11:176–180.
16. Wu SP, Zhang FH, Yu FB, Zhou R. Medial malleolus and del-toid ligament reconstruction in open ankle fractures with combination of vascularized fibular head osteo-tendinous flap and free flap transfers. Microsurgery 2009;29:630–635. 17. Ahmed SK, Fung BK, Ip WY, Chow SP. Lateral tibial
con-dyle reconstruction by pedicled vascularized fibular head graft: Long-term result. Strategies Trauma Limb Reconstr. 2011;6:163–166.
18. Onoda S, Sakuraba M, Asano T, et al. Use of vascularized free fibular head grafts for upper limb oncologic reconstruction.
Plast Reconstr Surg. 2011;127:1244–1253.
19. Chung DW, Han CS, Lee JH, Lee SG. Outcomes of wrist arthroplasty using a free vascularized fibular head graft for Enneking stage II giant cell tumors of the distal radius.
Microsurgery 2013;33:112–118.
20. Scaglioni MF, Chang EI, Gur E, et al. The role of the fibula head flap for joint reconstruction after osteoarticular resec-tions. J Plast Reconstr Aesthet Surg. 2014;67:617–623.
21. Ejiri S, Tajino T, Kawakami R, Hakozaki M, Konno S. Long-term follow-up of free vascularized fibular head graft for reconstruction of the proximal humerus after wide resection for bone sarcoma. Fukushima J Med Sci. 2015;61:58–65. 22. Innocenti M, Delcroix L, Manfrini M, Ceruso M, Capanna R.
Vascularized proximal fibular epiphyseal transfer for distal radial reconstruction. J Bone Joint Surg Am. 2004;86:1504–1511. 23. Tsai TM, Ludwig L, Tonkin M. Vascularized fibular
epiphyseal transfer: A clinical study. Clin Orthop Relat Res. 1986;210:228–234.
24. Innocenti M, Ceruso M, Manfrini M, et al. Free vascularized growth-plate transfer after bone tumor resection in children.
J Reconstr Microsurg. 1998;14:137–143.
25. Innocenti M, Delcroix L, Manfrini M, Ceruso M, Capanna R. Vascularized proximal fibular epiphyseal transfer for dis-tal radial reconstruction. J Bone Joint Surg Am. 2005;87(Suppl 1):237–246.
26. Innocenti M, Baldrighi C, Menichini G. Long term results of epiphyseal transplant in distal radius reconstruction in chil-dren. Handchir Mikrochir Plast Chir. 2015;47:83–89.
27. Yang J, Qin B, Li P, Fu G, Xiang J, Gu L. Vascularized proxi-mal fibular epiphyseal transfer for Bayne and Klug type III radial longitudinal deficiency in children. Plast Reconstr Surg. 2015;135:157e–166e.
28. Restrepo J, Katz D, Gilbert A. Arterial vascularization of the proximal epiphysis and the diaphysis of the fibula. Int J
Microsurg. 1980;2:49–54.
29. Bonnel F, Lesire M, Gomis R, Allieu Y, Rabischong P. Arterial vascularization of the fibula micro-surgical transplant tech-niques: Diaphysis-superior epiphysis. Anat Clin. 1981;3:13–22. 30. Mozaffarian K, Lascombes P, Dautel G. Vascular basis of free
transfer of proximal epiphysis and diaphysis of fibula: An ana-tomical study. Arch Orthop Trauma Surg. 2009;129:183–187.