Downloaded from https://journals.lww.com/intjrehabilres by BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3tIQ5gQCIeyxoHNtHYz46siWQ+R7s7imnRJ+LIMpDF/MfOCX5owmBhQ== on 07/30/2018 Downloadedfrom https://journals.lww.com/intjrehabilresby BhDMf5ePHKav1zEoum1tQfN4a+kJLhEZgbsIHo4XMi0hCywCX1AWnYQp/IlQrHD3tIQ5gQCIeyxoHNtHYz46siWQ+R7s7imnRJ+LIMpDF/MfOCX5owmBhQ==on 07/30/2018
Evaluation of disability in patients with degenerative
and inflammatory arthritis
Saime Ay
a, Birkan Sonel Tur
band Ay ¸se Ku¨c¸u¨kdeveci
bBoth degenerative and inflammatory arthritis cause disability that has deteriorative effect on patients’ daily activities. The aim of this study was to determine the disability level of patients with chronic degenerative and inflammatory arthritis and evaluate the relationship of different activities with disability. Sixty-three rheumatoid arthritis (RA) and 39 osteoarthritis (OA) patients who were hospitalized in our clinics to receive physical therapy and rehabilitation were included in this study. The patients were evaluated for severity of pain (Likert), functional stage (Steinbrocker), and physical disability (Stanford Health Assessment Questionnaire). The severity of pain was higher and functional stage was more advanced in the RA group (P < 0.05). Disability levels were mild in 38%, moderate in 44.5%, and severe in 16% of RA patients. In contrast, disability levels of OA patients were mild in 84.5% and moderate in 13%. The total disability score and the disability scores of activities, such as dressing, eating, hygiene, reaching for an object, and gripping an object were significantly higher in the RA group than in the OA group (P < 0.05). Disability in walking and rising were not different between the two groups (P > 0.05). Although the parameters that strongly correlated with general disability
were gripping, hygiene/grooming, running errands, and shopping in the RA group, they were walking, running errands, and shopping in the OA group. Degenerative arthritis can cause as much disability as inflammatory arthritis regarding activities related with lower extremity functions. Thus, while planning treatment these factors must be determined and an appropriate multidisciplinary rehabilitation process should be initiated. International Journal of Rehabilitation Research 31:159–163 c 2008
Wolters Kluwer Health | Lippincott Williams & Wilkins.
International Journal of Rehabilitation Research2008, 31:159–163 Keywords: daily activities, disability, osteoarthritis, rheumatoid arthritis
aDepartment of Physical Medicine and Rehabilitation, Ufuk University School of
Medicine andbDepartment of Physical Medicine and Rehabilitation,
Ankara University School of Medicine, Ankara, Turkey
Correspondence to Dr Saime Ay, MD, Department of Physical Medicine and Rehabilitation, Ufuk University School of Medicine Doctor Rıdvan Ege Hospital, 06520 Balgat-Ankara, Turkey
Tel: + 90 312 2044264; fax: + 90 312 2872390; e-mail: saimeay@yahoo.com
Received29 May 2007 Accepted 17 September 2007
Introduction
Physical disability is one of the main health problems in the adult population. According to the World Health Organization’s definition, a disability is any restriction or lack of ability to perform an activity in the manner or within the range considered normal for a human being. In other words, it is the restriction to perform routine daily life activities and it affects both physical and cognitive functions (Kirby, 1998; Song et al., 2006). The problems causing physical disability are mostly related to the musculoskeletal system. The most common diseases of the musculoskeletal system among degenerative and
inflammatory rheumatic disorders are osteoarthritis
(OA) and rheumatoid arthritis (RA), respectively
(Hawley and Wolfe, 1991). The ratio of RA/OA causing disability was determined as 1/7 in the USA (Bodley, 1995).
RA is an autoimmune disease characterized by diffuse and symmetric chronic inflammation of joints. The severity of the disease, degree of pain, and functional status all cause physical disability (O’Dell, 2001). The cartilage changes, loss of flexibility of subchondral bone, and neuromuscular changes facilitating the articular
degeneration in OA cause disability (Wylde et al., 2006). The disability in OA is related with pain and functional status. It has been shown that, even in patients with asymptomatic osteofit, functional loss and disability can develop in a few years (Spector et al., 1993).
Pain can be defined as unpleasant, emotional, and sensory experience accompanying tissue damage. Pain is the most serious problem causing patients to seek out medical help in both of these diseases. Articular pain is the main cause of disability that affects the daily activities of the patient (McDougall, 2006).
Although inflammatory arthritis is rare, it causes more disability by having more deteriorative effects on daily activities. Degenerative arthritis is more common, progresses slower compared with inflammatory arthritis, and has a better prognosis, but it causes as much disability as inflammatory arthritis (Soka et al., 2003, 2006).
This study was planned to determine the disability level in chronic degenerative and inflammatory arthritis patients and the relationship of different activities with daily activities.
Methods
Sixty-three RA and 39 OA patients who were diagnosed
according to American College of Rheumatology
criteria (Altman et al., 1986; Arnett et al., 1988) and hospitalized for physical therapy and rehabilitation in Ankara University Medical School Physical Medicine and Rehabilitation Clinics were included in this study. Among the osteoarthritic patients, 32 had gonarthrosis and seven had coxarthrosis. Moreover, eight of the patients had manual OA besides their gonarthrosis or coxarthrosis. Patients who had anatomic or traumatic problems causing secondary OA and who had neurological diseases that could cause disability were not included in this study. The age, sex, and duration of disease of the patients were recorded. Patients were evaluated regard-ing severity of pain, functional stage, and physical disability.
Pain, the most prominent symptom in patients, was evaluated by the five-point Likert pain scale (0–4; no, mild, moderate, severe, and worst pain).
The Functional classification was made according to Steinbrocker staging (stages 1–4) (Steinbrocker et al., 1949).
The Stanford Health Assessment Questionnaire Disabil-ity Index, which was proven valid for evaluating disabilDisabil-ity in RA and OA patients, was used (Fries et al., 1980; Pincus
et al., 1989; Ku¨cu¨kdeveci et al., 2004). The Stanford
Health Assessment Questionnaire is a short, easy to perform questionnaire that can be completed in 5–9 min. This disability scale includes eight subgroups evaluating dressing and grooming, rising, eating, walking, hygiene, reaching, and gripping activities. Each subgroup is scored as 0 (without any difficulty), 1 (with some difficulty), 2 (with much difficulty), and 3 (unable to do). The points obtained from each item are added and divided by the number of items, and the general disability score (0– 3) is obtained. On the basis of the information obtained from patients, the level of disability in various daily activities and the relationship of these activities with disability were evaluated.
Pearson’s test was used for correlation, and the Mann–
Whitney U-test and w2 test were used for statistical
comparison of parameters. The P level for significance was determined as 0.05.
Results
Of the 63 RA patients, 49 (77.7%) were women and of the 39 OA patients, 32 (82%) were women, and there was no statistically significant difference between groups regarding sex. The mean age was 48 ± 14.9 years and duration of disease was 9.2 ± 7.8 years (Table 1).
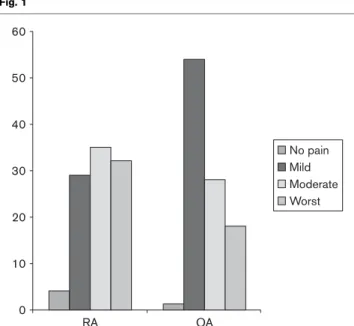
When pain of RA patients was evaluated, three patients (4%) had no pain, 18 patients (29%) had mild, 22 (35%) had moderate, and 20 patients (32%) had severe pain. Of OA patients, 21 (54%) had mild, 11 (28%) moderate, and seven (18%) had severe pain. The pain in the RA group
was significantly greater (P = 0.03, w2= 10.6) (Fig. 1).
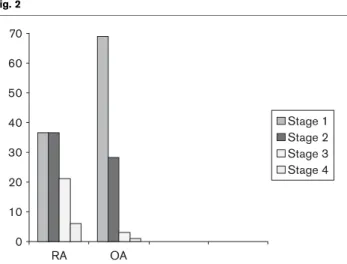
Functional staging of RA patients showed that 73% were in stage 1–2, whereas 97% of the patients from the OA group were in stage 1–2. The difference between groups
was statistically significant (P = 0.002, w2= 13.9) (Fig. 2).
The disability evaluation of the patients showed that in the RA group 38% of the patients had mild, 44.5% had moderate, and 16% had severe disability. On the other hand, of the patients in the OA group, 84.5% had mild and 13% had moderate disability. In the RA group, both total disability score and scores of dressing, eating, hygiene, reaching, and gripping activities were signifi-cantly higher than in the OA group (P < 0.05). Disability in walking and rising were not different between the two groups (P > 0.05). The parameters strongly correlated with disability were gripping, grooming, running errands, and shopping activities in the RA group. On the other hand, walking and running errands and shopping were the
Table 1 Demographic characteristics of patients
RA (n = 63) OA (n = 39) P Age (years) 48.4 ± 14.9 60.7 ± 8.7 < 0.05 Sex (% female) 77.7 82 NS Duration of disease (years) 9.2 ± 7.8 9.4 ± 6.9 NS NS, not significant; OA, osteoarthritis; RA, rheumatoid arthritis.
Fig. 1 60 50 40 30 20 10 0 RA OA No pain Mild Moderate Worst
Evaluation of pain (%) P < 0.05. RA, rheumatoid arthritis; OA, osteoarthritis.
parameters that were strongly correlated with disability in the OA group (Table 2).
Discussion
Degenerative and inflammatory arthritis are the most common articular diseases, which can cause disability and negatively affect the quality of life (Creamer et al., 2000; Croon et al., 2004).
RA is defined primarily as a synovial disease, as it mainly affects synovial joints and tendons. The most important factors contributing to the disability in RA are cartilage damage, bone damage, narrowing of the articular distance, increased intra-articular fluid volume, swelling of soft tissue around the joint, subluxations, and decreased articular mobility (Ferraz et al., 1990; Thyberg et al., 2005).
With increasing age, the incidence of OA increases and the articular pain caused by OA negatively affects the daily and social activities of the patients, and becomes
the main cause of physical and psychosocial disability. The mechanical and biological changes in the articular cartilage, intervertebral disk, tendon, ligament, and articular capsule with aging increase the susceptibility of these tissues to the disease and trauma. Experimental studies showed that the ability of the musculoskeletal system cells to perform special functions, synthesize matrix, and proliferate decreases with increasing age. OA, which develops because of this pathological process, is the main cause of disability. The joints affected by OA are thought to have special risk factors, which are related to the anatomy, biochemical, and physiologic characteristics of the joint. OA can develop in all synovial joints; however, knee, hand, hip, and articular process joints of the spine are the most commonly affected joints (Cushnaghan and Dieppe, 1991). The OA of lower extremities especially cause difficulty in performing daily activities by restricting articular movement, and causing weakness, pain, and deterioration of proprioception. This decreases the independence of the individual and causes inactivity and disability (Urwin et al., 1998). A correlation between the severity of pain and disability is observed. It was reported that the risk of disability in patients with knee pain is 1.5 times more than the patients without pain (McAlindon et al., 1993). Pain leads to avoiding physical activity, and in turn, this results in a decrease in muscle strength, which forms a vicious circle (Felson et al., 1987; Creamer et al., 2000).
RA is seen at a younger age than OA. The progress is more severe and it can cause disability in both lower and upper extremity functions. Although the onset of OA is at older ages, it is more common. Despite the fact that it has a better progress than RA, it causes disability more frequently. Degenerative arthritis causes as much dis-ability as inflammatory arthritis, especially in lower extremity functions (Soka et al., 2003, 2006).
A study comparing the disabilities of OA and RA patients reported that although walking and bending were the most affected functions, manual functions, gripping, and reaching were the least affected functions in OA patients. In our study, walking was the most deteriorated function in the OA group, but gripping, eating, and hygiene were not affected as much. In the above mentioned study, although the disability levels in functions such as reaching, gripping, and grooming were high, walking and rising activities were less affected in RA patients (Hakkinen et al., 2005), which was in accordance with the findings of our study.
The facts that upper extremity functions are more affected in RA and the pain score is higher are related to the number of swollen and tender upper extremity joints, decreased gripping force, decrease in muscle strength and endurance, and restricted ankle and shoulder movements. The effect on mobility is related
Fig. 2 70 60 50 40 30 20 10 0 RA OA Stage 1 Stage 2 Stage 3 Stage 4
Functional staging (%) P < 0.05. RA, rheumatoid arthritis; OA, osteoarthritis.
Table 2 Evaluation of disability (scores of subgroups of Stanford Disability Index) RA (n = 63) OA (n = 39) P value Dressing and grooming 1.1 ± 0.9 0.2 ± 0.4 < 0.001 Rising 0.8 ± 0.8 0.7 ± 0.6 NS Eating 1.2 ± 0.8 0.0 ± 0.2 < 0.001 Walking 1.0 ± 0.8 1.1 ± 0.6 NS Hygiene 1.2 ± 0.8 0.4 ± 0.3 < 0.001 Reach 1.1 ± 0.9 0.7 ± 0.6 < 0.001 Grip 1.4 ± 0.8 0.0 ± 0.1 < 0.001 Other (activities) 1.4 ± 1.0 1.0 ± 0.7 < 0.01 General 1.2 ± 0.8 0.5 ± 0.3 < 0.001 NS, not significant; OA, osteoarthritis; RA, rheumatoid arthritis.
to the involvement of knee and hip joints, pain, and the range of joint movement. As lower extremity involvement is more common in OA patients, the disability findings of lower extremities are greater (Badley et al., 1984; Hakkinen et al., 2005). The high prevalence of knee symptoms and radiographic knee osteoarthritis in the aged population shows that this disability is mainly because of knee osteoarthritis (Fries et al., 1980). Another study showed that knee and hip OA prevalence is high and suggested that disability is mainly related to knee OA. This study also showed that patients with knee and hip OA have more difficulty in performing daily activities than those without. The number of swollen and tender joints is correlated with disability in walking and daily activities. Functional restriction is not only related to the joint involvement but also to the joint’s range of motion (McAlindon et al., 1992). It is shown that disability increases with radiographic severity and pain, and osteofits are risk factors in asymptomatic patients for more functional loss and development of disability within a few years (Spector and Hart, 1992).
Although it is known that articular complaints are mostly related to OA, the detrimental effects of OA on daily activities are generally neglected and RA and other inflammatory arthropathies are accepted as the most important causes of physical disability (Song et al., 2006). In a study performed in the USA, the ratio of RA and OA causing disability is reported as 1/7 (Bodley, 1995). In this study, the general disability level is significantly higher in the RA group than the OA group. Lower and upper extremity disabilities are seen in both upper and lower extremities. Difficulty in gripping and reaching and difficulty in activities such as opening a jar lid can be seen in the OA group, but they are more common in the RA group. However, it should be kept in mind that patients with manual OA have decrease in gripping and muscle strength, and difficulty in performing upper extremity functions. This disability positively correlates with the activity of disease, pain, number of swollen and tender joints and laboratory tests reflecting the inflam-matory parameters. However, there is no significant difference between the two arthritis groups regarding disability in activities such as walking and rising. It has been shown that although mobility is the most affected parameter, manual abilities and reaching are less affected in OA patients (McAlindon et al., 1993). The disability score of patients with pain during passive joint move-ments, tender joints, decreased muscle strength, and instable ligaments is higher than the patients who do not have these symptoms (Ethgen et al., 2004).
Degenerative arthritis can cause as much disability as inflammatory arthritis regarding lower extremity func-tions. Thus, while planning the treatment strategies, determination of these factors and planning an appro-priate multidisciplinary rehabilitation process can help to
obtain a more effective response to treatment. We suggest an active treatment and rehabilitation program for both arthritis groups to decrease the disability level of patients.
References
Altman R, Asch E, Bloch D, Bole G, Borenstein D, Brandt K, et al. (1986). Development of criteria for the classification and reporting of osteo-arthritis: classification of osteoarthritis of the knee. Arthritis Rheum 29:1039–1049.
Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, et al. (1988). The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 31:315–324.
Badley E, Wagstaff S, Wood PH (1984). Measures of functional ability in arthritis in relation to impairment of range of joint movement. Ann Rheum Dis 43:563–569.
Bodley EM (1995). The effect of osteoarthritis on disability and health care use in Canada. J Rheumatol 32:19–22.
Creamer P, Letbridge-Cejku M, Hochberg MC (2000). Factors associated with functional impairment in symptomatic knee osteoarthritis. Rheumatology 39:490–496.
Croon EM, Sluiter JK, Nijssen TF, Dijkmans BA, Lankhorst GJ, Frings-Dresen MH (2004). Predictive factors of work disability in rheumatoid arthritis: a systematic literature review. Ann Rheum Dis 63:1362–1367.
Cushnaghan J, Dieppe PA (1991). Study of 500 patients with limb joint osteoarthritis analysis by age, sex and distribution of symptomatic joint sites. Ann Rheum Dis 50:8–13.
Ethgen O, Vanparijs P, Delhalle S, Rosant S, Bruyere O, Reginster JY (2004). Social support and health-related quality of life in hip and knee osteoarthritis. Qual Life Res 13:321–330.
Felson DT, Naimark A, Anderson T, Kazis L, Castelli W, Meenan RF (1987). The prevalence of knee osteoarthritis in the elderly: the Framingham osteoarthritis study. Arthritis Rheum 30:914–918.
Ferraz M, Oliveira L, Araujo P, Atra E, Walter SD (1990). EPM-ROM scale: an evaluative instrument to be used in rheumatoid arthritis trials. Clin Exp Rheumatol 8:491–494.
Fries JF, Spitz P, Kraines RG, Holman HR (1980). Measurement of patient outcome in arthritis. Arthritis Rheum 23:137–145.
Hakkinen A, Kautiainen H, Hannonen P, Ylinen J, Arkela-Kautiainen M, Sokka T (2005). Pain and joint mobility explain individual subdimensions of the health assessment questionnaire (HAQ) disability index in patients with rheumatoid arthritis. Ann Rheum Dis 64:59–63.
Hawley JD, Wolfe F (1991). Pain, disability, and pain/disability relationships in seven rheumatic disorders: a study of 1522 patients. J Rheumatol 18: 1552–1557.
Kirby RL (1998). Impairment, disability, and handicap. In: DeLisa JA, Gans BM, editors. Rehabilitation medicine, principles and practice. Philadelphia: Lipincott–Raven Publishers; pp. 55–60.
Ku¨cu¨kdeveci A, Sahin H, Ataman S, Griffiths B, Tennant A (2004). Issues in cross-cultural validity: example from the adaptation, reliability, and validity testing of a Turkish version of the Stanford Health Assessment Questionnaire. Arthritis Rheum 51:14–19.
McAlindon TE, Cooper C, Kirwan JR, Dieppe PA (1992). Knee pain and disability in the community. Br J Rheumatol 31:189–192.
McAlindon TE, Cooper C, Kirwan JR, Dieppe PA (1993). Determinants of disability in osteoarthritis of the knee. Ann Rheum Dis 52:258–262. McDougall JJ (2006). Arthritis and pain. Neurogenic origin of joint pain. Arthritis
Res Ther 10:220.
O’Dell JR (2001). Rheumatoid arthritis: the clinical picture. In: Koopman WJ, editor. Arthritis and allied conditions. Philadelphia: Lippincott Williams & Wilkins; pp. 1157–1186.
Pincus T, Callahan LF, Brooks RH, Fuchs HA, Olsen NJ, Kaye JJ (1989). Self-report questionnaire scores in rheumatoid arthritis compared with traditional physical, radiographic, and laboratory measures. Ann Intern Med 110: 259–266.
Soka T, Krishman E, Hakinken A, Hannonen P (2003). Functional disability in rheumatoid arthritis patients compared with a community population in Finland. Arthritis Rheum 48:59–63.
Soka T, Kautiainen H, Hannonen P, Pincus T (2006). Changes in Health Assessment Questionnaire disability scores over five years in patients with rheumatoid arthritis compared with the general population. Arthritis Rheum 54:3113–3118.
Song J, Rowland WC, Dunlop D (2006). Population impact of arthritis in older adults. Arthritis Rheum 55:248–255.
Spector TD, Hart DJ (1992). How serious is knee osteoarthritis? Ann Rheum Dis 51:1105–1106.
Spector TD, Hart DJ, Harris PA, Byrne J, Dacre JE, Doyle DV (1993). Definition of osteoarthritis of the knee for epidemiological studies. Ann Rheum Dis 52:790–794.
Steinbrocker O, Traeger CH, Batterman RC (1949). Therapeutic criteria rheumatoid arthritis. J Am Med Assoc 140:654–662.
Thyberg I, Hass UA, Gerdle B, Nordenskio¨ld U, Skogh T (2005). Activity limitation in rheumatoid arthritis correlates with reduced grip force
regardless of sex: the Swedish TIRA Project. Arthritis Rheum 53: 886–896.
Urwin M, Symmons D, Allison T, Brammah T, Busby H, Roxby M, Williams G (1998). Estimating the burden of musculoskeletal disorders in the community: the comparative prevalence of symptoms at different anatomical sites and the relation to social deprivation. Ann Rheum Dis 57:649–655.
Wylde V, Hewlett S, Learmonth ID, Cavendish VJ (2006). Personal impact of disability in osteoarthritis: patient, professional and public values. Musculo-skelet Care 4:152–166.