ArchBronconeumol.2014;50(9):411–414
www . a r c h b r o n c o n e u m o l . o r g
Letters
to
the
Editor
PrimaryTrachealB-cellLymphomaCausing RecurrentCentralAirwayObstruction夽,夽夽
LinfomadecélulasBtraquealprimariocausantedeobstrucción recurrentedevíasaéreascentrales
TotheEditor:
Primarymalignanttumorsofthetracheaareveryuncommon, andcanoftenbeconfusedwithasthmaorchronicobstructive pul-monary disease(COPD). Trachealtumorsare veryrare,withan incidenceoflessthan0.01%;mostaresquamouscellcarcinomas.1
Veryfewcasesofprimarytracheallymphomacausingcentral air-wayobstructionhavebeendescribedtodate.2
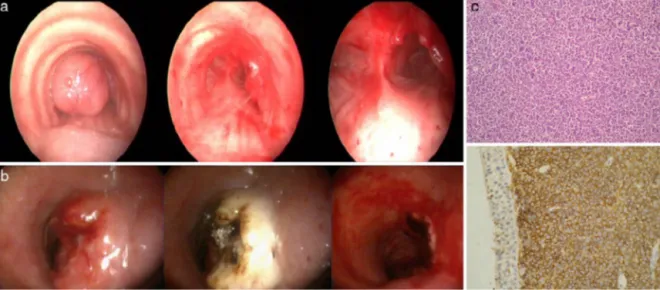
A72-year-oldmanwasadmittedwithdifficultybreathing.The patienthad beenmonitoredfora yearfollowing a diagnosisof COPD.Hehadan80packs/yearhistoryofsmoking.Physical exam-ination and laboratory tests were normal. On bronchoscopy, a smoothpolypoidmasswasobservedinthemiddleofthetrachea, almostcompletelyoccupyingthelumen.Adiodelaserandcoring wasusedtodebulkthetumor(Fig.1a).Pathologicalexamination revealedaB-celllymphoma.
The patient received the appropriate chemotherapy, but 20 monthsafterthefirstinterventionhewasreadmittedtohospital
Fig.1.(aandb)Bronchoscopyviewbeforeandaftertheinterventions.(c)ImmunohistochemicalstainingofatrachealtumorshowinglargeB-celllymphoma.
夽 Pleasecitethisarticleas:ÖnürST,DalarL,SökücüSN.LinfomadecélulasB
traquealprimariocausantedeobstrucciónrecurrentedevíasaéreascentrales.Arch
Bronconeumol.2014;50:411–412.
夽夽 ThismanuscriptwaspresentedattheEuropeanRespiratorySocietyAnnual
CongressinVienna2012,asaposterpresentation.
forstridoranddyspnea.Thepresenceofanothermassalmost com-pletelyobstructingtheupperthird ofthetracheawasobserved (Fig. 1b). Repeat interventional bronchoscopy was performed usingadiodelaser,andmechanicaldebulkingwasperformedto completelycleartheairwaylumen.
Pathologicalexaminationrevealedaroundcelltumor. Immuno-histochemical staining showed the presence of diffuse/strong CD20+,scantCD3+ and CD5+,anddisseminatedCD45+(Fig.1c). MacrocyticB-celllymphomawasthereforediagnosed.
Aroundtwo thirdsof all primary tracheal tumors are squa-mouscellcarcinomasoradenoidcysticcarcinomas.Theremaining third are malignant, intermediate or benign lesions.1 Primary
hematopoieticmalignantdiseasesofthetracheaareveryrare,and areobservedmorecommonlyincasesofextramedullary
plasmocy-tomaornon-Hodgkin’slymphoma.AsthmaandCOPDarecommon
erroneousdiagnoses.3InfactourpatienthadbeentreatedforCOPD
foroneyearpriortoadmission.
Thetreatmentofchoicedependsonthesizeofthelesion,and itmaybenecessarytoreconstructthelumenofthetumor-free trachea.Itshouldberememberedthatnon-Hodgkin’slymphomais rarelylimitedtothetracheainapatientpresentingcentralairway obstructioncausedbyanendoluminalmass.Airwayobstruction canrecurinanotherpartofthetrachea,despiteusingappropriate chemotherapy.
1579-2129/©2014SEPAR.PublishedbyElsevierEspaña,S.L.U.Allrightsreserved.
412 LetterstotheEditor/ArchBronconeumol.2014;50(9):411–414
Completeemergencyresectionofatumorinthetracheacanbe achievedwithrigidbronchoscopy.Inthiscase,theairway obstruc-tionoccurredontwo occasions20monthsapart.Thediagnosis wasobtainedusinganinterventionalbronchoscopyapproachwith rapidimprovement oftheconditionand openingof theairway lumenatthetimeofdiagnosis.
ConflictsofInterest
Theauthorsdeclarethattheyhavenoconflictsofinterest. References
1.GrilloHC,MatthisenDJ.Primarytrachealtumors:treatmentandresults.Ann ThoracSurg.1990;49:69–77.
2.DingJ,ChenZ,ShiM.Trachealstentingforprimarytrachealmucosa-associated lymphoidtissuelymphoma.EurJMedRes.2013;18:8.
3.TakamiA, OkumuraH,MaedaY,Kumano Y, AsakuraH,OdaM,etal. Pri-marytracheallymphoma: casereportand literaturereview.IntJHematol. 2005;82:338–42.
SedaTuralÖnür,aLeventDalar,b,∗SinemNedimeSökücüa
aYedikuleChestDiseasesandThoracicSurgery,Teaching andResearchHospital, ˙Istanbul,Turkey
bDepartmentofPulmonaryMedicine,SchoolofMedicine, ˙Istanbul BilimUniversity, ˙Istanbul,Turkey
∗Correspondingauthor.
E-mailaddresses:leventdalar@gmail.com,leventdalar@yahoo.com (L.Dalar).
DiffuseAlveolarHemorrhageasFirst ManifestationofaPheochromocytoma夽
Hemorragiaalveolardifusacomoprimeramanifestaciónclínica deunfeocromocitoma
TotheEditor:
Diffusealveolarhemorrhage(DAH)isaclinicalcondition char-acterizedbyhemoptysis, anemia and dyspnea.The radiological patternofthisdiseaseisdefinedbyground-glassconsolidations andinterlobularseptalthickening(crazy-pavingpattern).Causes are multiple and include malignancy, infections, autoimmune diseases,coagulopathiesandpulmonaryhypertension. Pheochro-mocytomaisatumorderivedfromchromaffincellsthattypically presentsasarterialhypertension(HT)associatedwith diaphore-sis,tachycardia andheadache. Wedescribe belowthecaseof a patientwhoseinitialclinicalmanifestationofpheochromocytoma wasmassivehemoptysisandacutecoronarysyndrome.Thiscase demonstratestheimportanceofconsideringpheochromocytoma asapossiblediagnosisincasesofDAHwithnoapparentcause.
A 68-year-old male was seen in the emergency room after
anepisodeoffrankhemoptysisassociatedwithoppressivechest pain,nausea,sweatingandpallor.Dyspnea,coldsweatsandpallor wereconfirmedonphysicalexamination.BP>180/100mmHg,HR 120bpm.TherewerenosignificantchangesonECGandbilateral diffuse alveolar pattern was observed on chest X-ray. Labora-torytest parameters ofnote includedblood glucose 257mg/dl, leukocytosiswithneutrophilia,hemoglobin14g/dl(MCVnormal), creatinine 1.19mg/dl, urea 62mg/dl, troponin T 596.6ng/l and CK186U/l.Arterialbloodgaseswerecompatiblewithhypoxemic respiratoryfailure(PaO251.4mmHg).Non-STsegmentelevation acutecoronarysyndromewithhemoptysiswassuspected,sothe patientwasadmittedtotheICUwheredoubleantiplatelet ther-apy was initiated but not anticoagulation, due to hemoptysis. The patient had another episode of frank hemoptysis associ-ated with a hypertensive crisis requiring oxygen therapy and intravenousbolusadministrationofmethylprednisolone.The clin-icalpictureimprovedwithinhourswithnormalizationof renal functionandanemia(Hb10.9g/dl).Whenthepatientwas inter-viewedagain, he reportedepisodes of headache, sweating and
夽 Please citethis article as:Querol RipollR, delOlmo García MI,Cámara
Gómez R, Merino-Torres JF. Hemorragia alveolardifusa como primera
man-ifestación clínica de un feocromocitoma. Arch Bronconeumol. 2014;50:412–
413.
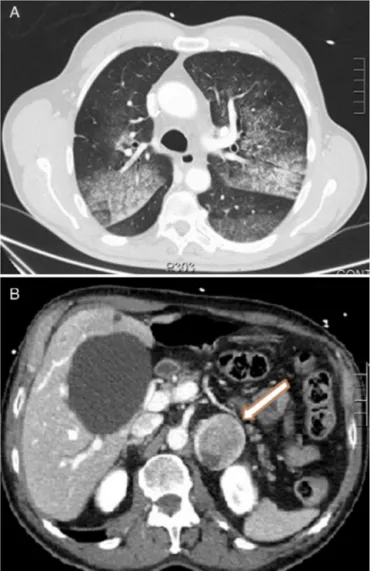
palpitations on performing Valsalva manoeuvers. CT showed a crazy-pavinglungpattern,ground-glassconsolidationsand inter-lobularseptal thickening,compatiblewithalveolarhemorrhage (Fig. 1A)and heterogeneousleft adrenallesion 46mm×40mm
(Fig. 1B). Raised catecholamine and metanephrine levels in
Fig.1.(A)CTaxialimageshowingcrazy-pavinglungpattern:ground-glass
consoli-dationsandinterlobularseptalthickening.(B)CTaxialimagewithcontrastmedium
showingheterogeneousleftadrenallesion,46mm×40mm.