Giant hydatid lung cysts
Nurettin Karaoglanoglu
a,*, Ibrahim Can Kurkcuoglu
a, Metin Gorguner
b,
Atilla Eroglu
a, Atila Turkyilmaz
aaDepartment Of Thoracic Surgery, School of Medicine, AtatuÈrk University, Erzurum, Turkey bDepartment Of Chest Diseases, School of Medicine, AtatuÈrk University, Erzurum, Turkey
Received 17 October 2000; received in revised form 2 March 2001; accepted 16 March 2001
Abstract
Objective: In this clinical retrospective study, we aimed to evaluate giant hydatid lung cyst cases as a different clinical entity that recorded in last 10 years in our clinic. Methods: Between February 1990 and May 2000, a total of 305 hydatid lung cyst cases from patients that had been operated were reviewed, and 67 (21.9%) cysts with more than 10 cm in diameters of them were regarded as a giant hydatid lung cyst. Further investigations were made with respect to different factors. Results: Thirty-six (54%) cases were male and 31 (46%) were female. The ages ranged between 5 and 54 (mean 21.6) years. The most common symptoms recorded were; cough (68%), thoracic pain (55%) and dyspnea (52%). Cyst sizes were ranged between 10 and 22 cm (mean 13.4) in diameters. Forty-two (62%) of them were in the right, 22 (33%) were in the left hemithorax, and three (5%) were located bilaterally. Cystotomy or cystectomy and capitonnage was the most frequent applied operation procedure (71%). Resection was performed in nine (13%) cases. Thirteen (19%) cases had air leakage more than 10 days in which ®ve (7%) of them empyema occurred postoperatively. One case died due to respiratory failure in fourth postoperative day. The postoperative hospital stay ranged between 6 and 43 (mean 10.5) days. No recurrence was recorded in 1±5 years of a follow-up period. Conclusions: Giant hydatid lung cysts must be regarded as a different clinical entity because of their early occurrence, having more serious symptoms, with frequent operative complications, and they need prolonged care with higher cost effects. q 2001 Elsevier Science B.V. All rights reserved.
Keywords: Giant hydatid cyst; Lung; Treatment
1. Introduction
Echinococcosis is a parasitic disease frequently seen in sheep and cattle raising countries with poor sanitary condi-tions. The disease is encountered endemically in the Eastern and Southeastern region of Turkey [1].
Attaining giant sizes due to delays in treatment may complicate the clinical presentation, treatment and post-operative course of pulmonary hydatic disease. These hyda-tic cysts are called as `giant hydatid cyst' [2±4]. In such cases, postoperative complications due to destruction caused by the cyst also result in labor and economic loss. There are few investigations of giant hydatid cysts of the lung in literature [3,4]. For this reason, we aimed to evaluate giant hydatid lung cyst cases as a different clinical entity as recorded in last 10 years in our clinic.
2. Methods
We reviewed the charts of 305 cases that underwent operation for hydatid lung cysts in our department between February 1990 and May 2000 retrospectively. In all cases, both typical conventional and computerized radiological ®ndings, and indirect hemagglutination test for Echinococ-cosis were obtained in preoperative period. However, a de®-nite diagnosis was established pathologically in postoperative course (non-selected group). Because of their lack of speci®city, Casoni's intradermal test and Wein-berg complement ®xation test were not used.
Sixty-seven cases (21.9%) with more than 10-cm in diameter were regarded as a giant hydatid cyst (selected group). Cyst sizes were determined by means of conven-tional radiography, computerized tomography and intrao-perative ®ndings.
Further investigation was performed with respect to sex, age, family history, symptom, size, location, serology, type of operation, postoperative complication, mortality, dura-tion of hospitalizadura-tion and recurrence rate between the
European Journal of Cardio-thoracic Surgery 19 (2001) 914±917
1010-7940/01/$ - see front matter q 2001 Elsevier Science B.V. All rights reserved. PII: S1010-7940(01)00687-X
www.elsevier.com/locate/ejcts
* Corresponding author Tel.: 13166333/2149; fax: 1 90-442-3166340.
E-mail address: nkaraoglanoglu@hotmail.com (N. Karaoglanoglu).
selected and non-selected group. Our results were compared with available literature.
The statistical signi®cance between selected and non-selected groups was estimated using paired samples t-test. Correlation coef®cients were also estimated using Pearson's test.
3. Results
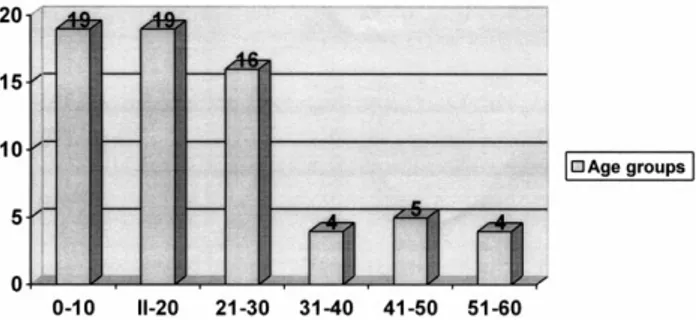
The 67 surgically con®rmed cases of giant hydatid lung cyst were presented. Among these cases, 36 (54%) were male and 31 (46%) were female. The ages were ranged between 5 and 54 (mean 21.6) years. The mean age was also found as 25.2 years in our non-selected group (P 0:5). Fig. 1 shows the age distribution of 67 cases. As shown, the majority of them were included in the ®rst three decades. Family history showed that one patient's mother had also been operated for hydatid cyst.
All of the cases were symptomatic in the giant hydatid lung cyst group. The most common symptoms were cough (68%), thoracic pain (55%) and dyspnea (52%) with respec-tively. Other symptoms were also fever, hydatoptysis that expectoration of germinative membrane or hydatid cyst, and hemoptysis (Fig. 2). On the other hand, only 13% of non-selected group were symptomatic (P 0:002).
Cyst sizes ranged between 10 and 22 cm (mean 13.4) in diameters. Forty-two (62%) of cases were in the right, 22 (33%) were in the left hemithorax, and three (5%) were located bilaterally. Eight patients had multiple cysts. The giant cysts were also located in lower lobe in 41 (61%) cases, in upper lobe in 26 (39%), and four (6%) in middle lobe. Four cases (6%) had also giant liver hydatid cysts.
Fig. 3 shows the computed tomographic appearance of the left giant hydatid lung cyst in a 5-year-old case.
All the cases received indirect hemagglutination test with 58 cases being positive (87%), and 11 cases having eosino-philia (16%).
Posterolateral thoracotomy was performed with a double-lumen endotracheal tube in all cases. To prevent contamina-tion, the pleura isolated with compresses soaked in povidon iodine. The applied operation types were; cystotomy and capitonnage (55%), cystectomy and capitonnage (16%), cystectomy and capitonnage and decortication (16%),
N. Karaoglanoglu et al. / European Journal of Cardio-thoracic Surgery 19 (2001) 914±917 915
Fig. 1. Age distribution of giant hydatid lung cyst cases.
Fig. 2. Symptoms of giant hydatid lung cyst cases.
Fig. 3. (A,B) Posterior±anterior and lateral radiograph of giant hydatid lung cyst. (C) The computed tomographic appearance of giant hydatid lung cyst a 5-year-old case.
segmentectomy (6%), lobectomy (4%), and bilobectomy superior (3%). Cystotomy or cystectomy and capitonnage (71%) was the most frequent applied operation procedure (Table 1). In nine (13%) cases resection was achieved due to presence of destroyed lung tissue. Resection rate was 9% (21/238) in non-selected group (P 0:46). In three cases with bilateral hydatid lung cysts, operation was accom-plished with contra-lateral thoracotomy in 21±31 days.
Thirteen (19%) cases had air leakage for more than 10 days in which ®ve (7%) of them empyema occurred operatively. One case received reoperation because of post-operative excessive bleeding. One case died due to respiratory failure in fourth postoperative day. The compli-cation rate was within 19% in selected, and 8.8% in non-selected group (P 0:017).
The postoperative hospital stay ranged between 6 and 43 (mean 10.5) days. It was 7.2 days in non-selected group (P 0:03). No recurrence was recorded in 1±5 years of a follow-up period.
Although, the size of the cysts was correlated with post-operative complications and hospital stay (P 0:021), there was no any correlation between the location of the cysts and postoperative complications or hospital stay (P 0:25). The age of patients was no correlated with postoperative complications and hospital stay (P 0:34). The type of operation performed was associated with complications. In cases applied resection, the complication rate was higher than the cases applied cystotomy or cystectomy and capi-tonnage (P 0:009).
If associated hepatic hydatid cyst is located on the diaphragmatic surface of the liver it is treated with trans-diaphragmatic approach in the same setting. Other cysts treated by percutaneous drainage if they were type 1 and 2 hydatid cysts according to Gharbi's description [5], and by laporotomy in a different setting if type 3 and 4 cysts [6]. 4. Discussion
Hydatid lung cysts may reach very large sizes due to relatively higher elasticity of the lung tissue compared with other tissues [2]. Symptom free course of the disease in same cases and poor socioeconomic conditions prevent the necessary treatment and operation until the cysts reach a very large size. The term of `giant hydatid cyst' has been
used since the treatment of these cysts require different treatment and operative techniques compared to other smal-ler cysts [3,4].
There is no generally accepted size to de®ne exterior diameter of cyst as `giant' [3,4]. In our study, the cyst with more than 10-cm in diameter were regarded as a giant hydatid lung cyst.
The phenomenon is known to occur more often in young males [2,7±9]. The lung tissue and immune system of the host in children and the adolescent allows the rapid growth of cyst and hence giant hydatid cysts are more commonly seen at these ages [2,4]. But, we could not ®nd statistical signi®cance for the mean age between our selected and non-selected groups.
The symptoms of cases with hydatid lung cyst include; thoracic pain, dyspnea, hemoptysis, fatigue, allergic reac-tions and hydatoptysis [3,7±11]. However, cases of no symptom development could be as high as ranging between 5 and 45% [7±9]. All of the cases were symptomatic in our giant hydatid lung cyst group. Whereas only 13% of non-selected group were symptomatic, and it was statistically very signi®cant. As the size of cyst increases dyspnea, thor-acic pain and hydatoptysis are more frequently encountered [3]. Other symptoms may be present in children with giant hydatid cyst that are not seen in adults. Thoracic deforma-tion was reported in other studies [2]. We have established expanded hemitorax in two cases and growth retardation in eight cases.
The location of the cysts was mainly in the right and lower lobes as reported in the literature [2,7±9,12]. Our results were similar to the general literature knowledge.
Diagnostic dif®culties are not experienced especially in non-complicated cases in our country since the disease is endemic. The most important diagnostic tool is radiology [3,10±14]. Chest X-ray and computerized thoracic tomo-graphy are generally suf®cient for diagnosis. However, a de®nite diagnosis was based on pathological con®rmation. On the other hand, the most commonly carried out serolo-gical test for diagnosis of hydatid disease was indirect hemagglutination test in our clinic. Casoni's intradermal test and Weinberg complement ®xation test were not routi-nely used because of their high rates of false positive results [14].
In treatment of hydatid lung cyst, the operation proce-dures protecting lung parenchyma are more frequently preferred [2,3,9]. Resection of the lung must be avoided for two reasons; the compressed lung parenchyma is gener-ally healthy and should be expanded postoperatively, and the second reason is the possibility of recurrence of hydatid cyst. Lobectomy procedure must be performed when the complications such as suppuration, pulmonary ®brosis and bronchiectasis consuming more than 50% of one lobe [2]. Although the reasons are very well-known, the resection rates are not low in different studies; 4.3% in 149 cases by Ayuso [8], 12% in 807 cases by Qian [10], 48.3% in 331 cases by Burgos [12]. All of these studies include hydatid
N. Karaoglanoglu et al. / European Journal of Cardio-thoracic Surgery 19 (2001) 914±917 916
Table 1
The operation types of giant hydatid lung cyst cases
Operation type %
Cystotomy and capitonnage 55 Cystectomy and capitonnage 16 Cystectomy and capitonnage and decortication 16
Segmentectomy 6
Lobectomy 4
cyst cases other than giant hydatid cysts in general. Hale-zeroglu and colleagues [3] also reported as 6% of pulmon-ary resection rate in their giant hydatid cysts of the lung. In our study, resection rate was 13% in giant hydatid lung cyst group, and 9% in non-selected group, and it was statistically non-signi®cant.
Single lung ventilation and posterolateral thoracotomy were performed in all cases. Cystotomy or cystectomy and capitonnage was the most commonly applied operation procedure. Enucleation procedure was not used our cases because of the risk of rupture. In the cases with bilateral involvement, median sternotomy procedure may be successfully used [15]. In our three cases with bilateral hydatid disease, however, posterolateral thoracotomy was accomplished following two different operations due to larger cyst size and posterior location.
Postoperative complications are in¯uenced by the size and number of cysts and the type of operation. The compli-cation rates were reported between 12.9 and 19% in litera-ture [3,5,8,11]. In our study, the complication rate was within 19% in selected group, and there was a statistical signi®cance between selected and non-selected groups. The size of the cysts was correlated with postoperative complications and hospital stay. However, there was no correlation between the location of the cysts or the age of patients and postoperative complications or hospital stay. In cases of applied resection, on the other hand, the complica-tion rate was higher than the cases applied cystotomy or cystectomy and capitonnage.
In literature, successful results of medical treatment were shown [16,17]. But we suggest that medical treatment should be performed in only inoperable cases due to cardiac and/or pulmonary performance status or in preventing post-operative recurrences. No inoperable case was present in our study and in all of our cases. For prophylactic purpose, we used Albendasole at 10 mg/kg per day for 1±3 months in postoperative period.
Mortality and recurrence rates of hydatid lung cysts are very low in literature [2,3,7,18]. Similarly, no recurrence occurred in our cases and only one patient died postopera-tively.
In conclusion, giant hydatid lung cysts must be regarded as a different clinical entity because of their early occur-rence, more serious symptoms, with frequent operative complications, and the need for prolonged care with higher costs.
References
[1] Ministry of Health, Department of Therapy. Statistical yearbook of directory of state hospitals 1989, Ankara: Ministry of Health, 1990. p. 83.
[2] Symbas PN, Aletras H. Hydatid disease of the lung. In: Shields TW, editor. General thoracic surgery. Philadelphia: Williams and Wilkins, 1994. pp. 1021±1031.
[3] Halezeroglu S, Celik M, Uysal A, Senol C, Keles M, Arman B. Giant hydatid cysts of the lung. J Thorac Cardiovasc Surg 1997;113:712± 717.
[4] Lamy AL, Cameron BH, LeBlanc JG, Culham JA, Blair GK, Taylor GP. Giant hydatid lung cysts in the Canadian northwest: outcome of conservative treatment in three children. J Pediatr Surg 1993;28:1140±1143.
[5] Balik AA, Basoglu M, Celebi F, Oren D, Polat KY, Atamanalp SS, Akcay MN. Surgical treatment of hydatid disease of the liver: review of 304 cases. Arch Surg 1999;134:166±169.
[6] Gharbi HA, Hassine W, Brauner MW, Dupuch K. Ultrasound exam-ination of the hydatid liver. Radiology 1981;139:459±463. [7] Wolcott MW, Harris SH, Briggs JN, Dobell AR, Brown RK. Hydatid
disease of the lung. J Thorac Cardiovasc Surg 1971;62:465±469. [8] Ayuso LA, de Peralta GT, Lazaro RB, Stein AJ, Sanchez JA, Aymerich
DF. Surgical treatment of pulmonary hydatidosis. J Thorac Cardio-vasc Surg 1981;82:569±575.
[9] Dogan R, Yuksel M, Cetin G, Suzer K, Alp M, Kaya S, Unlu M, Moldibi B. Surgical treatment of hydatid cysts of the lung: reports on 1055 patients. Thorax 1989;44:192±199.
[10] Qian Z. Thoracic hydatid cysts: a report of 842 cases treated over a thirty-year period. Ann Thorac Surg 1988;46:342±346.
[11] Aytac A, Yurdakul Y, Ikizler C, Olga R, Saylam A. Pulmonary hyda-tid disease. Report of 100 patients. Ann Thorac Surg 1977;23:145± 151.
[12] Burgos L, Baquerizo A, Munoz W, de Aretxabala X, Solar C, Fonseca L. Experience in the surgical treatment of 331 patients with pulmon-ary hydatidosis. J Thorac Cardiovasc Surg 1991;102:427±430. [13] Salih OK, Topcuoglu MS, Celik SK, Ulus T, Tokcan A. Surgical
treatment of hydatid cysts of the lung: analysis of 405 patients. Can J Surg 1998;41:131±135.
[14] Aletras H, Symbas PN. Hydatid disease of the lung. In: Shields TW, LoCicero III J, Ponn RB, editors. General thoracic surgery. Philadel-phia, PA: Lippincott Williams and Wilkins, 2000. pp. 1113±1122. [15] Cetin G, Dogan R, Yuksel M, Alp M, Ucanok K, Kaya S, Unlu M.
Surgical treatment of bilateral hydatid disease of the lung via median sternotomy: experience in 60 consecutive patients. J Thorac Cardio-vasc Surg 1988;36:114±117.
[16] Gil-Grande LA, Boixeda D, Garcia-Hoz F, Barcena R, Lledo A, Suarez E, Pascasio JM, Moreira V. Treatment of liver hydatid disease with mebendazole: a prospective study of thirteen cases. Am J Gastro-enterol 1983;78:584±588.
[17] Morris DL, Dykes PW, Marriner S, Bogan J, Burrows F, Skeene-Smith H, Clarkson MJ. Albendazole: objective evidence of response in human hydatid disease. J Am Med Assoc 1985;253:2053±2057. [18] Saidi F. Surgery of hydatid disease. Philadelphia, PA: W.B. Saunders
Company, 1976. p. 156.
N. Karaoglanoglu et al. / European Journal of Cardio-thoracic Surgery 19 (2001) 914±917 917